Korean J Pain.
2022 Oct;35(4):475-487. 10.3344/kjp.2022.35.4.475.
Actual situation and prescribing patterns of opioids by pain physicians in South Korea
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea
- 3Department of Anesthesiology and Pain Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
- 4Department of Anesthesiology and Pain Medicine, Jeong-clinic, Seoul, Korea
- 5Department of Anesthesiology and Pain Medicine, Inje University Seoul Paik Hospital, Seoul, Korea
- 6Department of Anesthesiology and Pain Medicine, Jeju National University School of Medicine, Jeju, Korea
- 7Department of Anesthesiology and Pain Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- KMID: 2533988
- DOI: http://doi.org/10.3344/kjp.2022.35.4.475
Abstract
- Background
Use of opioids for chronic intractable pain is increasing globally, and their proper use can improve patients’ quality of life. In contrast, opioid use disorders, such as abuse or addiction, caused by prescribing opioids, are a worldwide issue. This study aimed to understand current opioid prescribing patterns and pain physicians’ experiences with opioid use in South Korea.
Methods
Pain physicians in 42 university hospitals in South Korea were asked to complete anonymous questionnaires regarding opioid prescriptions.
Results
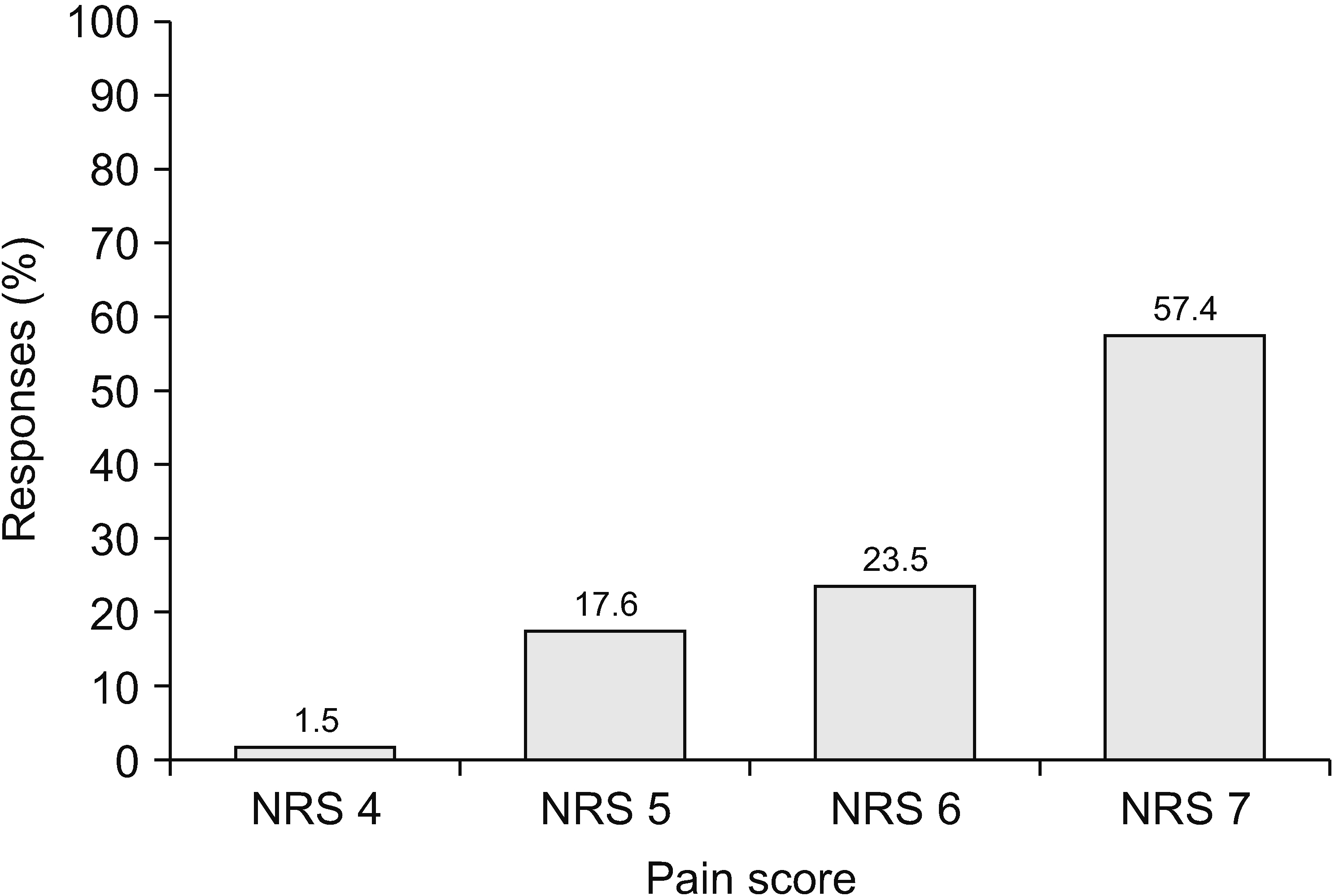
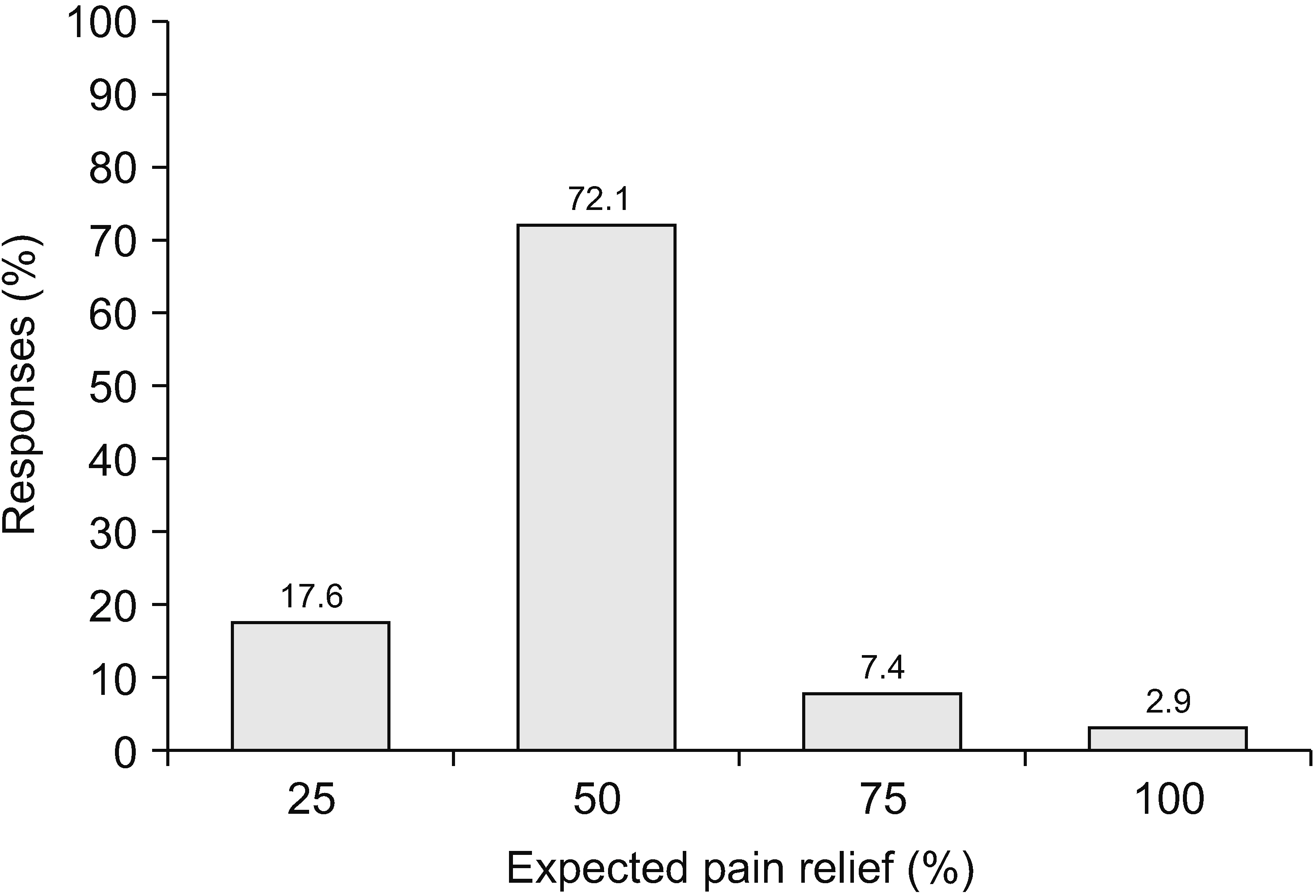
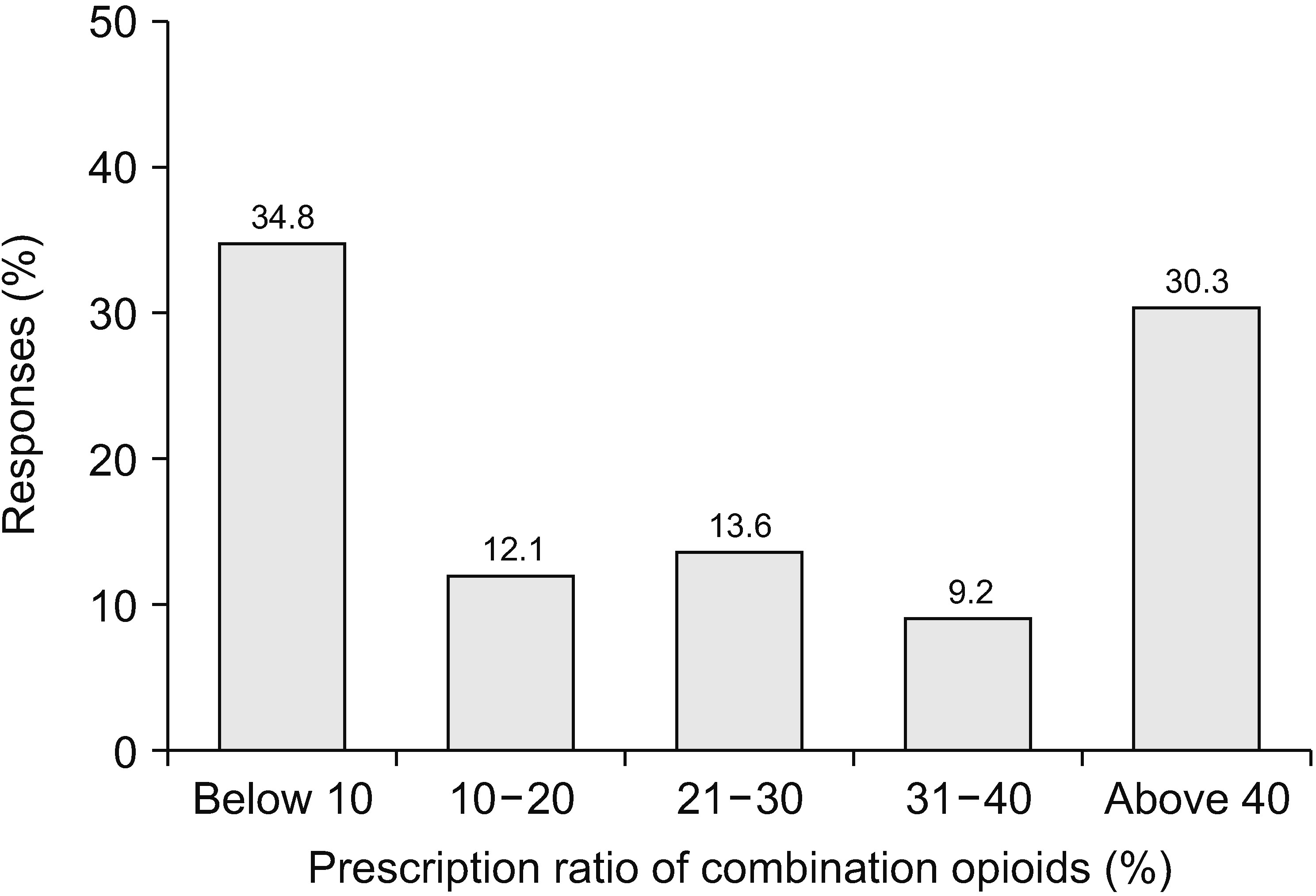
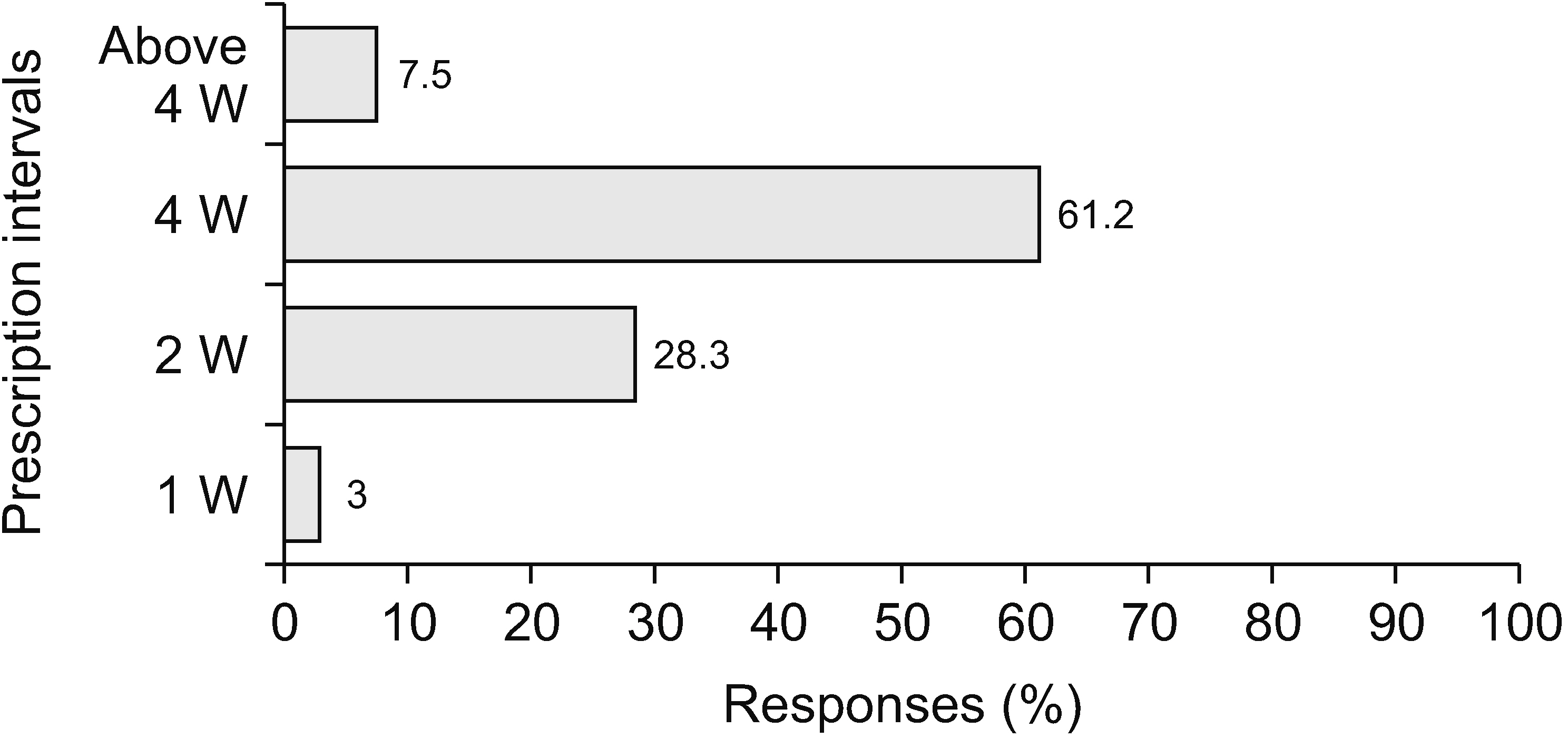
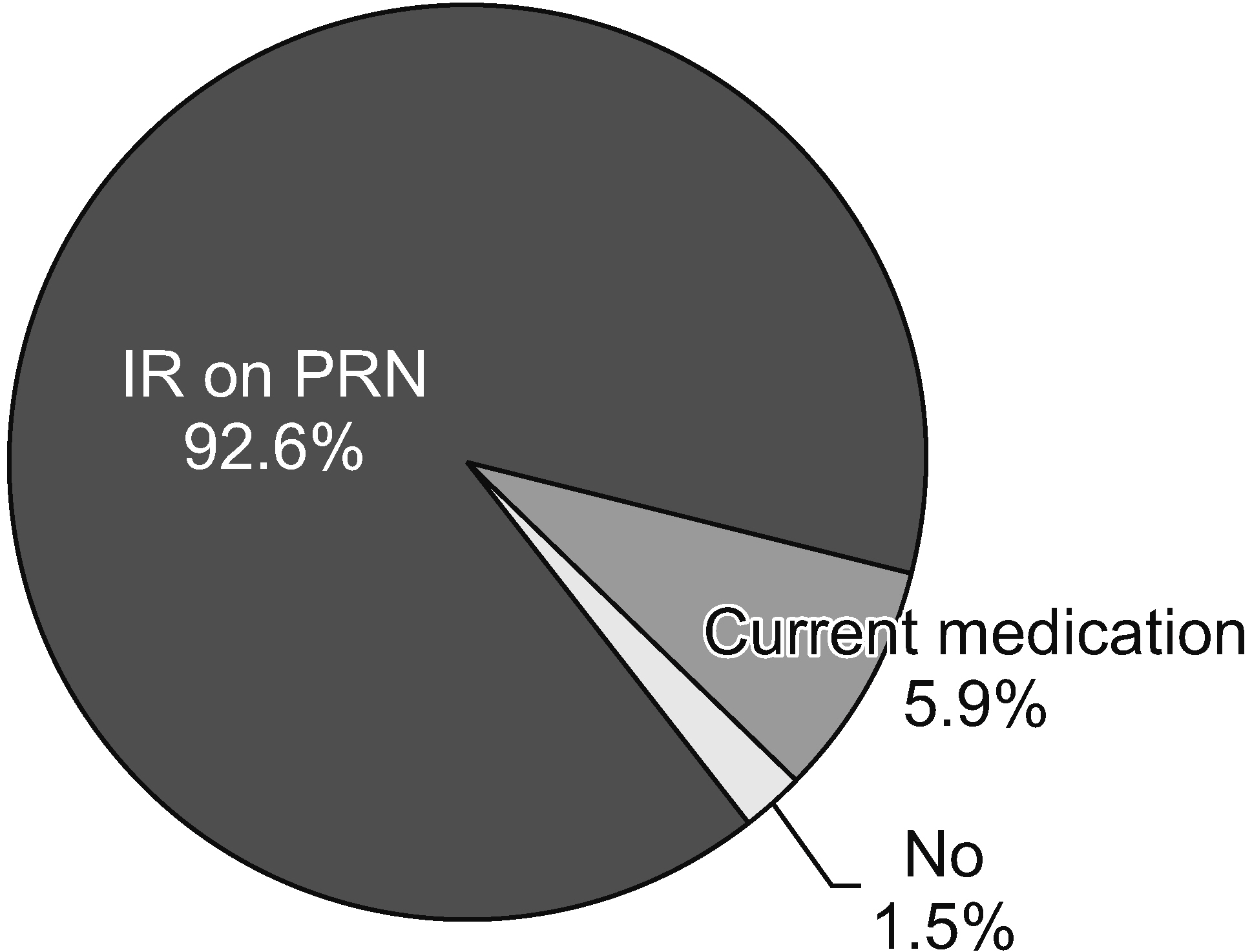
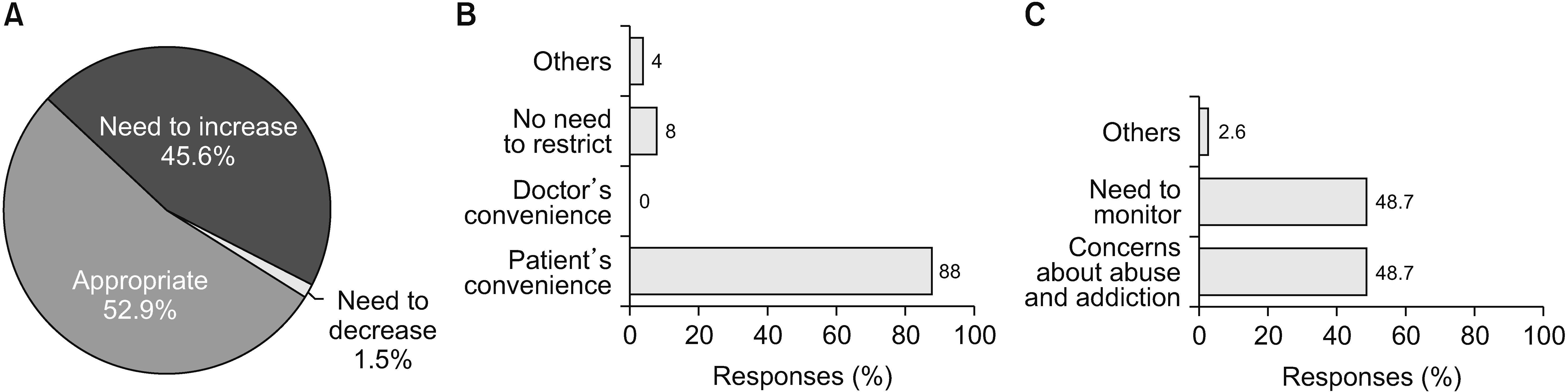
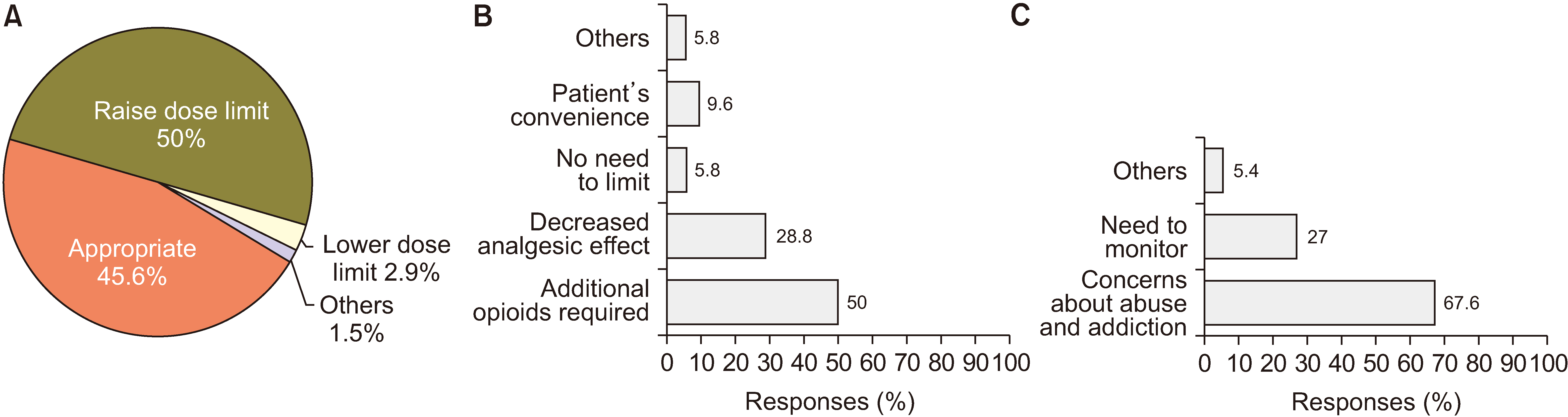
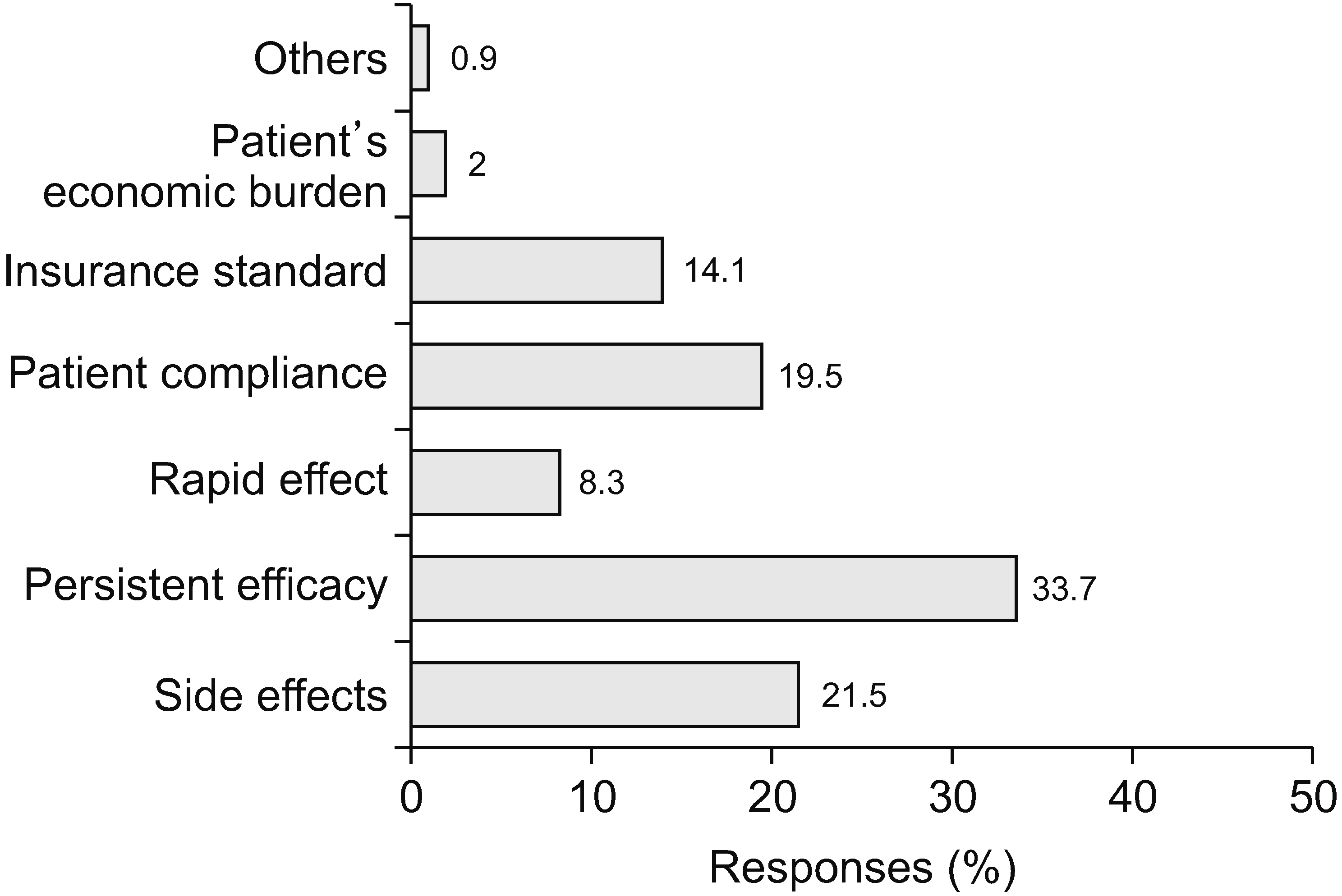
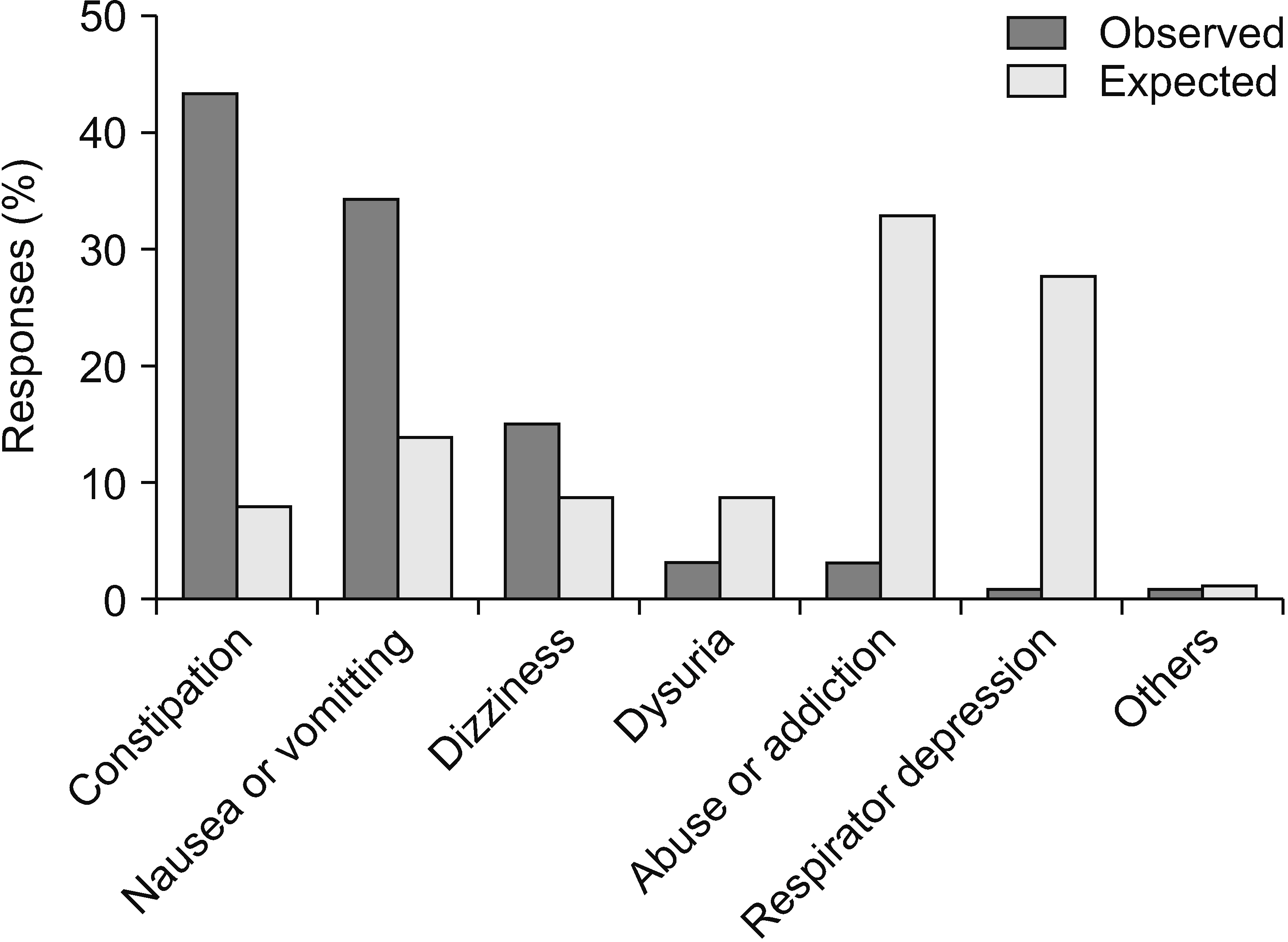
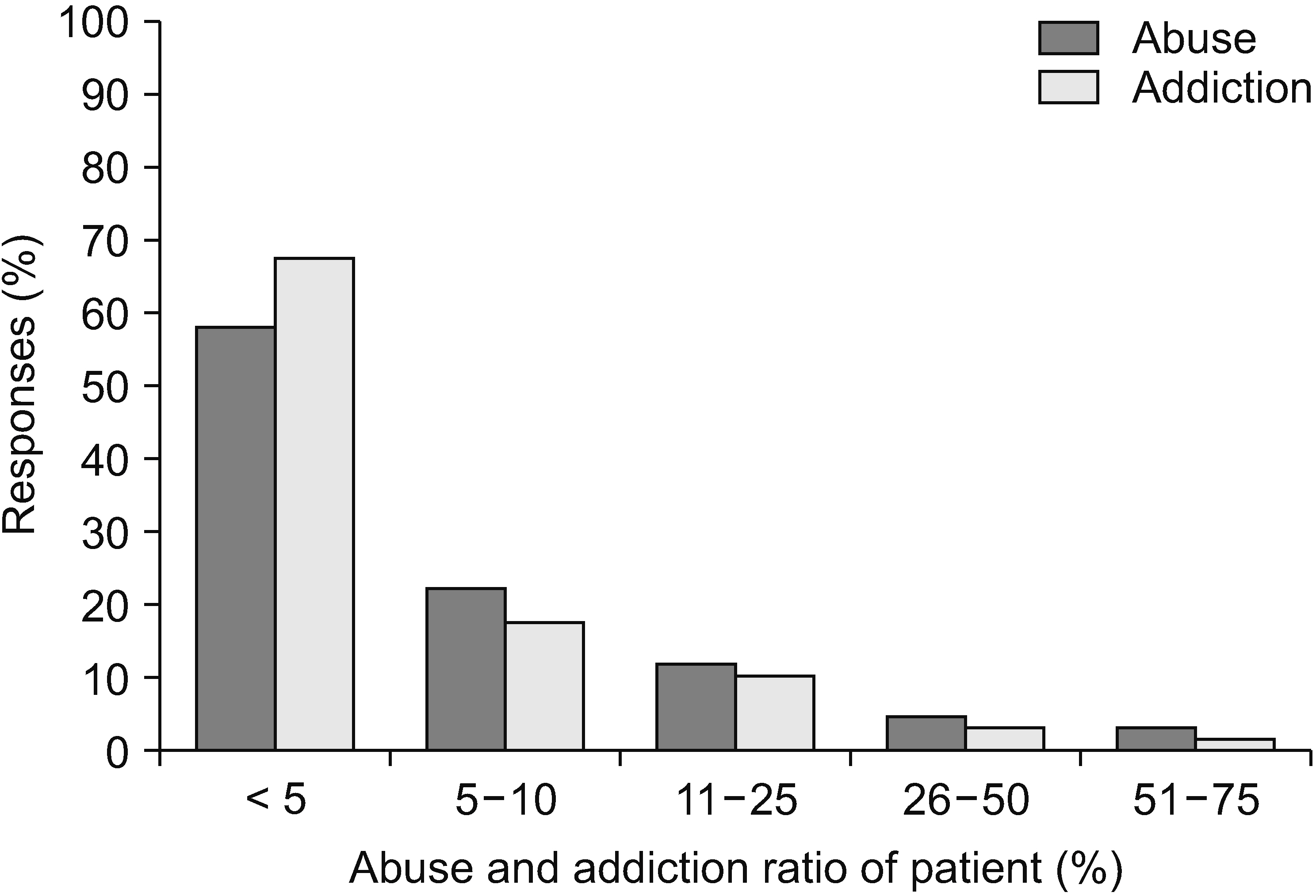
