J Korean Neurosurg Soc.
2022 Nov;65(6):801-815. 10.3340/jkns.2022.0021.
Evaluation of Stent Apposition in the LVIS Blue Stent-Assisted Coiling of Distal Internal Carotid Artery Aneurysms : Correlation with Clinical and Angiographic Outcomes
- Affiliations
-
- 1Department of Neurosurgery, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2535840
- DOI: http://doi.org/10.3340/jkns.2022.0021
Abstract
Objective
: To evaluate the stent apposition of a low-profile visualized intraluminal support (LVIS) device in distal internal carotid artery (ICA) aneurysms, examine its correlation with clinical and angiographic outcomes, and determine the predictive factors of ischemic adverse events (IAEs) related to stent-assisted coiling.
Methods
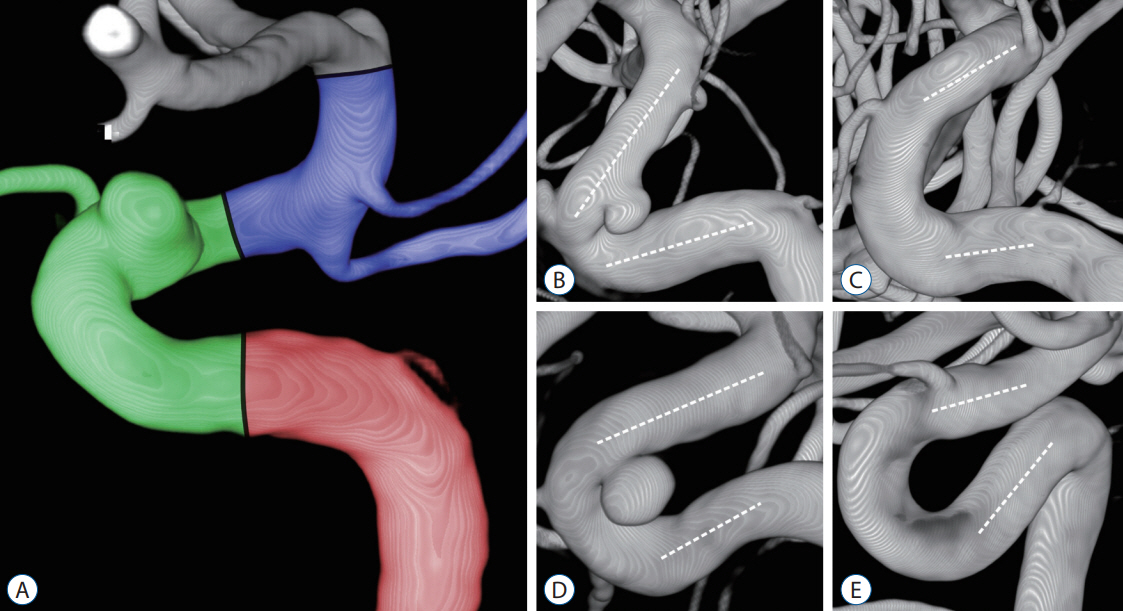
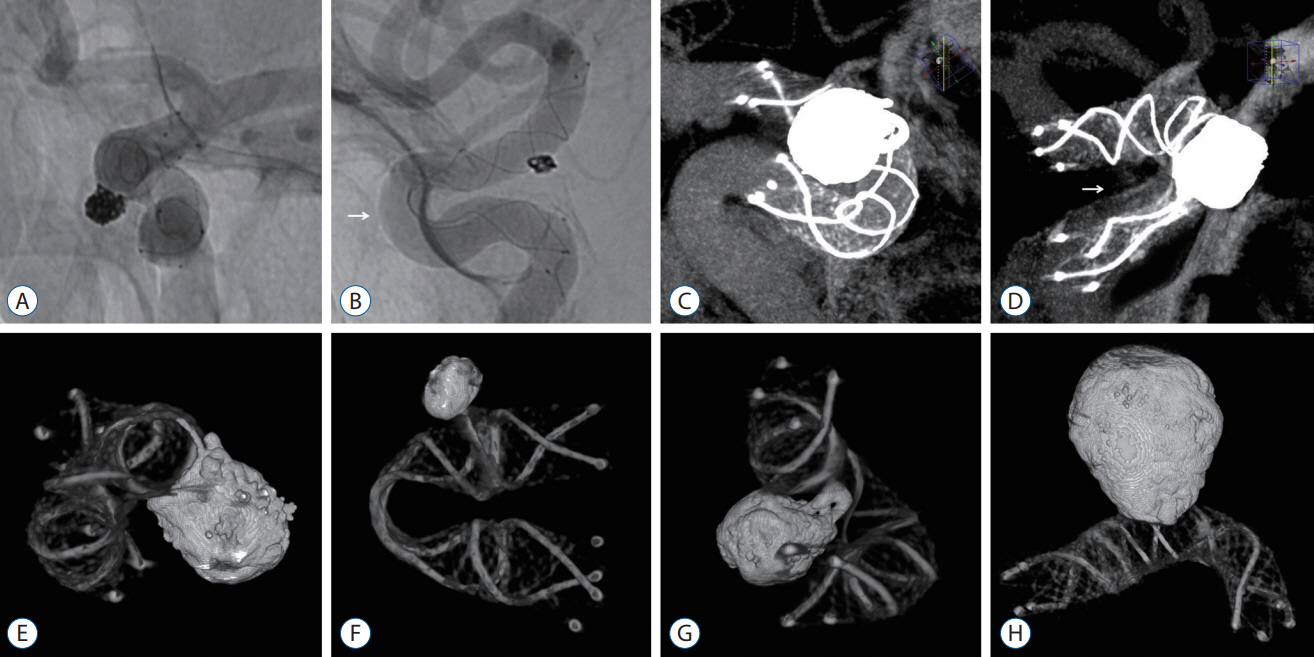
: We retrospectively analyzed a prospectively maintained database of 183 patients between January 2017 and February 2020. The carotid siphon from the cavernous ICA to the ICA terminus was divided into posterior, anterior, and superior bends. The anterior bends were categorized into angled (V) and non-angled (C, U, and S) types depending on the morphology and measured angles. Complete stent apposition (CSA) and incomplete stent apposition (ISA) were evaluated using unsubtracted angiography and flat-panel detector computed tomography. Dual antiplatelet therapy with aspirin 200 mg and clopidogrel 75 mg was