J Korean Neurosurg Soc.
2022 Nov;65(6):834-840. 10.3340/jkns.2022.0126.
Comparison of Inflammatory Markers Changes in Patients Who Used Postoperative Prophylactic Antibiotics within 24 Hours after Spine Surgery and 5 Days after Spine Surgery
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Medical Center, Kyung Hee University College of Medicine, Seoul, Korea
- KMID: 2535843
- DOI: http://doi.org/10.3340/jkns.2022.0126
Abstract
Objective
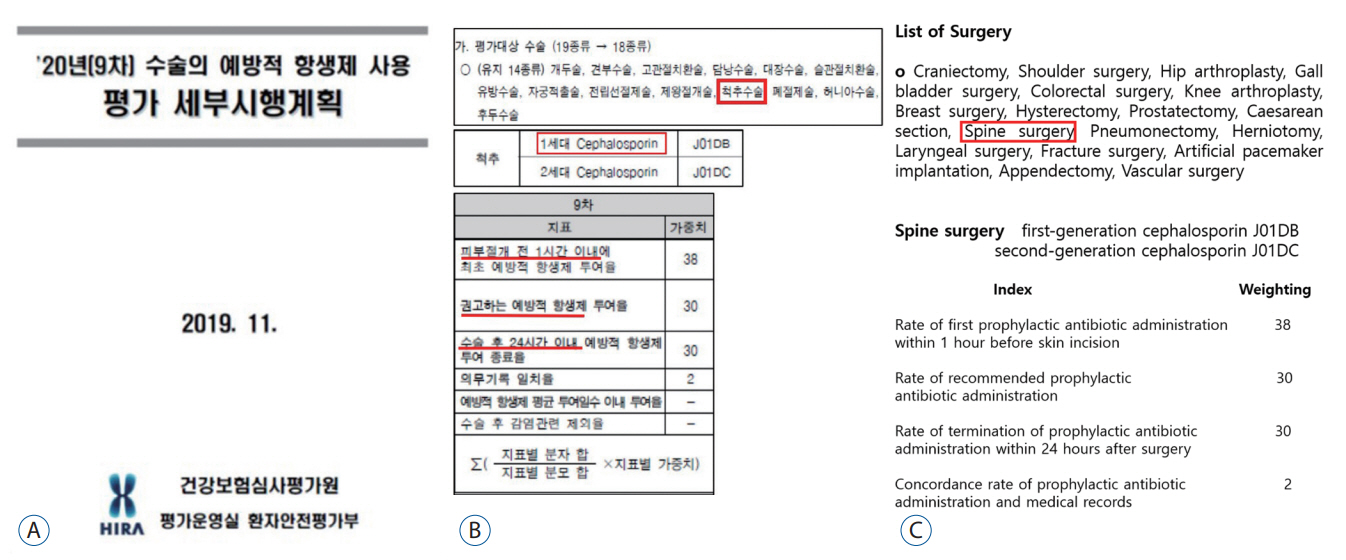
: C-reactive protein (CRP) level, erythrocyte sedimentation rate (ESR), and white blood cell (WBC) count are inflammatory markers used to evaluate postoperative infections. Although these markers are non-specific, understanding their normal kinetics after surgery may be helpful in the early detection of postoperative infections. To compliment the recent trend of reducing the duration of antibiotic use, this retrospective study investigated the inflammatory markers of patients who had received antibiotics within 24 hours after surgery according to the Health Insurance Review & Assessment Service guidelines and compared them with those of patients who had received antibiotics for 5 days, which was proven to be non-infectious.
Methods
: We enrolled 74 patients, divided into two groups. Patients underwent posterior lumbar interbody fusion (PLIF) at a single institution between 2019 and 2020. Group A included 37 patients who received antibiotics within 24 hours after the PLIF procedure, and group B comprised 37 patients who had used antibiotics for 5 days. A 1 : 1 nearest-neighbor propensity-matched analysis was used. The clinical variables included age, sex, medical history, body mass index, estimated blood loss, and operation time. Laboratory data included CRP, ESR, and WBC, which were measured preoperatively and on postoperative days (POD) 1, 3, 5, and 7.
