J Korean Neurosurg Soc.
2022 Nov;65(6):816-824. 10.3340/jkns.2022.0100.
Early Restoration of Hypoperfusion Confirmed by Perfusion Magnetic Resonance Image after Emergency Superficial Temporal Artery to Middle Cerebral Artery Anastomosis
- Affiliations
-
- 1Department of Neurosurgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurosurgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- KMID: 2535841
- DOI: http://doi.org/10.3340/jkns.2022.0100
Abstract
Objective
: Emergency superficial temporal artery to middle cerebral artery (STA-MCA) anastomosis in patients with large vessel occlusion who fails mechanical thrombectomy or does not become an indication due to over the time window can be done as an alternative for blood flow restoration. The authors planned this study to quantitatively measure the degree of improvement in cerebral perfusion flow using perfusion magnetic resonance imaging (MRI) after bypass surgery and to find out what factors are related to the outcome of the bypass surgery.
Methods
: For a total of 107 patients who underwent emergent STA-MCA bypass surgery with large vessel occlusion, the National Institute of Health stroke scale (NIHSS), modified Rankin score (mRS), infarction volume, and hypoperfusion area volume was calculated, the duration between symptom onset and reperfusion time, occlusion site and infarction type were analyzed. After emergency STA-MCA bypass, hypoperfusion area volume at post-operative 7 days was calculated and analyzed compared with pre-operative hypoperfusion area volume. The factors affecting the improvement of mRS were analyzed. The clinical status of patients who underwent emergency bypass was investigated by mRS and NIHSS before and after surgery, and changes in infarct volume, extent, degree of collateral circulation, and hypoperfusion area volume were measured using MRI and digital subtraction angiography (DSA).
Results
: The preoperative infarction volume was median 10 mL and the hypoperfusion area volume was median 101 mL. NIHSS was a median of 8 points, and the last normal to operation time was a median of 60.7 hours. STA patency was fair in 97.1% of patients at 6 months follow-up DSA and recanalization of the occluded vessel was confirmed at 26.5% of patients. Infarction volume significantly influenced the improvement of mRS (p=0.010) but preoperative hypoperfusion volume was not significantly influenced (p=0.192), and the infarction type showed marginal significance (p=0.0508). Preoperative NIHSS, initial mRS, occlusion vessel type, and last normal to operation time did not influence the improvement of mRS (p=0.272, 0.941, 0.354, and 0.391).
Conclusion
: In a patient who had an acute cerebral infarction due to large vessel occlusion with large ischemic penumbra but was unable to perform mechanical thrombectomy, STA-MCA bypass could be performed. By using time-to-peak images of perfusion MRI, it is possible to quickly and easily confirm that the brain tissue at risk is preserved and that the ischemic penumbra is recovered to a normal blood flow state.
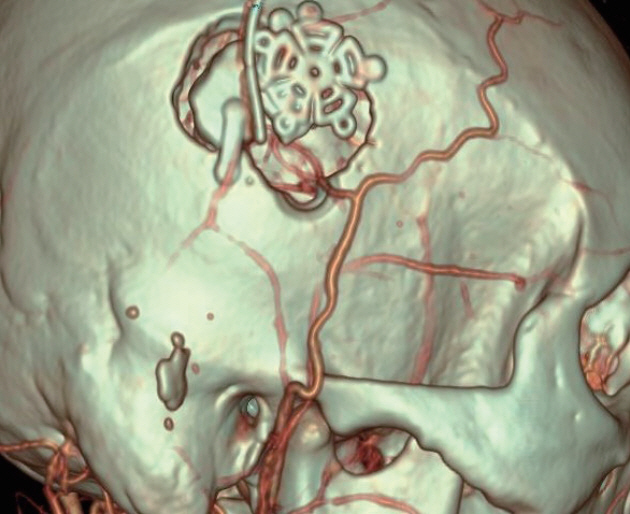
Figure
Reference
-
References
1. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 378:708–718. 2018.2. Astrup J, Symon L, Branston NM, Lassen NA. Cortical evoked potential and extracellular K+ and H+ at critical levels of brain ischemia. Stroke. 8:51–57. 1977.3. Back T. Pathophysiology of the ischemic penumbra--revision of a concept. Cell Mol Neurobiol. 18:621–638. 1998.4. Demeestere J, Wouters A, Christensen S, Lemmens R, Lansberg MG. Review of perfusion imaging in acute ischemic stroke: from time to tissue. Stroke. 51:1017–1024. 2020.5. Desai SM, Haussen DC, Aghaebrahim A, Al-Bayati AR, Santos R, Nogueira RG, et al. Thrombectomy 24 hours after stroke: beyond DAWN. J Neurointerv Surg. 10:1039–1042. 2018.6. EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. 313:1191–1200. 1985.7. Grubb RL Jr, Powers WJ, Clarke WR, Videen TO, Adams HP Jr, Derdeyn CP, et al. Surgical results of the carotid occlusion surgery study. J Neurosurg. 118:25–33. 2013.8. Jo H, Seo D, Kim YD, Ban SP, Kim T, Kwon OK, et al. Quantitative radiological analysis and clinical outcomes of urgent EC-IC bypass for hemodynamic compromised patients with acute ischemic stroke. Sci Rep. 12:8816. 2022.9. Kim H, Kim Y, Kim YW, Kim SR, Yang SH. Perfusion-weighted MRI parameters for prediction of early progressive infarction in middle cerebral artery occlusion. J Korean Neurosurg Soc. 59:346–351. 2016.10. Kim JH, Yoon W, Kim CK, Roh H, Bae HJ, Kwon TH, et al. Efficacy and safety of timely urgent superficial temporal artery-to-middle cerebral artery bypass surgery in patients with acute ischemic stroke: a single-institutional prospective study and a pooled analysis. Cerebrovasc Dis. 50:34–45. 2021.11. Lee SB, Huh PW, Kim DS, Yoo DS, Lee TG, Cho KS. Early superficial temporal artery to middle cerebral artery bypass in acute ischemic stroke. Clin Neurol Neurosurg. 115:1238–1244. 2013.12. Leigh R, Knutsson L, Zhou J, van Zijl PC. Imaging the physiological evolution of the ischemic penumbra in acute ischemic stroke. J Cereb Blood Flow Metab. 38:1500–1516. 2018.13. McKetton L, Venkatraghavan L, Rosen C, Mandell DM, Sam K, Sobczyk O, et al. Improved white matter cerebrovascular reactivity after revascularization in patients with steno-occlusive disease. AJNR Am J Neuroradiol. 40:45–50. 2019.14. Moustafa RR, Baron JC. Pathophysiology of ischaemic stroke: insights from imaging, and implications for therapy and drug discovery. Br J Pharmacol 153 Suppl. 1(Suppl 1):S44–S54. 2008.15. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 378:11–21. 2018.16. Nussbaum ES, Janjua TM, Defillo A, Lowary JL, Nussbaum LA. Emergency extracranial-intracranial bypass surgery for acute ischemic stroke. J Neurosurg. 112:666–673. 2010.17. Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA. 306:1983–1992. 2011.18. Schmiedek P, Olteanu-Nerbe V, Marguth F. Timing of extracranial-intracranial arterial bypass surgery with special reference to acute cerebral ischaemia. Neurosurg Rev. 6:19–24. 1983.19. Tsivgoulis G, Safouris A, Katsanos AH, Arthur AS, Alexandrov AV. Mechanical thrombectomy for emergent large vessel occlusion: a critical appraisal of recent randomized controlled clinical trials. Brain Behav. 6:e00418. 2016.20. Vilela P, Rowley HA. Brain ischemia: CT and MRI techniques in acute ischemic stroke. Eur J Radiol. 96:162–172. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Middle Cerebral Artery AneurysmOriginating Near the Site of Anastomosis after Superficial Temporal Artery-Middle Cerebral Artery Bypass: Case Report
- External Carotid Artery Angioplasty and Stenting Followed by Superficial Temporal Artery to Middle Cerebral Artery Anastomosis
- Emergency In Situ Bypass during Middle Cerebral Artery Aneurysm Surgery: Middle Cerebral Artery-Superficial Temporal Artery Interposition Graft-Middle Cerebral Artery Anastomosis
- Superficial Temporal Artery-Middle Cerebral Artery Anastomosis for Internal Carotid Artery Occlusion by Subacute In-Stent Thrombosis after Carotid Artery Stenting
- Occlusion of the Middle Cerebral Artery Branch Mimicking Aneurysm