administered. Clopidogrel resistance was defined as fewer responders (≥10%, <40%) and non-responders (<10%) based on the percent inhibition (%INH) of the VerifyNow system. These were counteracted by a dose escalation to 150 mg for fewer responders or substitution with cilostazol 200 mg for non-responders. IAEs included intraoperative in-stent thrombosis, transient ischemic attack, cerebral infarction, and delayed in-stent stenosis. A multivariate logistic regression analysis was used to determine the predictive factors for ISA and IAEs.
Results
: There were 33 ISAs (18.0%) and 27 IAEs (14.8%). The anterior bend angle was narrower in ISA (-4.16°±25.18°) than in CSA (23.52°±23.13°) (p<0.001). The V- and S-types were independently correlated with the ISA (p<0.001). However, treatment outcomes, including IAEs (15.3% vs. 12.1%), aneurysmal complete occlusion (91.3% vs. 88.6%), and recanalization (none of them), did not differ between CSA and ISA (p>0.05). The %INH of 27 IAEs (13.78%±14.78%) was significantly lower than that of 156 non-IAEs (26.82%±20.23%) (p<0.001). Non-responders to clopidogrel were the only significant predictive factor for IAEs (p=0.001).
Conclusion
: The angled and tortuous anatomical peculiarity of the carotid siphon caused ISA of the LVIS device; however, it did not affect clinical and angiographic outcomes, while the non-responders to clopidogrel affected the IAEs related to stent-assisted coiling.
