Acute Crit Care.
2022 Aug;37(3):438-453. 10.4266/acc.2021.01501.
Cardiopulmonary resuscitation of infants at birth: predictable or unpredictable?
- Affiliations
-
- 1Maternal, Fetal and Neonatal Research Center, Tehran University of Medical Sciences, Tehran, Iran
- 2Department of Neonatology, Yas Hospital Complex, Tehran University of Medical Sciences, Tehra, Iran
- 3PhD Candidate in Reproductive Health, Maternal, Fetal and Neonatal Research Center, Institute of Family Health, Tehran University of Medical Sciences, Tehran, Iran
- 4Department of Advanced Technologies, School of Medicine, North Khorasan University of Medical Sciences, Bojnurd, Iran
- KMID: 2535308
- DOI: http://doi.org/10.4266/acc.2021.01501
Abstract
- Background
Anticipating the need for at-birth cardiopulmonary resuscitation (CPR) in neonates is very important and complex. Timely identification and rapid CPR for neonates in the delivery room significantly reduce mortality and other neurological disabilities. The aim of this study was to create a prediction system for identifying the need for at-birth CPR in neonates based on Machine Learning (ML) algorithms.
Methods
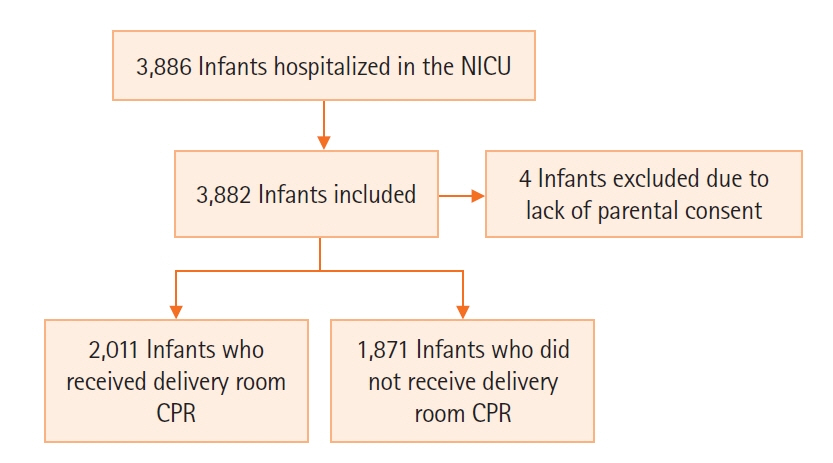
In this study, 3,882 neonatal medical records were retrospectively reviewed. A total of 60 risk factors was extracted, and five ML algorithms of J48, Naïve Bayesian, multilayer perceptron, support vector machine (SVM), and random forest were compared to predict the need for at-birth CPR in neonates. Two types of resuscitation were considered: basic and advanced CPR. Using five feature selection algorithms, features were ranked based on importance, and important risk factors were identified using the ML algorithms.
Results
To predict the need for at-birth CPR in neonates, SVM using all risk factors reached 88.43% accuracy and F-measure of 88.4%, while J48 using only the four first important features reached 90.89% accuracy and F-measure of 90.9%. The most important risk factors were gestational age, delivery type, presentation, and mother’s addiction.
Conclusions
The proposed system can be useful in predicting the need for CPR in neonates in the delivery room.
Keyword
Figure
Reference
-
1. Moshiro R, Mdoe P, Perlman JM. A global view of neonatal asphyxia and resuscitation. Front Pediatr. 2019; 7:489.
Article2. Shikuku DN, Milimo B, Ayebare E, Gisore P, Nalwadda G. Practice and outcomes of neonatal resuscitation for newborns with birth asphyxia at Kakamega County General Hospital, Kenya: a direct observation study. BMC Pediatr. 2018; 18:167.
Article3. World Health Organization. Guidelines on basic newborn resuscitation. Geneva: World Health Organization;2012.4. Reynolds C, Cox J, Livingstone V, Dempsey EM. Rescuer exertion and fatigue using two-thumb vs. two-finger method during simulated neonatal cardiopulmonary resuscitation. Front Pediatr. 2020; 8:133.
Article5. Cheung PY, Huang H, Xu C, Liu JQ, Ting JY, Wong R, et al. Comparing the quality of cardiopulmonary resuscitation performed at the over-the-head position and lateral position of neonatal manikin. Front Pediatr. 2020; 7:559.
Article6. Hosono S, Tamura M, Isayama T, Sugiura T, Kusakawa I, Ibara S, et al. Neonatal cardiopulmonary resuscitation project in Japan. Pediatr Int. 2019; 61:634–40.
