Ewha Med J.
2022 Oct;45(4):e8. 10.12771/emj.2022.e8.
Update on Diagnosis and Treatment of Colorectal Cancer
- Affiliations
-
- 1Department of Colon and Rectal Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2534746
- DOI: http://doi.org/10.12771/emj.2022.e8
Abstract
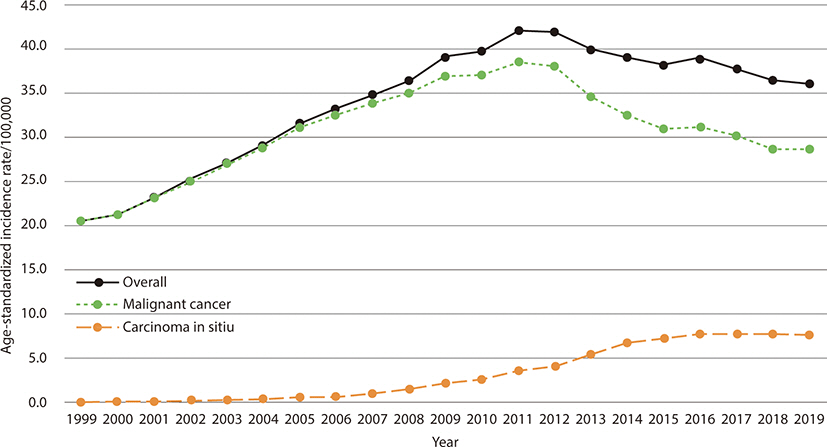
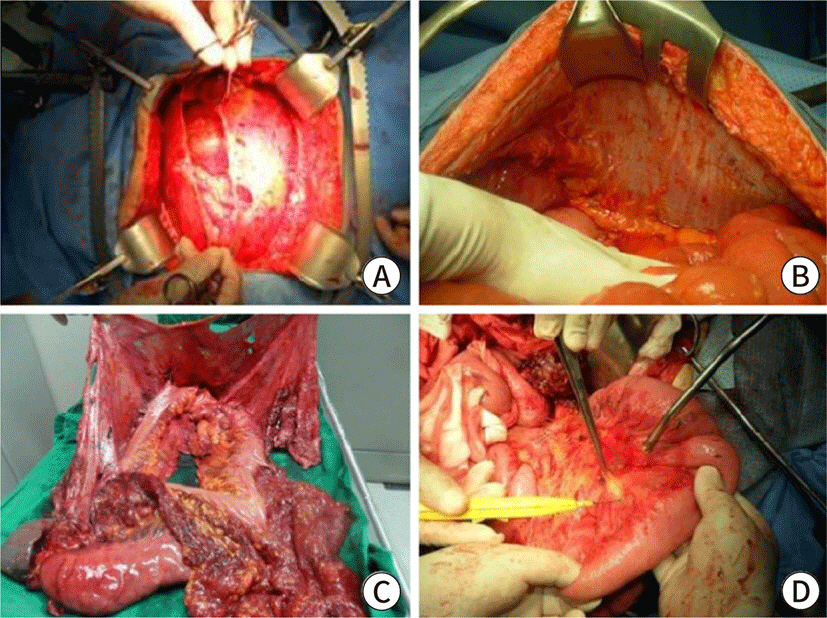
- The rate of colorectal cancer (CRC) has altered. Early-onset CRC patients are increasing, and it is one of the main causes of cancer-related death. Based on epidemiologic change, the CRC screening program needs to be changed. To increase compliance, non-invasive screening techniques are developed. Although CRC survival has increased, the oncologic prognosis of metastatic CRC is remains poor. Even in metastatic CRC, which is the most difficult to treat, attempts are being made to increase the survival rate by active surgical therapy with the creation of chemotherapeutic regimens and targeted treatment based on genomic information. Due to the introduction of aggressive chemotherapy regimens, targeted therapy based on genomic features, and improvements in surgical technique, the role of surgical treatment in metastatic CRC has expanded. Metastatic CRC surgery was indicated for liver, lung, and even peritoneal seeding. Local ablation therapy was also effectively used for liver and lung metastasis. Cytoreductive surgery and intraperitoneal chemotherapy were tried for peritoneal seeding and demonstrated good results in a subgroup of patients, although the right indication was carefully assessed. At the same time, one of the key goals of treatment for CRC was to maintain functional outcomes. Neoadjuvant treatment, in particular, helped rectal cancer patients preserve functional results while maintaining oncologic safety. Rectal cancer organ preservation techniques are now being researched heavily in a variety of neoadjuvant treatment settings, including immunotherapy and whole neoadjuvant therapy. Precision medicine based on patient and disease characteristics is currently being used for the diagnosis and treatment of CRC.