A total of 69 surveys were completed. Most pain physicians started prescribing opioids at a pain score of 7/10 and aimed to reduce pain by 50%. Most physicians (73.1%) actively explained the prescribed medications and possible side effects, and 61.2% of physicians preferred the prescription interval of 4 weeks. Immediate-release opioids were the most popular treatment for breakthrough pain (92.6%). The most common side effect encountered by physicians was constipation (43.3%), followed by nausea/vomiting (34.3%). Of the physicians, 56.5% replied that addiction and misuse prevalences were less than 5%. However, the most concerning side effect was addiction (33.0%).
Conclusions
The survey results showed that the prescribing patterns of pain physicians generally followed Korean guidelines. Physicians were most interested in the safety and effectiveness of opioid prescriptions. They were most concerned about respiratory depression and abuse or addiction. A significant number of physicians agreed that the NHIS regulations needed improvement for patient convenience and safe and effective treatment, though there were pros and cons of the NHIS restrictions on prescription conditions.
Keyword
Figure
Reference
-
1. Nadeau SE. 2015; Opioids for chronic noncancer pain: to prescribe or not to prescribe-what is the question? Neurology. 85:646–51. DOI: 10.1212/WNL.0000000000001766. PMID: 26138946. PMCID: PMC4548284. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84939506338&origin=inward.2. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. 2017; Health utilities in people with chronic pain using a population-level survey and linked health care administrative data. Pain. 158:408–16. DOI: 10.1097/j.pain.0000000000000776. PMID: 27902568. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85015777826&origin=inward.
