Acute Crit Care.
2022 Aug;37(3):312-321. 10.4266/acc.2022.00136.
Risk factors associated with development of coinfection in critically Ill patients with COVID-19
- Affiliations
-
- 1Department of Critical Care, Cleveland Clinic, Cleveland, OH, USA
- 2Department of Pharmacy, Cleveland Clinic, Cleveland, OH, USA
- 3Department of Quantitative Health Sciences, Cleveland Clinic, Cleveland, OH, USA
- 4Department of Anesthesiology and Critical Care, Memorial Sloan Kettering Cancer Center, New York, NY, USA
- KMID: 2535294
- DOI: http://doi.org/10.4266/acc.2022.00136
Abstract
- Background
At outset of the coronavirus disease 2019 (COVID-19) pandemic, the significance of bacterial and fungal coinfections in individuals with COVID-19 was unknown. Initial reports indicated that the prevalence of coinfection in the general population was low, but there was uncertainty regarding the risk of coinfection in critically ill patients.
Methods
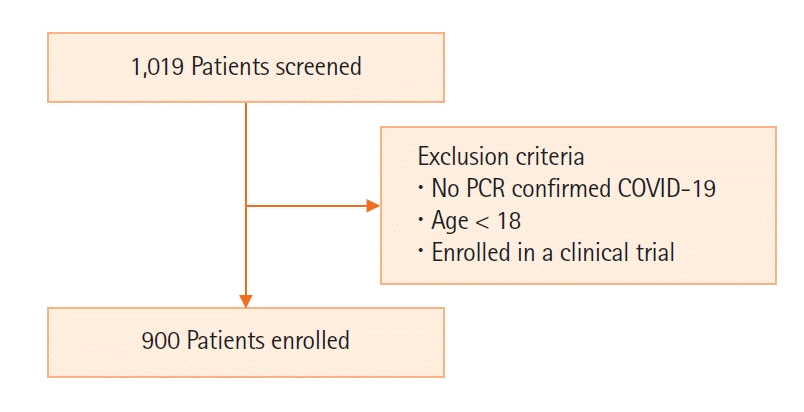
Nine hundred critically ill adult patients with COVID-19 infection were enrolled in this observational case-control study. Patients with a coinfection (case) and patients without a coinfection (control) were compared using univariate and multivariable analyses. A subgroup analysis was performed on patients with coinfection, dividing them into early (infection within 7 days) and late (infection after 7 days) infection groups.
Results
Two hundred and thirty-three patients (25.9%) had a bacterial or fungal coinfection. Vasopressor use (P<0.001) and severity of illness (higher Acute Physiology and Chronic Health Evaluation III score, P=0.009) were risk factors for the development of a coinfection. Patients with coinfection had higher mortality and length of stay. Vasopressor and corticosteroid use and central line and foley catheter placement were risk factors for late infection (>7 days). There were high rates of drug-resistant infections.
Conclusions
Critically ill patients with COVID-19 are at risk for both community-acquired and hospital-acquired infections throughout their hospitalization for COVID-19. It is important to consider the development of a coinfection in clinically worsening critically ill patients with COVID-19 and consider the likelihood of drug-resistance when choosing an empiric regimen.
Figure
Reference
-
1. Johns Hopkins University and Medicine. COVID-19 Map: Johns Hopkins coronavirus resource center [Internet]. Baltimore (MD): Johns Hopkins University and Medicine;2021. [cited 2022 May 3]. Available from: https://coronavirus.jhu.edu/map.html.2. Metersky ML, Masterton RG, Lode H, File TM Jr, Babinchak T. Epidemiology, microbiology, and treatment considerations for bacterial pneumonia complicating influenza. Int J Infect Dis. 2012; 16:e321–31.3. Bakaletz LO. Viral-bacterial co-infections in the respiratory tract. Curr Opin Microbiol. 2017; 35:30–5.4. Hughes S, Troise O, Donaldson H, Mughal N, Moore L. Bacterial and fungal coinfection among hospitalized patients with COVID-19: a retrospective cohort study in a UK secondary-care setting. Clin Microbiol Infect. 2020; 26:1395–9.5. Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021; 27:83–8.6. Karaba SM, Jones G, Helsel T, Smith LL, Avery R, Dzintars K, et al. Prevalence of co-infection at the time of hospital admission in COVID-19 patients, a multicenter study. Open Forum Infect Dis. 2020; 8:ofaa578.7. Youngs J, Wyncoll D, Hopkins P, Arnold A, Ball J, Bicanic T. Improving antibiotic stewardship in COVID-19: Bacterial co-infection is less common than with influenza. J Infect. 2020; 81:e55–7.8. Sepulveda J, Westblade LF, Whittier S, Satlin MJ, Greendyke WG, Aaron JG, et al. Bacteremia and blood culture utilization during COVID-19 surge in New York City. J Clin Microbiol. 2020; 58:e00875–20.9. Rawson TM, Moore L, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020; 71:2459–68.10. Bhatt PJ, Shiau S, Brunetti L, Xie Y, Solanki K, Khalid S, et al. Risk factors and outcomes of hospitalized patients with severe coronavirus disease 2019 (COVID-19) and secondary bloodstream infections: a multicenter case-control study. Clin Infect Dis. 2021; 72:e995–1003.11. Sharifipour E, Shams S, Esmkhani M, Khodadadi J, Fotouhi-Ardakani R, Koohpaei A, et al. Evaluation of bacterial co-infections of the respiratory tract in COVID-19 patients admitted to ICU. BMC Infect Dis. 2020; 20:646.12. Zhang H, Zhang Y, Wu J, Li Y, Zhou X, Li X, et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect. 2020; 9:1958–64.13. Baskaran V, Lawrence H, Lansbury LE, Webb K, Safavi S, Zainuddin NI, et al. Co-infection in critically ill patients with COVID-19: an observational cohort study from England. J Med Microbiol. 2021; 70:001350.