Figure
Cited by 1 articles
-
Weighing the benefits of lymphadenectomy in early-stage colorectal cancer
Seung Min Baik, Ryung-Ah Lee
Ann Surg Treat Res. 2023;105(5):245-251. doi: 10.4174/astr.2023.105.5.245.
Reference
-
References
1. Kang MJ, Won YJ, Lee JJ, Jung KW, Kim HJ, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treat. 2022; 54(2):330–344. DOI: 10.4143/crt.2022.128. PMID: 35313102. PMCID: PMC9016309.
Article2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71(3):209–249. DOI: 10.3322/caac.21660. PMID: 33538338.
Article3. Nam S, Kim D, Jung K, Choi YJ, Kang JG. Analysis of the incidence and clinical features of colorectal nonadenocarcinoma in Korea: a national cancer registry-based study. Ann Coloproctol. 2020; 36(6):390–397. DOI: 10.3393/ac.2020.05.03.2. PMID: 33486908. PMCID: PMC7837402.
Article4. Lee SM, Shin JS. Colorectal cancer in octogenarian and nonagenarian patients: clinicopathological features and survivals. Ann Coloproctol. 2020; 36(5):323–329. DOI: 10.3393/ac.2020.01.19.2. PMID: 33207113. PMCID: PMC7714379.
Article5. Siegel RL, Miller KD, Sauer AG, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020; 70(3):145–164. DOI: 10.3322/caac.21601. PMID: 32133645.
Article6. Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG clinical guidelines: colorectal cancer screening 2021. Am J Gastroenterol. 2021; 116(3):458–479. DOI: 10.14309/ajg.0000000000001122. PMID: 33657038.
Article7. Sohn DK, Kim MJ, Park Y, Suh M, Shin A, Lee HY, et al. The Korean guideline for colorectal cancer screening. J Korean Med Assoc. 2015; 58(5):420–432. DOI: 10.5124/jkma.2015.58.5.420.
Article8. Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004; 351(26):2704–2714. DOI: 10.1056/NEJMoa033403. PMID: 15616205.
Article9. Alhadi SC, Zain WZW, Zahari Z, Hashim MNM, Aziz SHSA, Zakaria Z, et al. The use of M2-pyruvate kinase as a stool biomarker for detection of colorectal cancer in tertiary teaching hospital: a comparative study. Ann Coloproctol. 2020; 36(6):409–414. DOI: 10.3393/ac.2020.08.27. PMID: 32972105. PMCID: PMC7837393.
Article10. Han YD, Oh TJ, Chung TH, Jang HW, Kim YN, An S, et al. Early detection of colorectal cancer based on presence of methylated syndecan-2 (SDC2) in stool DNA. Clin Epigenetics. 2019; 11(1):51. DOI: 10.1186/s13148-019-0642-0. PMID: 30876480. PMCID: PMC6419806.11. Meester RGS, Peterse EFP, Knudsen AB, de Weerdt AC, Chen JC, Lietz AP, et al. Optimizing colorectal cancer screening by race and sex: microsimulation analysis II to inform the American Cancer Society colorectal cancer screening guideline. Cancer. 2018; 124(14):2974–2985. DOI: 10.1002/cncr.31542. PMID: 29846942. PMCID: PMC6055229.
Article12. Liang PS, Allison J, Ladabaum U, Martinez ME, Murphy CC, Schoen RE, et al. Potential intended and unintended consequences of recommending initiation of colorectal cancer screening at age 45 years. Gastroenterology. 2018; 155(4):950–954. DOI: 10.1053/j.gastro.2018.08.019. PMID: 30138614.
Article13. Mannucci A, Zuppardo RA, Rosati R, Leo MD, Perea J, Cavestro GM. Colorectal cancer screening from 45 years of age: thesis, antithesis and synthesis. World J Gastroenterol. 2019; 25(21):2565–2580. DOI: 10.3748/wjg.v25.i21.2565. PMID: 31210710. PMCID: PMC6558439.
