J Stroke.
2022 Sep;24(3):390-395. 10.5853/jos.2022.00220.
Simplified Assessment of Lesion Water Uptake for Identification of Patients within 4.5 Hours of Stroke Onset: An Analysis of the MissPerfeCT Study
- Affiliations
-
- 1Department of Neuroradiology, Clinic of Radiology & Nuclear Medicine, University Hospital Basel, Basel, Switzerland
- 2Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 3Department of Radiology, University Hospital of Münster, Westfaelische Wilhelms-University of Münster, Münster, Germany
- 4Department of Neurology with Institute of Translational Neurology, University of Münster, Münster, Germany
- 5Department of Neurology, St. Josef-Hospital, Ruhr University Bochum, Bochum, Germany
- 6Department of Neurology, University Hospital Carl Gustav Carus, Dresden, Germany
- 7Neurovascular Center Dresden, University Hospital Carl Gustav Carus, Dresden, Germany
- 8Department of Radiology and Institute of Diagnostic and Interventional Radiology, University Medical Center Rostock, Rostock, Germany
- 9Medical Image Analysis Center (MIAC) and Department of Biomedical Engineering, University of Basel, Basel, Switzerland
- 10Institute for Stroke and Dementia Research (ISD), University Hospital, LMU Munich, Munich, Germany
- 11Institute of Neuroradiology, University Hospital Carl Gustav Carus, Dresden, Germany
- 12Department of Radiology, German Cancer Research Center, Heidelberg, Germany
- 13Department of Radiology, University Hospital, LMU Munich, Munich, Germany
- 14Department of Neuroradiology, University Medical Center Schleswig-Holstein, Lübeck, Germany
- 15Institute of Epidemiology and Social Medicine, University of Münster, Münster, Germany
- 16Department of Diagnostic and Interventional Neuroradiology, University Medical Center Marburg, Marburg University, Marburg, Germany
- KMID: 2534268