Article3. Fredheim OM, Kaasa S, Fayers P, Saltnes T, Jordhøy M, Borchgrevink PC. 2008; Chronic non-malignant pain patients report as poor health-related quality of life as palliative cancer patients. Acta Anaesthesiol Scand. 52:143–8. DOI: 10.1111/j.1399-6576.2007.01524.x. PMID: 18005378. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=37549051381&origin=inward.
Article4. Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. American Society of Interventional Pain Physicians. 2009; Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 12:E35–70. DOI: 10.36076/ppj.2009/12/E35. PMID: 19668291.5. Ballantyne JC, LaForge SK. 2007; Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 129:235–55. Erratum in: Pain 2007; 131: 350. DOI: 10.1016/j.pain.2007.07.021. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34548493466&origin=inward.
Article6. Warner EA. 2012; Opioids for the treatment of chronic noncancer pain. Am J Med. 125:1155–61. DOI: 10.1016/j.amjmed.2012.04.032. PMID: 22944349. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84869222793&origin=inward.
Article7. Busse JW, Craigie S, Juurlink DN, Buckley DN, Wang L, Couban RJ, et al. 2017; Guideline for opioid therapy and chronic noncancer pain. CMAJ. 189:E659–66. DOI: 10.1503/cmaj.170363. PMID: 28483845. PMCID: PMC5422149. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85019153936&origin=inward.
Article8. Kim ED, Lee JY, Son JS, Byeon GJ, Yeo JS, Kim DW, et al. 2017; Guidelines for prescribing opioids for chronic non-cancer pain in Korea. Korean J Pain. 30:18–33. DOI: 10.3344/kjp.2017.30.1.18. PMID: 28119768. PMCID: PMC5256264. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85010471669&origin=inward.