Article14. Imperiale TF, Kahi CJ, Rex DK. Lowering the starting age for colorectal cancer screening to 45 years: who will come… and should they? Clin Gastroenterol Hepatol. 2018; 16(10):1541–1544. DOI: 10.1016/j.cgh.2018.08.023. PMID: 30114484.
Article15. US Preventive Services Task Force. Screening for colorectal cancer US preventive services task force recommendation statement. J Am Med Assoc. 2021; 325(19):1965–1977. DOI: 10.1001/jama.2021.6238. PMID: 34003218.16. Kim YJ, Kim CH. Treatment for peritoneal metastasis of patients with colorectal cancer. Ann Coloproctol. 2021; 37(6):425–433. DOI: 10.3393/ac.2021.00920.0131. PMID: 34961304. PMCID: PMC8717073.
Article17. Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002; 235(6):759–766. DOI: 10.1097/00000658-200206000-00002. PMID: 12035031. PMCID: PMC1422504.
Article18. Torky R, Alessa M, Kim HS, Sakr A, Zakarneh E, Sauri F, et al. Characteristics of patients presented with metastases during or after completion of chemoradiation therapy for locally advanced rectal cancer: a case series. Ann Coloproctol. 2021; 37(3):186–191. DOI: 10.3393/ac.2020.08.10.1. PMID: 32972094. PMCID: PMC8273715.19. Ruers T, Punt C, Van Coevorden F, Pierie JPEN, Borel-Rinkes I, Ledermann JA, et al. Radiofrequency ablation combined with systemic treatment versus systemic treatment alone in patients with non-resectable colorectal liver metastases: a randomized EORTC Intergroup phase II study (EORTC 40004). Ann Oncol. 2012; 23(10):2619–2626. DOI: 10.1093/annonc/mds053. PMID: 22431703. PMCID: PMC3457746.
Article20. Chow FCL, Chok KSH. Colorectal liver metastases: an update on multidisciplinary approach. World J Hepatol. 2019; 11(2):150–172. DOI: 10.4254/wjh.v11.i2.150. PMID: 30820266. PMCID: PMC6393711.21. Sheikh S, Chen H, Sahgal A, Poon I, Erler D, Badellino S, et al. An analysis of a large multi-institutional database reveals important associations between treatment parameters and clinical outcomes for stereotactic body radiotherapy (SBRT) of oligometastatic colorectal cancer. Radiother Oncol. 2022; 167:187–194. DOI: 10.1016/j.radonc.2021.12.018. PMID: 34952002.
Article22. Nakamura Y, Hokuto D, Koyama F, Matsuo Y, Nomi T, Yoshikawa T, et al. The prognosis and recurrence pattern of right- and left-sided colon cancer in stage II, stage III, and liver metastasis after curative resection. Ann Coloproctol. 2021; 37(5):326–336. DOI: 10.3393/ac.2020.09.14. PMID: 32972100. PMCID: PMC8566149.
Article23. Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002; 235(6):759–766. DOI: 10.1097/00000658-200206000-00002. PMID: 12035031. PMCID: PMC1422504.
Article24. Park SH, Shin JK, Lee WY, Yun SH, Cho YB, Huh JW, et al. Clinical outcomes of neoadjuvant chemotherapy in colorectal cancer patients with synchronous resectable liver ketastasis: a propensity score matching analysis. Ann Coloproctol. 2021; 37(4):244–252. DOI: 10.3393/ac.2020.00710.0101. PMID: 34182620. PMCID: PMC8391040.
Article25. Sandström P, Røsok BI, Sparrelid E, Larsen PN, Larsson AL, Lindell G, et al. ALPPS improves resectability compared with conventional two-stage hepatectomy in patients with advanced colorectal liver metastasis: results from a Scandinavian multicenter randomized controlled trial (LIGRO trial). Ann Surg. 2018; 267(5):833–840. DOI: 10.1097/SLA.0000000000002511. PMID: 28902669. PMCID: PMC5916470.