Results
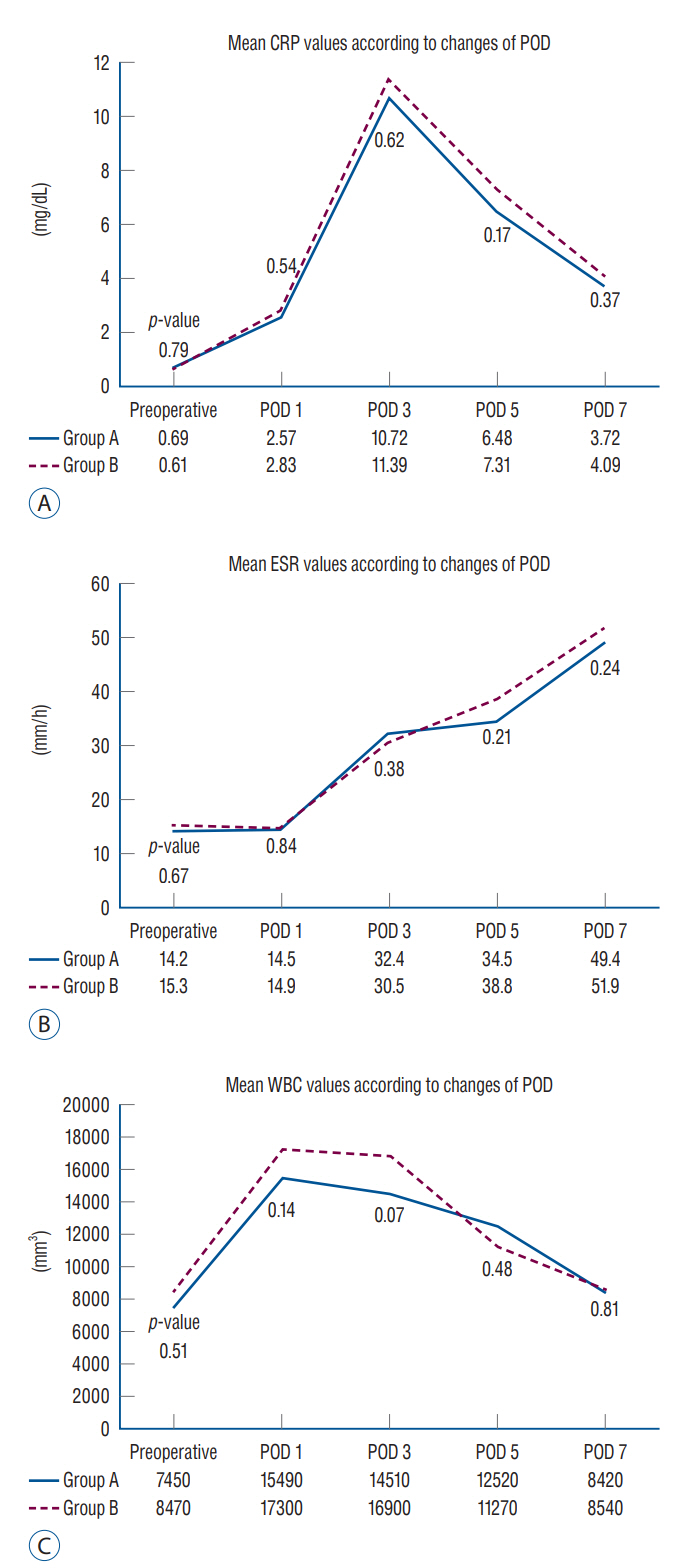
: CRP dynamics tended to decrease after peaking on POD 3, with a similar trend in both groups. The average CRP level in group B was slightly higher than that in group A; however, the difference was not statistically significant. Multiple linear regression analysis revealed operation time, number of fused levels, and estimated blood loss as significant predictors of a greater CRP peak value (r²=0.473, p<0.001) in patients. No trend (a tendency to decrease from the peak value) could be determined for ESR and WBC count on POD 7.
Conclusion
: Although slight differences were observed in numerical values and kinetics, sequential changes in inflammatory markers according to the duration of antibiotic administration showed similar patterns. Knowledge of CRP kinetics allows the assessment of the degree of difference between the clinical and expected values.