Article7. Fischer N, Soraisham A, Shah PS, Synnes A, Rabi Y, Singhal N, et al. Extensive cardiopulmonary resuscitation of preterm neonates at birth and mortality and developmental outcomes. Resuscitation. 2019; 135:57–65.8. Savani M, Upadhyay K, Talati AJ. Characteristics and outcomes of very low birth weight infants receiving epinephrine during delivery room resuscitation. Resuscitation. 2017; 115:1–4.
Article9. Foglia EE, Weiner G, de Almeida MF, Wyllie J, Wyckoff MH, Rabi Y, et al. Duration of resuscitation at birth, mortality, and neurodevelopment: a systematic review. Pediatrics. 2020; 146:e20201449.
Article10. Sarrato Z, Sarrato Z, Chamorro P, Castro V, Pacheco G, Luna S. Perinatal risk factors and outcome of preterm infants ≤27 weeks of gestational age who received delivery room cardiopulmonary resuscitation (CPR) [abstract]. J Perinatal Med. 2015; 43(s1):432–1299. Abstract no. P-0381.11. Deliberato RO, Escudero GG, Bulgarelli L, Neto AS, Ko SQ, Campos NS, et al. SEVERITAS: an externally validated mortality prediction for critically ill patients in low and middle-income countries. Int J Med Inform. 2019; 131:103959.
Article12. Kefi Z, Aloui K, Naceur MS. The early prediction of neonates mortality in intensive care unit. In: 2019 International Conference on Advanced Systems and Emergent Technologies (IC_ASET); 2019; Hammamet, Tunisia.13. Ahmad KA, Velasquez SG, Kohlleppel KL, Henderson CL, Stine CN, LeVan JM, et al. The characteristics and outcomes of cardiopulmonary resuscitation within the neonatal intensive care unit based on gestational age and unit level of care. Am J Perinatol. 2020; 37:1455–61.
Article14. Campbell ME, Byrne PJ. Cardiopulmonary resuscitation and epinephrine infusion in extremely low birth weight infants in the neonatal intensive care unit. J Perinatol. 2004; 24:691–5.
Article15. Kostelanetz AS, Dhanireddy R. Survival of the very-low-birth-weight infants after cardiopulmonary resuscitation in neonatal intensive care unit. J Perinatol. 2004; 24:279–83.
Article16. Lantos JD, Miles SH, Silverstein MD, Stocking CB. Survival after cardiopulmonary resuscitation in babies of very low birth weight: is CPR futile therapy? N Engl J Med. 1988; 318:91–5.
Article17. Salhab WA, Wyckoff MH, Laptook AR, Perlman JM. Initial hypoglycemia and neonatal brain injury in term infants with severe fetal acidemia. Pediatrics. 2004; 114:361–6.
Article18. Afjeh SA, Sabzehei MK, Esmaili F. Neonatal resuscitation in the delivery room from a tertiary level hospital: risk factors and outcome. Iran J Pediatr. 2013; 23:675–80.19. Jiang S, Lyu Y, Ye XY, Monterrosa L, Shah PS, Lee SK. Intensity of delivery room resuscitation and neonatal outcomes in infants born at 33 to 36 weeks’ gestation. J Perinatol. 2016; 36:100–5.
Article20. Sood S, Giacoia GP. Cardiopulmonary resuscitation in very low birthweight infants. Am J Perinatol. 1992; 9:130–3.
Article21. Zaichkin J, Kattwinkel J, McGowan J; American Heart Association; American Academy of Pediatrics. Textbook of neonatal resuscitation. Elk Grove Village: American Heart Association, American Academy of Pediatrics; 2011.22. Kattwinkel J, Niermeyer S, Nadkarni V, Tibballs J, Phillips B, Zideman D, et al. ILCOR advisory statement: resuscitation of the newly born infant: an advisory statement from the pediatric working group of the International Liaison Committee on Resuscitation. Circulation. 1999; 99:1927–38.
Article23. American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric advanced life support. Pediatrics. 2006; 117:e1005–28.24. Weiner G, Zaichkin J, Kattwinkel J; American Academy of Pediatrics; American Heart Association. Textbook of neonatal resuscitation. 7th ed. Elk Grove Village: American Academy of Pediatrics; 2016.25. Lee AC, Cousens S, Wall SN, Niermeyer S, Darmstadt GL, Carlo WA, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health. 2011; 11(Suppl 3):S12.