Article9. Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, et al. 2007; Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 147:478–91. Erratum in: Ann Intern Med 2008; 148: 247-8. DOI: 10.7326/0003-4819-147-7-200710020-00006. PMID: 17909209. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34848925500&origin=inward.
Article10. Han T. 2001; Opioids in cancer and non-cancer pain management in Korea: the past, present and future. Eur J Pain. 5 Suppl A:73–8. DOI: 10.1053/eujp.2001.0284. PMID: 11798222. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0035696241&origin=inward.
Article11. Cho NR, Chang YJ, Lee D, Kim JR, Ko DS, Choi JJ. 2021; Trends in opioid prescribing practices in South Korea, 2009-2019: are we safe from an opioid epidemic? PLoS One. 16:e0250972. DOI: 10.1371/journal.pone.0250972. PMID: 33979378. PMCID: PMC8115784. PMID: 69d86f514f0541bfa44b009bf800f6cc. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85105620114&origin=inward.
Article12. Kim K, Lee H, Shin JY. 2020; Explosive increase in tramadol use in Korea 2003-2013: analysis of patient trends based on the Korea National Health Insurance Database. J Psychoactive Drugs. 52:153–61. DOI: 10.1080/02791072.2019.1612125. PMID: 31079571. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086052347&origin=inward.
Article13. Gostin LO, Hodge JG Jr, Noe SA. 2017; Reframing the opioid epidemic as a national emergency. JAMA. 318:1539–40. DOI: 10.1001/jama.2017.13358. PMID: 28832871. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85033236376&origin=inward.
Article14. Kahan M, Mailis-Gagnon A, Wilson L, Srivastava A. National Opioid Use Guideline Group. 2011; Canadian guideline for safe and effective use of opioids for chronic noncancer pain: clinical summary for family physicians. Part 1: general population. Can Fam Physician. 57:1257–66. e407–18. PMID: 22084455. PMCID: PMC3215602. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=81855218048&origin=inward.15. Oh TK, Jeon YT, Choi JW. 2019; Trends in chronic opioid use and association with five-year survival in South Korea: a population-based cohort study. Br J Anaesth. 123:655–63. DOI: 10.1016/j.bja.2019.08.012. PMID: 31558315. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85072384311&origin=inward.
Article16. Baik JS. 2017; Guidelines for prescribing opioids for chronic non-cancer pain in Korea: can you overcome "opiophobia"? Korean J Pain. 30:1–2. DOI: 10.3344/kjp.2017.30.1.1. PMID: 28119766. PMCID: PMC5256267. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85010297602&origin=inward.
Article17. Kim MH, Park H, Park EC, Park K. 2011; Attitude and knowledge of physicians about cancer pain management: young doctors of South Korea in their early career. Jpn J Clin Oncol. 41:783–91. DOI: 10.1093/jjco/hyr043. PMID: 21502282. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=79957859396&origin=inward.
Article18. Le Merrer J, Becker JA, Befort K, Kieffer BL. 2009; Reward processing by the opioid system in the brain. Physiol Rev. 89:1379–412. DOI: 10.1152/physrev.00005.2009. PMID: 19789384. PMCID: PMC4482114. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=70349682196&origin=inward.
Article19. O'Brien T, Christrup LL, Drewes AM, Fallon MT, Kress HG, McQuay HJ, et al. 2017; European Pain Federation position paper on appropriate opioid use in chronic pain management. Eur J Pain. 21:3–19. DOI: 10.1002/ejp.970. PMID: 27991730. PMCID: PMC6680203. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85006314811&origin=inward.20. Jani M, Birlie Yimer B, Sheppard T, Lunt M, Dixon WG. 2020; Time trends and prescribing patterns of opioid drugs in UK primary care patients with non-cancer pain: a retrospective cohort study. PLoS Med. 17:e1003270. DOI: 10.1371/journal.pmed.1003270. PMID: 33057368. PMCID: PMC7561110. PMID: 3e1558bf693f404889fcdbe2fa9409b0. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85093490305&origin=inward.
Article21. Barnett ML, Olenski AR, Jena AB. 2017; Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. 376:663–73. DOI: 10.1056/NEJMsa1610524. PMID: 28199807. PMCID: PMC5428548. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85013498947&origin=inward.
Article22. Franklin GM. American Academy of Neurology. 2014; Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology. Neurology. 83:1277–84. DOI: 10.1212/WNL.0000000000000839. PMID: 25267983. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84921766370&origin=inward.
Article23. Dowell D, Haegerich TM, Chou R. 2016; CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep. 65:1–49. Erratum in: MMWR Recomm Rep 2016; 65: 295. DOI: 10.15585/mmwr.rr6501e1. PMID: 26987082. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84978823999&origin=inward.
Article24. Gaskin DJ, Richard P. 2012; The economic costs of pain in the United States. J Pain. 13:715–24. DOI: 10.1016/j.jpain.2012.03.009. PMID: 22607834. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84864445461&origin=inward.
Article25. Castañeda AM, Lee CS, Kim YC, Lee D, Moon JY. 2018; Addressing opioid-related chemical coping in long-term opioid therapy for chronic noncancer pain: a multicenter, observational, cross-sectional study. J Clin Med. 7:354. DOI: 10.3390/jcm7100354. PMID: 30322212. PMCID: PMC6210168. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85085120941&origin=inward.
Article26. Boudreau D, Von Korff M, Rutter CM, Saunders K, Ray GT, Sullivan MD, et al. 2009; Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 18:1166–75. DOI: 10.1002/pds.1833. PMID: 19718704. PMCID: PMC3280087. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=67651094525&origin=inward.
Article27. Petzke F, Bock F, Hüppe M, Nothacker M, Norda H, Radbruch L, et al. 2020; Long-term opioid therapy for chronic noncancer pain: second update of the German guidelines. Pain Rep. 5:e840. DOI: 10.1097/PR9.0000000000000840. PMID: 32904018. PMCID: PMC7447355. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85105915220&origin=inward.
Article28. Chou R, Huffman LH. American Pain Society. American College of Physicians. 2007; Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 147:505–14. Erratum in: Ann Intern Med 2008; 148: 247-8. DOI: 10.7326/0003-4819-147-7-200710020-00008. PMID: 17909211. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34848826292&origin=inward.