- DOI: http://doi.org/10.5853/jos.2022.00220
Abstract
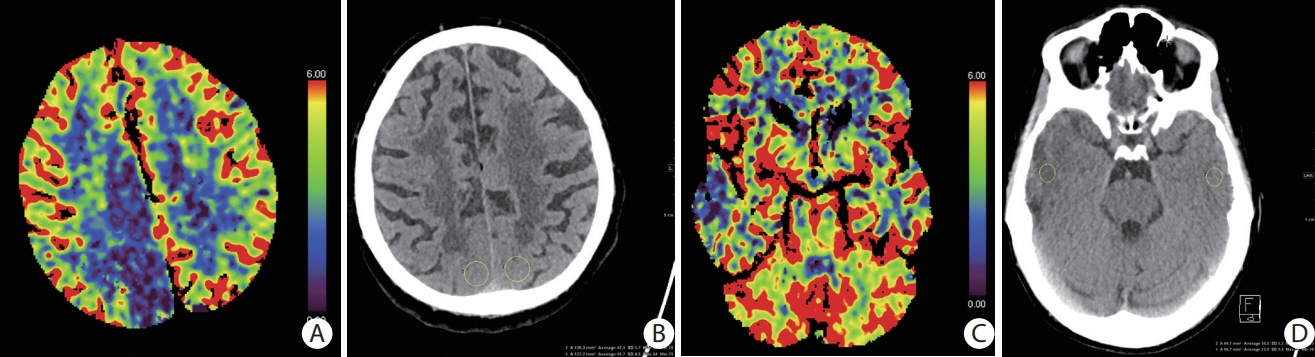
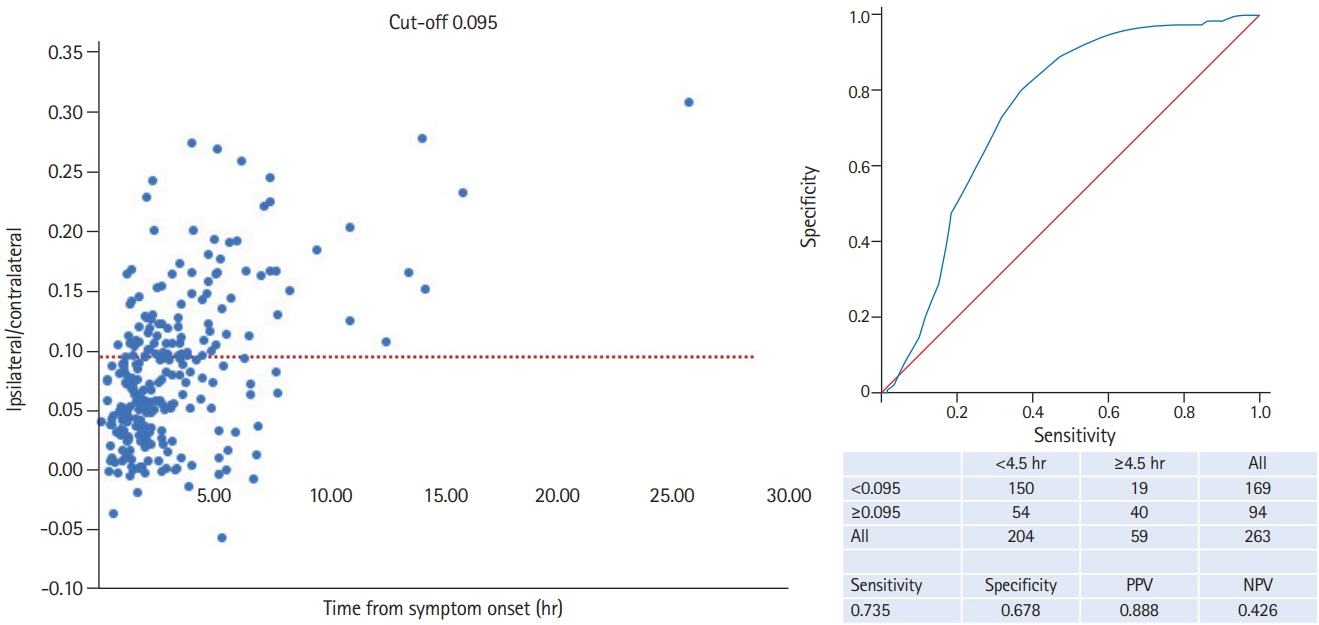
- Background and Purpose
Many patients with stroke cannot receive intravenous thrombolysis because the time of symptom onset is unknown. We tested whether a simple method of computed tomography (CT)-based quantification of water uptake in the ischemic tissue can identify patients with stroke onset within 4.5 hours. Methods This retrospective analysis of the MissPerfeCT study (August 2009 to November 2017) includes consecutive patients with known onset of symptoms from seven tertiary stroke centers. We developed a simplified algorithm based on region of interest (ROI) measurements to quantify water uptake of the ischemic lesion and thereby quantify time of symptom onset within and beyond 4.5 hours. Perfusion CT was used to identify ischemic brain tissue, and its density was measured in non-contrast CT and related to the density of the corresponding area of the contralateral hemisphere to quantify lesion water uptake. Results Of 263 patients, 204 (77.6%) had CT within 4.5 hours. Water uptake was significantly lower in patients with stroke onset within (6.7%; 95% confidence interval [CI], 6.0% to 7.4%) compared to beyond 4.5 hours (12.7%; 95% CI, 10.7% to 14.7%). The area under the curve for distinguishing these patient groups according to percentage water uptake was 0.744 with an optimal cut-off value of 9.5%. According to this cut-off the positive predictive value was 88.8%, sensitivity was 73.5%, specificity 67.8%, negative predictive value was 42.6%. Conclusions Ischemic stroke patients with unknown time of symptom onset can be identified as being within a timeframe of 4.5 hours using a ROI-based method to assess water uptake on admission non-contrast head CT.