Article26. American Academy of Pediatrics. Neonatal resuscitation program [Internet]. Itasca (IL): American Academy of Pediatrics;2020. [cited 2022 Mar 1]. Available from: https://www.aap.org/en/learning/neonatal-resuscitation-program/.27. Hendson L, Russell L, Robertson CM, Liang Y, Chen Y, Abdalla A, et al. Neonatal and neurodevelopmental outcomes of very low birth weight infants with histologic chorioamnionitis. J Pediatr. 2011; 158:397–402.
Article28. Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994; 84:1414–20.
Article29. Bazilevych K, Meniailov I, Fedulov K, Goranina S, Chumachenko D, Pyrohov P. Determining the probability of heart disease using data mining methods. In: 2nd International Workshop on Informatics & Data-Driven Medicine; 2019; Lviv, Ukraine:30. Hu L, Gao W, Zhao K, Zhang P, Wang F. Feature selection considering two types of feature relevancy and feature interdependency. Expert Syst Appl. 2018; 93:423–34.
Article31. Saeys Y, Inza I, Larrañaga P. A review of feature selection techniques in bioinformatics. Bioinformatics. 2007; 23:2507–17.
Article32. Sheikhtaheri A, Zarkesh MR, Moradi R, Kermani F. Prediction of neonatal deaths in NICUs: development and validation of machine learning models. BMC Med Inform Decis Mak. 2021; 21:131.
Article33. Urbanowicz RJ, Meeker M, La Cava W, Olson RS, Moore JH. Relief-based feature selection: Introduction and review. J Biomed Inform. 2018; 85:189–203.
Article34. González R, Rupérez M, Sevene E, Vala A, Maculuve S, Bulo H, et al. Effects of HIV infection on maternal and neonatal health in southern Mozambique: a prospective cohort study after a decade of antiretroviral drugs roll out. PLoS One. 2017; 12:e0178134.
Article35. Macdonald EM, Ng R, Bayoumi AM, Raboud J, Brophy J, Masinde KI, et al. Adverse neonatal outcomes among women living with HIV: a population-based study. J Obstet Gynaecol Can. 2015; 37:302–9.
Article36. Theron G, Brummel S, Fairlie L, Pinilla M, McCarthy K, Owor M, et al. Pregnancy outcomes of women conceiving on antiretroviral therapy (ART) compared to those commenced on ART during pregnancy. Clin Infect Dis. 2021; 73:e312–20.
Article37. Wedi CO, Kirtley S, Hopewell S, Corrigan R, Kennedy SH, Hemelaar J. Perinatal outcomes associated with maternal HIV infection: a systematic review and meta-analysis. Lancet HIV. 2016; 3:e33–48.
Article38. Araujo Júnior E, Peixoto AB, Zamarian AC, Elito Júnior J, Tonni G. Macrosomia. Best Pract Res Clin Obstet Gynaecol. 2017; 38:83–96.
Article39. Nkwabong E, Nzalli Tangho GR. Risk factors for macrosomia. J Obstet Gynaecol India. 2015; 65:226–9.
Article40. Bajaj M, Natarajan G, Shankaran S, Wyckoff M, Laptook AR, Bell EF, et al. Delivery room resuscitation and short-term outcomes in moderately preterm infants. J Pediatr. 2018; 195:33–8.41. Wyckoff MH, Salhab WA, Heyne RJ, Kendrick DE, Stoll BJ, Laptook AR, et al. Outcome of extremely low birth weight infants who received delivery room cardiopulmonary resuscitation. J Pediatr. 2012; 160:239–44.
Article42. Sawyer T, Lee HC, Aziz K. Anticipation and preparation for every delivery room resuscitation. In : In: proceeding of Seminars in Fetal and Neonatal Medicine; 2018. Elsevier.
Article43. Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010; 304:992–1000.
Article44. In : Mellander M, editor. Perinatal management, counselling and outcome of fetuses with congenital heart disease. In: proceeding of Seminars in Fetal and Neonatal Medicine; 2005. Elsevier.
Article45. Draper E, Kurinczuk J, Kenyon S. MBRRACE-UK 2017 perinatal confidential enquiry: term, singleton, intrapartum stillbirth and intrapartum-related neonatal death. Leicester: The Infant Mortality and Morbidity Studies, Department of Health Sciences, University of Leicester;2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of Intact Cord Resuscitation
- Initial Resuscitation at Delivery and Short Term Neonatal Outcomes in Very-Low-Birth-Weight Infants
- The Author's Response: Compression Rate during Cardiopulmonary Resuscitation
- Liver Laceration with Hemoperitoneum after Cardiopulmonary Resuscitation
- Cardiac Arrest Due to Unrecognized Congenital Diaphragmatic Hernia