Article29. Eisenberg E, McNicol ED, Carr DB. 2005; Efficacy and safety of opioid agonists in the treatment of neuropathic pain of nonmalignant origin: systematic review and meta-analysis of randomized controlled trials. JAMA. 293:3043–52. DOI: 10.1001/jama.293.24.3043. PMID: 15972567. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=20644431597&origin=inward.
Article30. Barbera L, Seow H, Husain A, Howell D, Atzema C, Sutradhar R, et al. 2012; Opioid prescription after pain assessment: a population-based cohort of elderly patients with cancer. J Clin Oncol. 30:1095–9. DOI: 10.1200/JCO.2011.37.3068. PMID: 22370317. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84863951751&origin=inward.
Article31. Beloeil H, Albaladejo P, Sion A, Durand M, Martinez V, Lasocki S, et al. 2019; Multicentre, prospective, double-blind, randomised controlled clinical trial comparing different non-opioid analgesic combinations with morphine for postoperative analgesia: the OCTOPUS study. Br J Anaesth. 122:e98–106. DOI: 10.1016/j.bja.2018.10.058. PMID: 30915987. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85059165166&origin=inward.
Article32. Carville SF, Arendt-Nielsen L, Bliddal H, Blotman F, Branco JC, Buskila D, et al. 2008; EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis. 67:536–41. Erratum in: Ann Rheum Dis 2015; 74: 476. DOI: 10.1136/ard.2007.071522. PMID: 17644548. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=41849093775&origin=inward.
Article33. Lee J, Lim YH, Hong SJ, Jeong JH, Choi HR, Park SK, et al. 2021; Multicenter survey of symptoms, work life, economic status, and quality of life of complex regional pain syndrome patients. Korean J Pain. 34:288–303. DOI: 10.3344/kjp.2021.34.3.288. PMID: 34193635. PMCID: PMC8255153. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85110343207&origin=inward.
Article34. Busse JW, Wang L, Kamaleldin M, Craigie S, Riva JJ, Montoya L, et al. 2018; Opioids for chronic noncancer pain: a systematic review and meta-analysis. JAMA. 320:2448–60. DOI: 10.1001/jama.2018.18472. PMID: 30561481. PMCID: PMC6583638. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85058673821&origin=inward.35. Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Slavin K, Trescot AM, et al. 2017; Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 20(2S):S3–92. DOI: 10.36076/ppj.2017.s92. PMID: 28226332.36. Woo A, Lechner B, Fu T, Wong CS, Chiu N, Lam H, et al. 2015; Cut points for mild, moderate, and severe pain among cancer and non-cancer patients: a literature review. Ann Palliat Med. 4:176–83. DOI: 10.3978/j.issn.2224-5820.2015.09.04. PMID: 26541396. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84987625579&origin=inward.37. Kim J, Shin S, Jeong Y, Kim SY, Lee HJ. 2020; Medicolegal consideration to prevent medical malpractice regarding opioid administration: an analysis of judicial opinion in South Korea. J Pain Res. 13:1525–32. DOI: 10.2147/JPR.S256759. PMID: 32612380. PMCID: PMC7323961. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086874080&origin=inward.38. Kim CL, Hong SJ, Lim YH, Jeong JH, Moon HS, Choi HR, et al. 2020; Patients' perception about opioids and addiction in South Korea. Korean J Pain. 33:234–44. DOI: 10.3344/kjp.2020.33.3.234. PMID: 32606268. PMCID: PMC7336346. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85091747747&origin=inward.
Article39. Hanks GW, Conno F, Cherny N, Hanna M, Kalso E, McQuay HJ, et al. 2001; Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer. 84:587–93. DOI: 10.1054/bjoc.2001.1680. PMID: 11237376. PMCID: PMC2363790. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0037758126&origin=inward.
Article40. Smith HS. 2008; Combination opioid analgesics. Pain Physician. 11:201–14. DOI: 10.36076/ppj.2008/11/201. PMID: 18354712.
Article41. Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. 2009; Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 10:113–30. DOI: 10.1016/j.jpain.2008.10.008. PMID: 19187889. PMCID: PMC4043401. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=58949087497&origin=inward.
Article42. Kalso E, Edwards JE, Moore AR, McQuay HJ. 2004; Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 112:372–80. DOI: 10.1016/j.pain.2004.09.019. PMID: 15561393.
Article43. Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, et al. 2017; Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 20(2S):S93–109. DOI: 10.36076/ppj.2017.s109. PMID: 28226333.44. Salsitz EA. 2016; Chronic pain, chronic opioid addiction: a complex nexus. J Med Toxicol. 12:54–7. DOI: 10.1007/s13181-015-0521-9. PMID: 26602212. PMCID: PMC4781803. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84948132277&origin=inward.
Article45. Soffin EM, Lee BH, Kumar KK, Wu CL. 2019; The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth. 122:e198–208. DOI: 10.1016/j.bja.2018.11.019. PMID: 30915988. PMCID: PMC8176648. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85059153949&origin=inward.
Article46. Webster LR. 2017; Risk factors for opioid-use disorder and overdose. Anesth Analg. 125:1741–8. DOI: 10.1213/ANE.0000000000002496. PMID: 29049118. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85032450877&origin=inward.
Article47. Clark DJ, Schumacher MA. 2017; America's opioid epidemic: supply and demand considerations. Anesth Analg. 125:1667–74. DOI: 10.1213/ANE.0000000000002388. PMID: 29049112. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85032440107&origin=inward.48. Champagne-Langabeer T, Madu R, Giri S, Stotts AL, Langabeer JR. 2021; Opioid prescribing patterns and overdose deaths in Texas. Subst Abus. 42:161–7. DOI: 10.1080/08897077.2019.1675114. PMID: 31644388. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85074584595&origin=inward.
Article49. Guy GP Jr, Zhang K, Bohm MK, Losby J, Lewis B, Young R, et al. 2017; Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 66:697–704. DOI: 10.15585/mmwr.mm6626a4. PMID: 28683056. PMCID: PMC5726238. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85024105633&origin=inward.
Article50. Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, et al. 2015; The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 36:559–74. DOI: 10.1146/annurev-publhealth-031914-122957. PMID: 25581144. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84925260632&origin=inward.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Time on shift in the emergency department and decision to prescribe opioids to patients without chronic opioid use
- Patients’ perception about opioids and addiction in South Korea
- Attitudes toward Social Issues Related to Opioid Use among Palliative Care Physicians
- Cancer Pain Management: Opioids
- Breakthrough pain and rapid-onset opioids in patients with cancer pain: a narrative review