Anesth Pain Med.
2022 Oct;17(4):412-419. 10.17085/apm.22168.
Five-year all-cause mortality in critically ill liver transplant patients with coronary artery disease: analysis of acute-on chronic liver failure
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Laboratory for Cardiovascular Dynamics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2535340
- DOI: http://doi.org/10.17085/apm.22168
Abstract
- Background
Patients with acute-on-chronic liver failure (ACLF) are critically ill and have high waiting-list mortality. Although studies demonstrated that appropriately treated coronary artery disease (CAD) should not be regarded as a contraindication to liver transplant (LT), data regarding long-term outcomes in critically ill liver LT recipients are lacking. The aim of this study was to compare the rates of all-cause death at 5 years following LT in patients with ACLF with or without CAD.
Methods
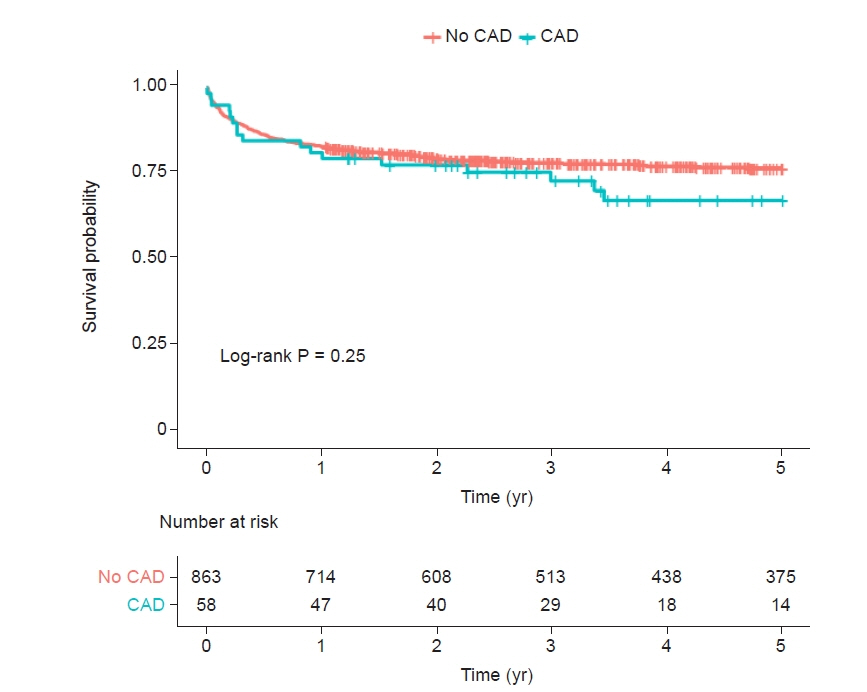
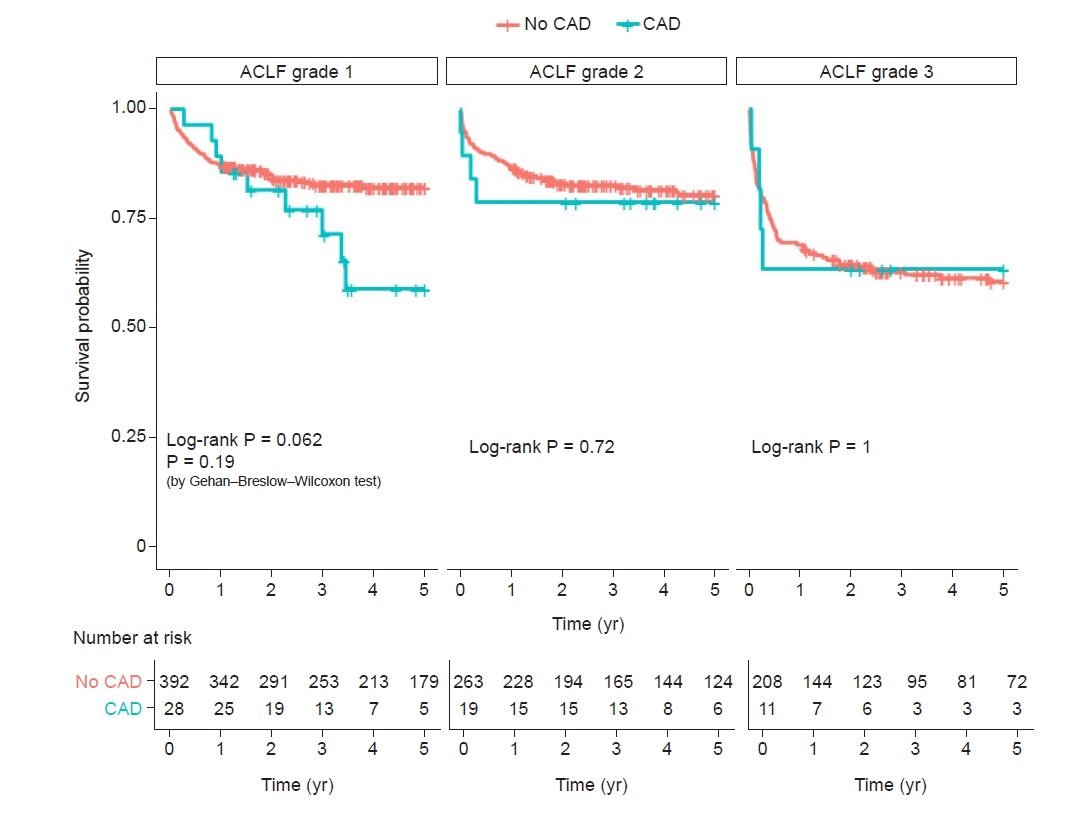
Between 2010 and 2020, we evaluated 921 consecutive LT patients (MELD score, 32 ± 9) and ACLF classified by CLIF-C ACLF score. Up to 5-year all-cause death according to the CAD status was examined. CAD was defined as a preoperative history of coronary artery bypass graft or a percutaneous intervention and old myocardial infarction. Kaplan-Meier survival analysis was used.
Results
Up to 5 years, 212 (23.0%) of all ACLF patients (n = 921) in whom 17 (29.3%) of 58 CAD patients died. In patients with CAD (6.3%, 58/921), the Kaplan-Meier cumulative mortality rate at 5 years was numerically higher but was not statistically significant when compared with those without CAD (32.9% vs. 23.5%, log-rank, P = 0.25). In subgr oup analysis, there were comparable risks of cumulative mortalities at 5 years across the stratification of ACLF grade 1, 2, and 3 (log-rank P = 0.062, P = 0.72, and P = 0.999, respectively).