Keyword
Figure
Reference
-
References
1. Benndorf G, Strother CM, Claus B, Naeini R, Morsi H, Klucznik R, et al. Angiographic CT in cerebrovascular stenting. AJNR Am J Neuroradiol. 26:1813–1818. 2005.2. Bouillot P, Brina O, Ouared R, Yilmaz H, Farhat M, Erceg G, et al. Geometrical deployment for braided stent. Med Image Anal. 30:85–94. 2016.3. Cho YD, Sohn CH, Kang HS, Kim JE, Cho WS, Hwang G, et al. Coil embolization of intracranial saccular aneurysms using the low-profile visualized intraluminal support (LVIS™) device. Neuroradiology. 56:543–551. 2014.4. Chung J, Matsuda Y, Nelson J, Keigher K, Lopes DK. A new low-profile visualized intraluminal support (LVIS) device, LVIS Blue: laboratory comparison between old and new LVIS. Neurol Res. 40:78–85. 2018.5. Dholakia RJ, Kappel AD, Pagano A, Woo HH, Lieber BB, Fiorella DJ, et al. In vitro angiographic comparison of the flow-diversion performance of five neurovascular stents. Interv Neuroradiol. 24:150–161. 2018.6. Dumont TM, Eller JL, Mokin M, Sorkin GC, Levy EI. Advances in endovascular approaches to cerebral aneurysms. Neurosurgery 74 Suppl. 1:S17–S31. 2014.7. Fiorella D, Arthur A, Boulos A, Diaz O, Jabbour P, Pride L, et al. Final results of the US humanitarian device exemption study of the low-profile visualized intraluminal support (LVIS) device. J Neurointerv Surg. 8:894–897. 2016.8. Gurbel PA, Bliden KP, Butler K, Tantry US, Gesheff T, Wei C, et al. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study. Circulation. 120:2577–2585. 2009.9. Ha EJ, Cho WS, Kim JE, Cho YD, Choi HH, Kim T, et al. Prophylactic antiplatelet medication in endovascular treatment of intracranial aneurysms: low-dose prasugrel versus clopidogrel. AJNR Am J Neuroradiol. 37:2060–2065. 2016.10. Heller RS, Malek AM. Parent vessel size and curvature strongly influence risk of incomplete stent apposition in enterprise intracranial aneurysm stent coiling. AJNR Am J Neuroradiol. 32:1714–1720. 2011.11. Heller RS, Malek AM. Delivery technique plays an important role in determining vessel wall apposition of the enterprise self-expanding intracranial stent. J Neurointerv Surg. 3:340–343. 2011.12. Heller RS, Miele WR, Do-Dai DD, Malek AM. Crescent sign on magnetic resonance angiography revealing incomplete stent apposition: correlation with diffusion-weighted changes in stent-mediated coil embolization of aneurysms. J Neurosurg. 115:624–632. 2011.13. Hwang G, Huh W, Lee JS, Villavicencio JB, Villamor RB Jr, Ahn SY, et al. Standard vs modified antiplatelet preparation for preventing thromboembolic events in patients with high on-treatment platelet reactivity undergoing coil embolization for an unruptured intracranial aneurysm: a randomized clinical trial. JAMA Neurol. 72:764–772. 2015.14. Ikeda H, Otsuka R, Uesaka D, Sano N, Torikoshi S, Hayase M, et al. Effects of acute angle, proximal bending, and distal bending in the deployment vessels on incomplete low-profile visualized intraluminal support (LVIS) expansion: an in vitro study. J Neurointerv Surg. 13:453–458. 2021.15. Iosif C, Piotin M, Saleme S, Barreau X, Sedat J, Chau Y, et al. Safety and effectiveness of the low profile visualized intraluminal support (LVIS and LVIS Jr) devices in the endovascular treatment of intracranial aneurysms: results of the TRAIL multicenter observational study. J Neurointerv Surg. 10:675–681. 2018.16. Jankowitz BT, Gross BA, Seshadhri S, Girdhar G, Jadhav A, Jovin TG, et al. Hemodynamic differences between pipeline and coil-adjunctive intracranial stents. J Neurointerv Surg. 11:908–911. 2019.17. Kim CH, Hwang G, Kwon OK, Ban SP, Chinh ND, Tjahjadi M, et al. P2Y12 reaction units threshold for implementing modified antiplatelet preparation in coil embolization of unruptured aneurysms: a prospective validation study. Radiology. 282:542–551. 