Figure
Reference
-
References
1. Black S, Kushner I, Samols D. C-reactive protein. J Biol Chem. 279:48487–48490. 2004.2. Burke JP. Maximizing appropriate antibiotic prophylaxis for surgical patients: an update from LDS Hospital, Salt Lake City. Clin Infect Dis 33 Suppl. 2:S78–S83. 2001.3. Cha HG, Kwon JG, Han HH, Eom JS, Kim EK. Appropriate prophylactic antibiotic use in clean wound surgery under local anesthesia. J Korean Med Sci. 34:e135. 2019.4. Choi MK, Kim SB, Kim KD, Ament JD. Sequential changes of plasma C-reactive protein, erythrocyte sedimentation rate and white blood cell count in spine surgery : comparison between lumbar open discectomy and posterior lumbar interbody fusion. J Korean Neurosurg Soc. 56:218–223. 2014.5. Dobzyniak MA, Fischgrund JS, Hankins S, Herkowitz HN. Single versus multiple dose antibiotic prophylaxis in lumbar disc surgery. Spine (Phila Pa 1976). 28:E453–E455. 2003.6. Foglar C, Lindsey RW. C-reactive protein in orthopedics. Orthopedics. 21:687–691. quiz 692-693. 1998.7. Gelalis ID, Arnaoutoglou CM, Politis AN, Batzaleksis NA, Katonis PG, Xenakis TA. Bacterial wound contamination during simple and complex spinal procedures. A prospective clinical study. Spine J. 11:1042–1048. 2011.8. Harbarth S, Samore MH, Lichtenberg D, Carmeli Y. Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance. Circulation. 101:2916–2921. 2000.9. Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 163:972–978. 2003.10. Hellbusch LC, Helzer-Julin M, Doran SE, Leibrock LG, Long DJ, Puccioni MJ, et al. Single-dose vs multiple-dose antibiotic prophylaxis in instrumented lumbar fusion--a prospective study. Surg Neurol. 70:622–627. discussion 627. 2008.11. Kakimaru H, Kono M, Matsusaki M, Iwata A, Uchio Y. Postoperative antimicrobial prophylaxis following spinal decompression surgery: is it necessary? J Orthop Sci. 15:305–309. 2010.12. Kanayama M, Hashimoto T, Shigenobu K, Oha F, Togawa D. Effective prevention of surgical site infection using a Centers for Disease Control and Prevention guideline-based antimicrobial prophylaxis in lumbar spine surgery. J Neurosurg Spine. 6:327–329. 2007.13. Khan MH, Smith PN, Rao N, Donaldson WF. Serum C-reactive protein levels correlate with clinical response in patients treated with antibiotics for wound infections after spinal surgery. Spine J. 6:311–315. 2006.14. Kurtz SM, Lau E, Ong KL, Carreon L, Watson H, Albert T, et al. Infection risk for primary and revision instrumented lumbar spine fusion in the Medicare population. J Neurosurg Spine. 17:342–347. 2012.15. Mok JM, Pekmezci M, Piper SL, Boyd E, Berven SH, Burch S, et al. Use of C-reactive protein after spinal surgery: comparison with erythrocyte sedimentation rate as predictor of early postoperative infectious complications. Spine (Phila Pa 1976). 33:415–421. 2008.16. O’Toole JE, Eichholz KM, Fessler RG. Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine. 11:471–476. 2009.17. Scherer MA, Neumaier M, von Gumppenberg S. C-reactive protein in patients who had operative fracture treatment. Clin Orthop Relat Res. (393):287–293. 2001.18. Takahashi J, Ebara S, Kamimura M, Kinoshita T, Itoh H, Yuzawa Y, et al. Early-phase enhanced inflammatory reaction after spinal instrumentation surgery. Spine (Phila Pa 1976). 26:1698–1704. 2001.19. Tan TL, Shohat N, Rondon AJ, Foltz C, Goswami K, Ryan SP, et al. Perioperative antibiotic prophylaxis in total joint arthroplasty: a single dose is as effective as multiple doses. J Bone Joint Surg Am. 101:429–437. 2019.20. The Heath Insurance Review & Assessment service : Detailed implementation plan for the evaluation of prophylactic antibiotic use in surgery in 2020 (9th). Available at : https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=7623&pageIndex=1&pageIndex2=1#none/.21. Thelander U, Larsson S. Quantitation of C-reactive protein levels and erythrocyte sedimentation rate after spinal surgery. Spine (Phila Pa 1976). 17:400–404. 1992.22. Vigushin DM, Pepys MB, Hawkins PN. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest. 91:1351–1357. 1993.23. Weinstein JN, Lurie JD, Tosteson TD, Tosteson AN, Blood EA, Abdu WA, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 33:2789–2800. 2008.24. Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 91:1295–1304. 2009.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Prophylactic Antibiotics in Spinal Surgery
- THE STUDY ON THE ADMINISTRATION PERIOD OF POSTOPERATIVE PROPHYLACTIC ANTIBIOTICS AND ANTI-INFLAMMATORY DRUGS USED TO REDUCE EDEMA.
- Postoperative Spine Infections
- Comparison of Preoperative and Postoperative Parecoxib Administration for Pain Control Following Major Spine Surgery
- Comparison of erythrocyte sedimentation rate and C-reactive protein in patients with distal radius fractures according to the prophylactic antibiotic period: 1 day versus 1 week