Article26. Hasselgren K, Røsok BI, Larsen PN, Sparrelid E, Lindell G, Schultz NA, et al. ALPPS improves survival compared with TSH in patients affected of CRLM: survival analysis from the randomized controlled trial LIGRO. Ann Surg. 2021; 273(3):442–448. DOI: 10.1097/SLA.0000000000003701. PMID: 32049675.27. Vallance AE, van der Meulen J, Kuryba A, Charman SC, Botterill ID, Prasad KR, et al. The timing of liver resection in patients with colorectal cancer and synchronous liver metastases: a population-based study of current practice and survival. Colorectal Dis. 2018; 20(6):486–495. DOI: 10.1111/codi.14019. PMID: 29338108.
Article28. Slesser AAP, Simillis C, Goldin R, Brown G, Mudan S, Tekkis PP. A meta-analysis comparing simultaneous versus delayed resections in patients with synchronous colorectal liver metastases. Surg Oncol. 2013; 22(1):36–47. DOI: 10.1016/j.suronc.2012.11.002. PMID: 23253399.
Article29. Brouquet A, Mortenson MM, Vauthey JN, Rodriguez-Bigas MA, Overman MJ, Chang GJ, et al. Surgical strategies for synchronous colorectal liver metastases in 156 consecutive patients: classic, combined or reverse strategy? J Am Coll Surg. 2010; 210(6):934–941. DOI: 10.1016/j.jamcollsurg.2010.02.039. PMID: 20510802.
Article30. Kim JY, Park IJ, Kim HR, Kim DK, Lee JL, Yoon YS, et al. Post-pulmonary metastasectomy prognosis after curative resection for colorectal cancer. Oncotarget. 2017; 8:36566–36577. DOI: 10.18632/oncotarget.16616. PMID: 28402263. PMCID: PMC5482677.
Article31. Pfannschmidt J, Dienemann H, Hoffmann H. Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg. 2007; 84(1):324–338. DOI: 10.1016/j.athoracsur.2007.02.093. PMID: 17588454.
Article32. Meng D, Fu L, Wang L, Dai Y, Lv W, Zhang J, et al. Video-assisted thoracoscopic surgery versus open thoracotomy in pulmonary metastasectomy: a meta-analysis of observational studies. Interact Cardiovasc Thorac Surg. 2016; 22(2):200–206. DOI: 10.1093/icvts/ivv309. PMID: 26590306.
Article33. Mitry E, Guiu B, Cosconea S, Jooste V, Faivre J, Bouvier AM. Epidemiology, management and prognosis of colorectal cancer with lung metastases: a 30-year population-based study. Gut. 2010; 59(10):1383–1388. DOI: 10.1136/gut.2010.211557. PMID: 20732912.
Article34. Roh SJ, Park SC, Choi J, Lee JS, Lee DW, Hong CW, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy with mitomycin C used for colorectal peritoneal carcinomatosis. Ann Coloproctol. 2020; 36(1):22–29. DOI: 10.3393/ac.2019.04.30. PMID: 32146785. PMCID: PMC7069674.
Article35. Goéré D, Glehen O, Quenet F, Guilloit JM, Bereder JM, Lorimier G, et al. Second-look surgery plus hyperthermic intraperitoneal chemotherapy versus surveillance in patients at high risk of developing colorectal peritoneal metastases (PROPHYLOCHIP-PRODIGE 15): a randomised, phase 3 study. Lancet Oncol. 2020; 21(9):1147–1154. DOI: 10.1016/S1470-2045(20)30322-3.
Article36. Klaver CEL, Wisselink DD, Punt CJA, Snaebjornsson P, Crezee J, Aalbers AGJ, et al. Adjuvant hyperthermic intraperitoneal chemotherapy in patients with locally advanced colon cancer (COLOPEC): a multicentre, open-label, randomised trial. Lancet Gastroenterol Hepatol. 2019; 4(10):761–770. DOI: 10.1016/S2468-1253(19)30239-0.37. Quénet F, Elias D, Roca L, Goéré D, Ghouti L, Pocard M, et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy versus cytoreductive surgery alone for colorectal peritoneal metastases (PRODIGE 7): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2021; 22(2):256–266. DOI: 10.1016/S1470-2045(20)30599-4.