Keyword
Figure
Reference
-
References
1. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384:1929–1935.2. Fink JN, Kumar S, Horkan C, Linfante I, Selim MH, Caplan LR, et al. The stroke patient who woke up: clinical and radiological features, including diffusion and perfusion MRI. Stroke. 2002; 33:988–993.3. Ma H, Campbell BC, Parsons MW, Churilov L, Levi CR, Hsu C, et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019; 380:1795–1803.4. Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 2018; 379:611–622.5. Scheldeman L, Wouters A, Boutitie F, Dupont P, Christensen S, Cheng B, et al. Different mismatch concepts for magnetic resonance imaging-guided thrombolysis in unknown onset stroke. Ann Neurol. 2020; 87:931–938.6. Minnerup J, Broocks G, Kalkoffen J, Langner S, Knauth M, Psychogios MN, et al. Computed tomography-based quantification of lesion water uptake identifies patients within 4.5 hours of stroke onset: a multicenter observational study. Ann Neurol. 2016; 80:924–934.7. Kemmling A, Flottmann F, Forkert ND, Minnerup J, Heindel W, Thomalla G, et al. Multivariate dynamic prediction of ischemic infarction and tissue salvage as a function of time and degree of recanalization. J Cereb Blood Flow Metab. 2015; 35:1397–1405.8. Thomalla G, Cheng B, Ebinger M, Hao Q, Tourdias T, Wu O, et al. DWI-FLAIR mismatch for the identification of patients with acute ischaemic stroke within 4·5 h of symptom onset (PRE-FLAIR): a multicentre observational study. Lancet Neurol. 2011; 10:978–986.9. Breuer L, Schellinger PD, Huttner HB, Halwachs R, Engelhorn T, Doerfler A, et al. Feasibility and safety of magnetic resonance imaging-based thrombolysis in patients with stroke on awakening: initial single-centre experience. Int J Stroke. 2010; 5:68–73.10. Aoki J, Kimura K, Iguchi Y, Shibazaki K, Iwanaga T, Watanabe M, et al. Intravenous thrombolysis based on diffusion-weighted imaging and fluid-attenuated inversion recovery mismatch in acute stroke patients with unknown onset time. Cerebrovasc Dis. 2011; 31:435–441.11. Dzialowski I, Weber J, Doerfler A, Forsting M, von Kummer R. Brain tissue water uptake after middle cerebral artery occlusion assessed with CT. J Neuroimaging. 2004; 14:42–48.12. Campbell BC, Ma H, Ringleb PA, Parsons MW, Churilov L, Bendszus M, et al. Extending thrombolysis to 4·5-9 h and wakeup stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet. 2019; 394:139–147.13. Broocks G, Leischner H, Hanning U, Flottmann F, Faizy TD, Schön G, et al. Lesion age imaging in acute stroke: water uptake in CT versus DWI-FLAIR mismatch. Ann Neurol. 2020; 88:1144–1152.14. Psychogios MN, Sporns PB, Ospel J, Katsanos AH, Kabiri R, Flottmann FA, et al. Automated perfusion calculations vs. visual scoring of collaterals and CBV-ASPECTS: has the machine surpassed the eye? Clin Neuroradiol. 2021; 31:499–506.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Visibility of CT Early Ischemic Change Is Significantly Associated with Time from Stroke Onset to Baseline Scan beyond the First 3 Hours of Stroke Onset
- Clinical Features of Patients with False Negative Diffusion-weighted MR Findings in Acute Ischemic Stroke
- Outcome Evaluation of Intravenous Infusion of Urokinase for Acute Ischemic Stroke
- Availability of Multimarker IndexTM in Prediction of Ischemic Stroke Severity
- Ischemic Lesion Water Uptake in Acute Stroke: Is Blood Glucose Related to Cause and Effect?