Korean J Transplant.
2022 Sep;36(3):173-179. 10.4285/kjt.22.0018.
First and second kidney transplantations from living donors offer comparable outcomes for patients
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Surgery, Seoul Medical Center, Seoul, Korea
- 3Department of Statistics and Data Center, Samsung Medical Center, Seoul, Korea
- 4Department of Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- KMID: 2533954
- DOI: http://doi.org/10.4285/kjt.22.0018
Abstract
- Background
Increasingly many patients are being relisted for repeat kidney transplantation due to longer survival times after transplantation. This study compared the outcomes of second living donor kidney transplantations (LDKTs) with those of first LDKTs.
Methods
Data were collected retrospectively for 1,429 LDKTs performed from 1995 to 2020 at Samsung Medical Center. The demographics of recipients and donors, immu-nologic factors, and outcomes of second LDKTs were compared to those of first LDKTs.
Results
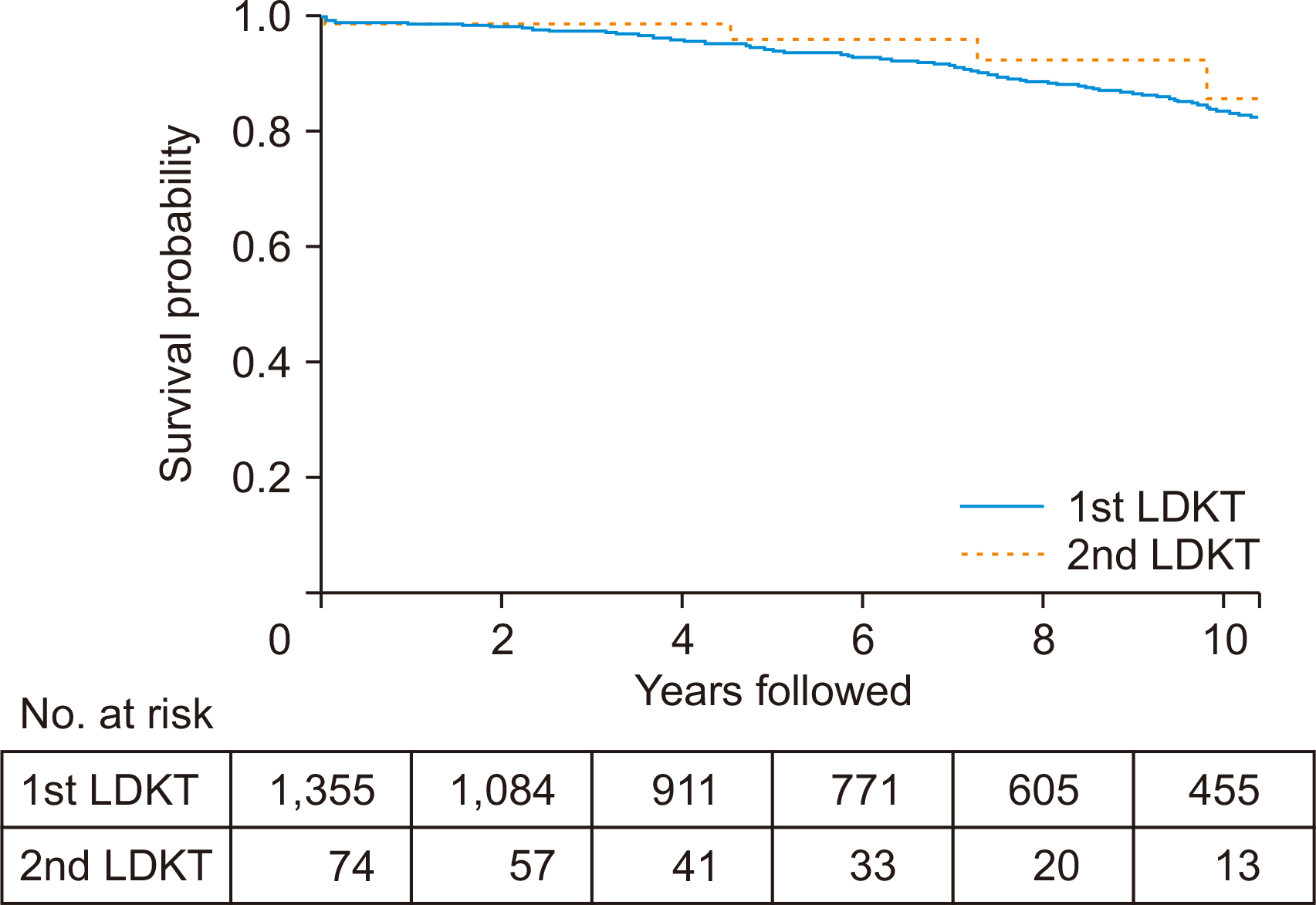
Among 1,429 cases of LDKT, 1,355 were first LDKT cases and 74 were second LDKT cases. Basic demographic data were comparable for the two groups of patients. The 5- and 10-year graft survival rates were 94% and 84% for first LDKTs and 96% and 86% for second LDKTs, respectively, with neither difference statistically significant (P=0.399). The 5- and 10-year patient survival rates were 98% and 94% for the first and 96% and 93% for the second LDKTs, respectively; neither difference was statistically significant (P=0.766). Multivariate analysis confirmed that a history of previous trans-plantation was not a statistically significant risk factor for graft loss (hazard ratio [HR], 0.83; P=0.677) or patient death (HR, 1.68; P=0.396).