Article38. Mendelaar PAJ, Smid M, van Riet J, Angus L, Labots M, Steeghs N, et al. Whole genome sequencing of metastatic colorectal cancer reveals prior treatment effects and specific metastasis features. Nat Commun. 2021; 12:3269. DOI: 10.1038/s41467-021-23629-4. PMID: 34039979. PMCID: PMC8155047.39. Varela C, Kim NK. Surgical treatment of low-lying rectal cancer: updates. Ann Coloproctol. 2021; 37(6):395–424. DOI: 10.3393/ac.2021.00927.0132. PMID: 34961303. PMCID: PMC8717072.
Article40. Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012; 30(16):1926–1933. DOI: 10.1200/JCO.2011.40.1836. PMID: 22529255.
Article41. Piozzi GN, Kim SH. Robotic intersphincteric resection for low rectal cancer: technical controversies and a systematic review on the perioperative, oncological, and functional outcomes. Ann Coloproctol. 2021; 37(6):351–367. DOI: 10.3393/ac.2021.00836.0119. PMID: 34784706. PMCID: PMC8717069.
Article42. Eldamshety O, Kotb S, Khater A, Roshdy S, Elnahas W, Zahi MS, et al. Early and late functional outcomes of anal sphincter-sparing procedures with total mesorectal excision for anorectal adenocarcinoma. Ann Coloproctol. 2020; 36(3):148–154. DOI: 10.3393/ac.2018.07.19. PMID: 32311866. PMCID: PMC7392569.
Article43. Huh JW, Maeda K, Liu Z, Wang X, Roslani AC, Lee WY. Current status of “Watch-and-Wait” rectal cancer treatment in Asia-Pacific countries. Ann Coloproctol. 2020; 36(2):70–77. DOI: 10.3393/ac.2020.01.19. PMID: 32054250. PMCID: PMC7299564.
Article44. Garcia-Aguilar J, Patil S, Kim JK, Yuval JB, Thompson H, Verheij F, et al. Preliminary results of the organ preservation of rectal adenocarcinoma (OPRA) trial. J Clin Oncol. 2020; 38:4008. DOI: 10.1200/JCO.2020.38.15_suppl.4008.
Article45. Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017; 2(7):501–513. DOI: 10.1016/S2468-1253(17)30074-2.
Article46. van der Valk MJM, Hilling DE, Bastiaannet E, Meershoek-Klein Kranenbarg E, Beets GL, Figueiredo NL, et al. Long-term outcomes of clinical complete responders after neoadjuvant treatment for rectal cancer in the International Watch & Wait Database (IWWD): an international multicentre registry study. Lancet. 2018; 391(10139):2537–2545. DOI: 10.1016/S0140-6736(18)31078-X.47. Kong JC, Guerra GR, Warrier SK, Ramsay RG, Heriot AG. Outcome and salvage surgery following "Watch and Wait" for rectal cancer after neoadjuvant therapy: a systematic review. Dis Colon Rectum. 2017; 60(3):335–345. DOI: 10.1097/DCR.0000000000000754. PMID: 28177997.
Article48. Giunta EF, Bregni G, Pretta A, Deleporte A, Liberale G, Bali AM, et al. Total neoadjuvant therapy for rectal cancer: making sense of the results from the RAPIDO and PRODIGE 23 trials. Cancer Treat Rev. 2021; 96:102177. DOI: 10.1016/j.ctrv.2021.102177. PMID: 33798955.49. Bahadoer RR, Dijkstra EA, van Etten B, Marijnen CAM, Putter H, Kranenbarg EM, et al. RAPIDO collaborative investigators. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. Lancet Oncol. 2021; 22(1):29–42. DOI: 10.1016/S1470-2045(20)30555-6.50. Oh SG, Park IJ, Seo J, Kim YI, Lim SB, Kim CW, et al. Beware of early relapse in rectal cancer patients treated with preoperative chemoradiotherapy. Ann Coloproctol. 2020; 36(6):382–389. DOI: 10.3393/ac.2020.06.11. PMID: 32674549. PMCID: PMC7837400.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic diagnosis and treatment of early colorectal cancer
- Crossroad between inflammation and carcinogenesis in colon
- Colorectal Cancer Screening and Surveillance in the Elderly: Updates and Controversies
- Influence of the COVID-19 Pandemic on the Treatment Patterns and Outcomes of Colorectal Cancer
- Direction of diagnosis and treatment improvement in colorectal cancer