Conclusions
All-cause mortality is high in patients with ACLF after LT but is not related to the presence of revascularized or treated CAD, across the stratification of ACLF grades.
Figure
Reference
-
1. Koshy AN, Gow PJ, Han HC, Teh AW, Jones R, Testro A, et al. Cardiovascular mortality following liver transplantation: predictors and temporal trends over 30 years. Eur Heart J Qual Care Clin Outcomes. 2020; 6:243–53.
Article2. Kwon HM, Hwang GS. Cardiovascular dysfunction and liver transplantation. Korean J Anesthesiol. 2018; 71:85–91.
Article3. Kwon HM, Moon YJ, Kim KS, Shin WJ, Huh IY, Jun IG, et al. Prognostic value of B-type natriuretic peptide in liver transplant patients: implication in posttransplant mortality. Hepatology. 2021; 74:336–50.
Article4. Kwon HM, Moon YJ, Jung KW, Park YS, Kim KS, Jun IG, et al. Appraisal of cardiac ejection fraction with liver disease severity: implication in post-liver transplantation mortality. Hepatology. 2020; 71:1364–80.
Article5. Skaro AI, Gallon LG, Lyuksemburg V, Jay CL, Zhao L, Ladner DP, et al. The impact of coronary artery disease on outcomes after liver transplantation. J Cardiovasc Med (Hagerstown). 2016; 17:875–85.
Article6. Satapathy SK, Vanatta JM, Helmick RA, Flowers A, Kedia SK, Jiang Y, et al. Outcome of liver transplant recipients with revascularized coronary artery disease: a comparative analysis with and without cardiovascular risk factors. Transplantation. 2017; 101:793–803.
