J Liver Cancer.
2022 Sep;22(2):194-201. 10.17998/jlc.2022.08.24.
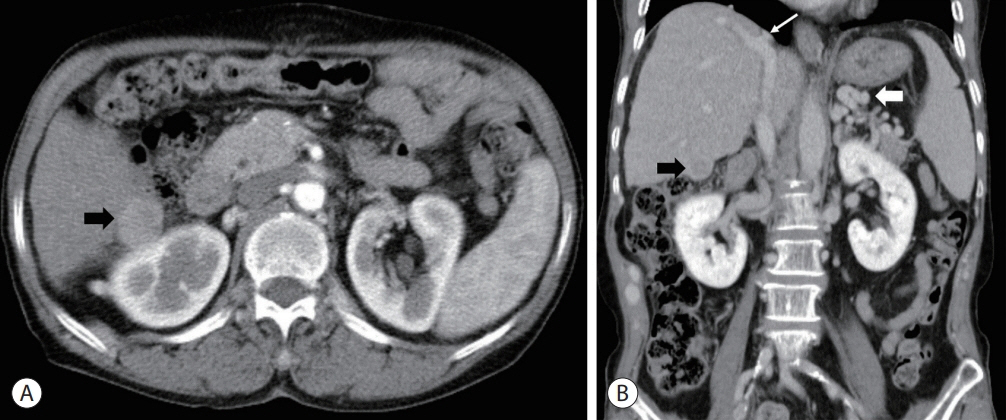
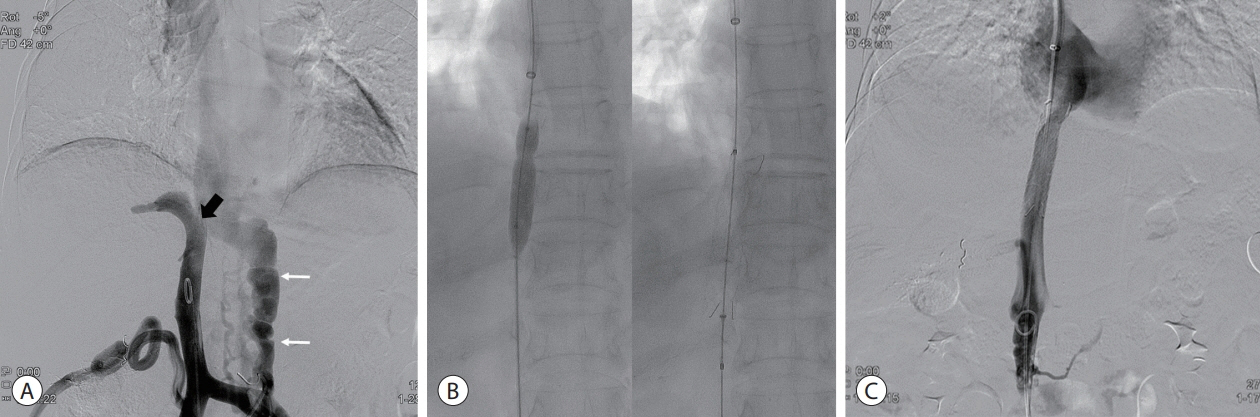
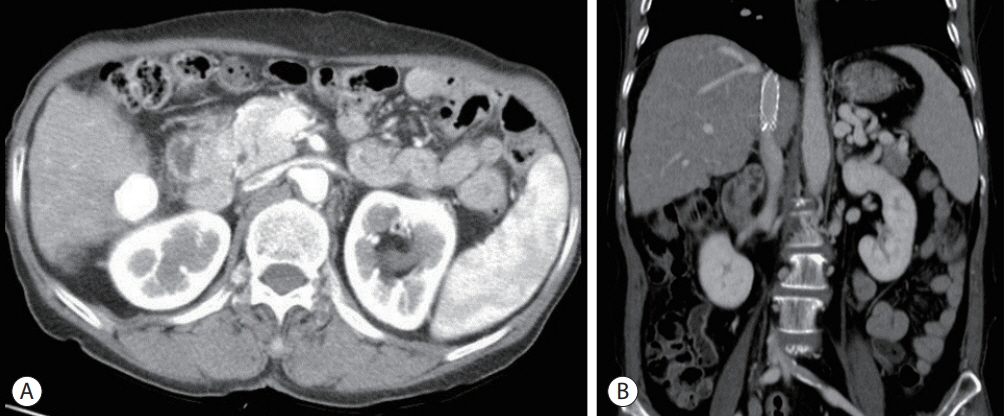
Hepatocellular carcinoma with Budd-Chiari syndrome due to membranous obstruction of the inferior vena cava with long-term follow-up: a case report
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 3Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Department of General Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2534247
- DOI: http://doi.org/10.17998/jlc.2022.08.24
Abstract
- Membranous obstruction of the inferior vena cava (MOVC) is a rare subset of Budd-Chiari syndrome (BCS) with a subacute onset that is often complicated by cirrhosis and hepatocellular carcinoma (HCC). Here we report a case of recurrent HCC in a patient with cirrhosis and BCS that was treated with several episodes of transarterial chemoembolization followed by surgical tumorectomy, whereas the MOVC was successfully treated with balloon angioplasty followed by endovascular stenting. The patient was followed up for 9.9 years without anticoagulation and experienced no stent thrombosis. After the tumorectomy, the patient was HCC-free for 4.4 years of follow-up.