2017.18. Kim HJ, Oh JS, Park SQ, Yoon SM, Ahn HS, Kim BT. The efficacy of P2Y12 reactive unit to predict the periprocedural thromboembolic and hemorrhagic complications according to clopidogrel responsiveness and safety of modification of dual antiplatelet therapy : a meta-analysis. J Korean Neurosurg Soc. 63:539–549. 2020.19. Kim YD, Kwon OK, Ban SP, Won YD, Bang JS, Kim T, et al. The inhibition rate estimated using verifynow can help to predict the thromboembolic risk of coil embolization for unruptured intracranial aneurysms. J Neurointerv Surg. 14:589–592. 2022.20. Koch MJ, Stapleton CJ, Raymond SB, Williams S, Leslie-Mazwi TM, Rabinov JD, et al. LVIS Blue as a low porosity stent and coil adjuvant. J Neurointerv Surg. 10:682–686. 2018.21. Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH, et al. An update to the raymond-roy occlusion classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg. 7:496–502. 2015.22. Matsuda Y, Chung J, Keigher K, Lopes D. A comparison between the new Low-profile Visualized Intraluminal Support (LVIS Blue) stent and the Flow Redirection Endoluminal Device (FRED) in bench-top and cadaver studies. J Neurointerv Surg. 10:274–278. 2018.23. Mokin M, Primiani CT, Ren Z, Piper K, Fiorella DJ, Rai AT, et al. Stent-assisted coiling of cerebral aneurysms: multi-center analysis of radiographic and clinical outcomes in 659 patients. J Neurointerv Surg. 12:289–297. 2020.24. Rouchaud A, Ramana C, Brinjikji W, Ding YH, Dai D, Gunderson T, et al. Wall apposition is a key factor for aneurysm occlusion after flow diversion: a histologic evaluation in 41 rabbits. AJNR Am J Neuroradiol. 37:2087–2091. 2016.25. Waihrich E, Clavel P, Mendes GAC, Iosif C, Moraes Kessler I, Mounayer C. Influence of carotid siphon anatomy on brain aneurysm presentation. AJNR Am J Neuroradiol. 38:1771–1775. 2017.26. Waihrich E, Clavel P, Mendes G, Iosif C, Kessler IM, Mounayer C. Influence of anatomic changes on the outcomes of carotid siphon aneurysms after deployment of flow-diverter stents. Neurosurgery. 83:1226–1233. 2018.27. Wang C, Tian Z, Liu J, Jing L, Paliwal N, Wang S, et al. Flow diverter effect of LVIS stent on cerebral aneurysm hemodynamics: a comparison with Enterprise stents and the Pipeline device. J Transl Med. 14:199. 2016.28. Wanke I, Forsting M. Stents for intracranial wide-necked aneurysms: more than mechanical protection. Neuroradiology. 50:991–998. 2008.29. Wu P, Ocak PE, Wang D, Ocak U, Xu S, Li Y, et al. Endovascular treatment of ruptured tiny intracranial aneurysms with low-profile visualized intraluminal support device. J Stroke Cerebrovasc Dis. 28:330–337. 2019.30. Yuki I, Ishibashi T, Dahmani C, Kato N, Ikemura A, Abe Y, et al. Combination of high-resolution cone beam computed tomography and metal artefact reduction software: a new image fusion technique for evaluating intracranial stent apposition after aneurysm treatment. BMJ Case Rep. 12:e230687. 2019.31. Zhang C, Pu F, Li S, Xie S, Fan Y, Li D. Geometric classification of the carotid siphon: association between geometry and stenoses. Surg Radiol Anat. 35:385–394. 2013.32. Zhang H, Gao X, Liang H, Ren Y. Incomplete stent apposition of low-profile visualized intraluminal support stents in the treatment of cerebral aneurysms. J Neurointerv Surg. 12:591–597. 2020.33. Zhang X, Zhong J, Gao H, Xu F, Bambakidis NC. Endovascular treatment of intracranial aneurysms with the LVIS device: a systematic review. J Neurointerv Surg. 9:553–557. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- Overlapping Stents-Assisted Coiling for Vertebral Artery Dissecting Aneurysm : LVIS Stent within Neuroform EZ Stent
- Very Late Stent Thrombosis after Sole Stent-Assisted Coiling at the Paraclinoid Giant Aneurysm : Could Prophylactic Antiplatelet Therapy Be Ceased at the Only 1 Year after Procedure?
- Clinical and Angiographic Outcomes of Aneurysms Treated with Two Self-expanding Stent-assisted Coiling Systems: A Comparison of Solitaire AB and Enterprise VRD Stents
- Kissing Aneurysms at Fenestrated Proximal Basilar Artery: Double-barrel Stent-assisted Coiling Using Dual Closed-cell Stents