Article7. Patel SS, Lin FP, Rodriguez VA, Bhati C, John BV, Pence T, et al. The relationship between coronary artery disease and cardiovascular events early after liver transplantation. Liver Int. 2019; 39:1363–71.
Article8. Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. CANONIC Study Investigators of the EASL–CLIF Consortium. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013; 144:1426–37, 1437.e1-9.
Article9. Artzner T, Michard B, Weiss E, Barbier L, Noorah Z, Merle JC, et al. Liver transplantation for critically ill cirrhotic patients: stratifying utility based on pretransplant factors. Am J Transplant. 2020; 20:2437–48.
Article10. Jalan R, Saliba F, Pavesi M, Amoros A, Moreau R, Ginès P, et al. CANONIC study investigators of the EASL-CLIF Consortium. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol. 2014; 61:1038–47.11. Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, et al. Acute-on chronic liver failure. J Hepatol. 2012; 57:1336–48.
Article12. Moon KW. R statistics and graphs for medical papers. Seoul: Hannarae;2015. p. 466.13. Moon KW. autoReg: automatic linear and logistic regression and survival analysis. Web-R.org [Internet]. [cited 2022 Jan 11]. Available from https://cran.r-project.org/web/packages/autoReg/index.html.14. Therneau TM. A package for survival analysis in S. Version 2.38. CRAN.R-project.org [Internet]. [cited 2015]. Available from https://mran.microsoft.com/snapshot/2017-02-04/web/packages/survival/citation.html.15. Therneau TM. A package for survival analysis in R. R package version 3.4-0. CRAN.R-project.org [Internet]. [cited 2022 Aug 9]. Available from https://cran.r-project.org/web/packages/survival/index.html.16. Arroyo V, Moreau R, Kamath PS, Jalan R, Ginès P, Nevens F, et al. Acute-on-chronic liver failure in cirrhosis. Nat Rev Dis Primers. 2016; 2:16041.
Article17. Arroyo V, Moreau R, Jalan R, Ginès P; EASL-CLIF Consortium CANONIC Study. Acute-on-chronic liver failure: a new syndrome that will re-classify cirrhosis. J Hepatol. 2015; 62(1 Suppl):S131–43.
Article18. Artzner T, Michard B, Besch C, Levesque E, Faitot F. Liver transplantation for critically ill cirrhotic patients: overview and pragmatic proposals. World J Gastroenterol. 2018; 24:5203–14.
Article19. Sundaram V, Kogachi S, Wong RJ, Karvellas CJ, Fortune BE, Mahmud N, et al. Effect of the clinical course of acute-on-chronic liver failure prior to liver transplantation on post-transplant survival. J Hepatol. 2020; 72:481–8.
Article20. Barman PM, VanWagner LB. Cardiac risk assessment in liver transplant candidates: current controversies and future directions. Hepatology. 2021; 73:2564–76.
Article21. Wray C, Scovotti JC, Tobis J, Niemann CU, Planinsic R, Walia A, et al. Liver transplantation outcome in patients with angiographically proven coronary artery disease: a multi-institutional study. Am J Transplant. 2013; 13:184–91.
Article22. Moon YJ, Kwon HM, Jung KW, Jeong HW, Park YS, Jun IG, et al. Risk stratification of myocardial injury after liver transplantation in patients with computed tomographic coronary angiography-diagnosed coronary artery disease. Am J Transplant. 2019; 19:2053–66.
Article23. Lentine KL, Costa SP, Weir MR, Robb JF, Fleisher LA, Kasiske BL, et al. American Heart Association Council on the Kidney in Cardiovascular Disease and Council on Peripheral Vascular Disease; American Heart Association; American College of Cardiology Foundation. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation: endorsed by the American Society of Transplant Surgeons, American Society of Transplantation, and National Kidney Foundation. Circulation. 2012; 126:617–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Difference of the Clinical Patterns between Acute Liver Failure and Acute-on-Chronic Liver Failure
- Mortality scoring systems for liver transplant recipients: before and after model for end-stage liver disease score
- Understanding Acute Liver Failure: A Basic Overview of Definition and Treatment
- Acute-on-chronic liver failure: Terminology, mechanisms and management
- Pediatric Liver Transplantation for Metabolic Liver Disease