Keyword
Figure
Reference
-
1. Ludwig J, Hashimoto E, McGill DB, van Heerden JA. Classification of hepatic venous outflow obstruction: ambiguous terminology of the Budd-Chiari syndrome. Mayo Clin Proc. 1990; 65:51–55.2. Shukla A, Shreshtha A, Mukund A, Bihari C, Eapen CE, Han G, et al. Budd-Chiari syndrome: consensus guidance of the Asian Pacific Association for the study of the liver (APASL). Hepatol Int. 2021; 15:531–567.3. Matsui S, Ichida T, Watanabe M, Sugitani S, Suda T, Takahashi T, et al. Clinical features and etiology of hepatocellular carcinoma arising in patients with membranous obstruction of the inferior vena cava: in reference to hepatitis viral infection. J Gastroenterol Hepatol. 2000; 15:1205–1211.4. Okuda K. Inferior vena cava thrombosis at its hepatic portion (obliterative hepatocavopathy). Semin Liver Dis. 2002; 22:15–26.5. Okuda K, Kage M, Shrestha SM. Proposal of a new nomenclature for Budd-Chiari syndrome: hepatic vein thrombosis versus thrombosis of the inferior vena cava at its hepatic portion. Hepatology. 1998; 28:1191–1198.6. Simson IW. Membranous obstruction of the inferior vena cava and hepatocellular carcinoma in South Africa. Gastroenterology. 1982; 82:171–178.7. Kew MC, Hodkinson HJ. Membranous obstruction of the inferior vena cava and its causal relation to hepatocellular carcinoma. Liver Int. 2006; 26:1–7.8. Shrestha SM. Liver cirrhosis in hepatic vena cava syndrome (or membranous obstruction of inferior vena cava). World J Hepatol. 2015; 7:874–884.9. Lim JH, Park JH, Auh YH. Membranous obstruction of the inferior vena cava: comparison of findings at sonography, CT, and venography. AJR Am J Roentgenol. 1992; 159:515–520.10. Okuda K. Membranous obstruction of the inferior vena cava (obliterative hepatocavopathy, Okuda). J Gastroenterol Hepatol. 2001; 16:1179–1183.11. Valla DC. Budd-Chiari syndrome/hepatic venous outflow tract obstruction. Hepatol Int. 2018; 12(Suppl 1):168–180.12. Wu T, Wang L, Xiao Q, Wang B, Li S, Li X, et al. Percutaneous balloon angioplasty of inferior vena cava in Budd-Chiari syndromeR1. Int J Cardiol. 2002; 83:175–178.13. Lee BB, Villavicencio L, Kim YW, Do YS, Koh KC, Lim HK, et al. Primary Budd-Chiari syndrome: outcome of endovascular management for suprahepatic venous obstruction. J Vasc Surg. 2006; 43:101–108.14. Takamura M, Ichida T, Yokoyama J, Matsuda Y, Nomoto M, Aoyagi Y. Recurrence of hepatocellular carcinoma 102 months after successful eradication and removal of membranous obstruction of the inferior vena cava. J Gastroenterol. 2004; 39:681–684.15. Gwon D 2nd, Ko GY, Yoon HK, Sung KB, Kim JH, Lee SS, et al. Hepatocellular carcinoma associated with membranous obstruction of the inferior vena cava: incidence, characteristics, and risk factors and clinical efficacy of TACE. Radiology. 2010; 254:617–626.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Budd-Chiari syndrome caused by membranous obstruction of inferior vena cava
- A Case of Budd Chiari Syndrome Caused by Membraneous Obstruction of Suprahepatic Inferior Vena Cava
- Mesoatrial Shunt Operation for Treatment of Budd-Chiari Syndrome: A case report
- Multidisciplinary approach for hepatocellular carcinoma arising from cirrhotic liver with Budd-Chiari syndrome: a case report
- Balloon Angioplasty for Budd-Chiari Syndrome Resulting from Primary Repair of an Inferior Vena Cava Injury