Article14. d'Humières C, Patrier J, Lortat-Jacob B, Tran-Dinh A, Chemali L, Maataoui N, et al. Two original observations concerning bacterial infections in COVID-19 patients hospitalized in intensive care units during the first wave of the epidemic in France. PLoS One. 2021; 16:e0250728.15. Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020; 81:266–75.
Article16. Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020; 26:1622–9.
Article17. Chang CY, Chan KG. Underestimation of co-infections in COVID-19 due to non- discriminatory use of antibiotics. J Infect. 2020; 81:e29–30.18. Han J, Gatheral T, Williams C. Procalcitonin for patient stratification and identification of bacterial co-infection in COVID-19. Clin Med (Lond). 2020; 20:e47.
Article19. Vanhomwegen C, Veliziotis I, Malinverni S, Konopnicki D, Dechamps P, Claus M, et al. Procalcitonin accurately predicts mortality but not bacterial infection in COVID-19 patients admitted to intensive care unit. Ir J Med Sci. 2021; 190:1649–52.
Article20. Loke HY, Kyaw WM, Chen M, Lim JW, Ang B, Chow A. Length of stay and odds of MRSA acquisition: a dose-response relationship? Epidemiol Infect. 2019; 147:e223.
Article21. Tess BH, Glenister HM, Rodrigues LC, Wagner MB. Incidence of hospital-acquired infection and length of hospital stay. Eur J Clin Microbiol Infect Dis. 1993; 12:81–6.
Article22. Stekhoven DJ, Bühlmann P. MissForest: non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012; 28:112–8.
Article23. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18:268–81.
Article24. Cleveland Clinic Foundation. Cumulative antimicrobial susceptibility of bacteria from cultures at CCF main campus. Cleveland: Cleveland Clinic Intranet.25. Nasir N, Rehman F, Omair SF. Risk factors for bacterial infections in patients with moderate to severe COVID-19: a case-control study. J Med Virol. 2021; 93:4564–9.
Article26. Klein EY, Monteforte B, Gupta A, Jiang W, May L, Hsieh YH, et al. The frequency of influenza and bacterial coinfection: a systematic review and meta-analysis. Influenza Other Respir Viruses. 2016; 10:394–403.
Article27. RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021; 384:693–704.
Article28. George MD, Baker JF, Winthrop K, Hsu JY, Wu Q, Chen L, et al. Risk for serious infection with low-dose glucocorticoids in patients with rheumatoid arthritis : a cohort study. Ann Intern Med. 2020; 173:870–8.
Article29. Obata R, Maeda T, Rizk D, Kuno T. Increased secondary infection in COVID-19 patients treated with steroids in New York City. Jpn J Infect Dis. 2021; 74:307–15.
Article30. Bassetti M, Kollef MH, Timsit JF. Bacterial and fungal superinfections in critically ill patients with COVID-19. Intensive Care Med. 2020; 46:2071–4.
Article31. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020; 323:1545–6.
Article32. Heesom L, Rehnberg L, Nasim-Mohi M, Jackson A, Celinski M, Dushianthan A, et al. Procalcitonin as an antibiotic stewardship tool in COVID-19 patients in the intensive care unit. J Glob Antimicrob Resist. 2020; 22:782–4.
Article33. Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020; 505:190–1.
Article34. Huang I, Pranata R, Lim MA, Oehadian A, Alisjahbana B. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis. 2020; 14:1753466620937175.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Critically Ill COVID-19 Patients in Busan, Republic of Korea
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea
- How We Have Treated Severe to Critically Ill Patients With Coronavirus Disease 2019 in Korea
- Comparison of critically ill COVID-19 and influenza patients with acute respiratory failure
- Treatment of Critically Ill Patients with Coronavirus Disease 2019