Conclusions
These results indicate that repeat kidney transplantation from living donors is a reasonable choice for patients who have experienced graft loss.
Figure
Reference
-
1. Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, et al. 2011; Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 11:2093–109. DOI: 10.1111/j.1600-6143.2011.03686.x. PMID: 21883901.2. Lamb KE, Lodhi S, Meier-Kriesche HU. 2011; Long-term renal allograft survival in the United States: a critical reappraisal. Am J Transplant. 11:450–62. DOI: 10.1111/j.1600-6143.2010.03283.x. PMID: 20973913.3. Poggio ED, Augustine JJ, Arrigain S, Brennan DC, Schold JD. 2021; Long-term kidney transplant graft survival: making progress when most needed. Am J Transplant. 21:2824–32. DOI: 10.1111/ajt.16463. PMID: 33346917.4. Magee JC, Barr ML, Basadonna GP, Johnson MR, Mahadevan S, McBride MA, et al. 2007; Repeat organ transplantation in the United States, 1996-2005. Am J Transplant. 7(5 Pt 2):1424–33. DOI: 10.1111/j.1600-6143.2007.01786.x. PMID: 17428290.5. Fiorentino M, Gallo P, Giliberti M, Colucci V, Schena A, Stallone G, et al. 2020; Management of patients with a failed kidney transplant: what should we do? Clin Kidney J. 14:98–106. DOI: 10.1093/ckj/sfaa094. PMID: 33564409. PMCID: PMC7857798.6. Pour-Reza-Gholi F, Nafar M, Saeedinia A, Farrokhi F, Firouzan A, Simforoosh N, et al. 2005; Kidney retransplantation in comparison with first kidney transplantation. Transplant Proc. 37:2962–4. DOI: 10.1016/j.transproceed.2005.08.034. PMID: 16213274.7. El-Agroudy AE, Wafa EW, Bakr MA, Donia AF, Ismail AM, Shokeir AA, et al. 2004; Living-donor kidney retransplantation: risk factors and outcome. BJU Int. 94:369–73. DOI: 10.1111/j.1464-410X.2004.04934.x. PMID: 15291869.8. Ojo A, Wolfe RA, Agodoa LY, Held PJ, Port FK, Leavey SF, et al. 1998; Prognosis after primary renal transplant failure and the beneficial effects of repeat transplantation: multivariate analyses from the United States Renal Data System. Transplantation. 66:1651–9. DOI: 10.1097/00007890-199812270-00014. PMID: 9884254.9. Rao PS, Schaubel DE, Wei G, Fenton SS. 2006; Evaluating the survival benefit of kidney retransplantation. Transplantation. 82:669–74. DOI: 10.1097/01.tp.0000235434.13327.11. PMID: 16969291.10. Meier-Kriesche HU, Kaplan B. 2002; Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation. 74:1377–81. DOI: 10.1097/00007890-200211270-00005. PMID: 12451234.11. Lefaucheur C, Suberbielle-Boissel C, Hill GS, Nochy D, Andrade J, Antoine C, et al. 2008; Clinical relevance of preformed HLA donor-specific antibodies in kidney transplantation. Am J Transplant. 8:324–31. DOI: 10.1111/j.1600-6143.2007.02072.x. PMID: 18162086.12. Amrouche L, Aubert O, Suberbielle C, Rabant M, Van Huyen JD, Martinez F, et al. 2017; Long-term outcomes of kidney transplantation in patients with high levels of preformed DSA: the Necker high-risk transplant program. Transplantation. 101:2440–8. DOI: 10.1097/TP.0000000000001650. PMID: 28114171.13. Halloran PF. 2004; Immunosuppressive drugs for kidney transplantation. N Engl J Med. 351:2715–29. DOI: 10.1056/NEJMra033540. PMID: 15616206.14. Mourad G, Garrigue V, Squifflet JP, Besse T, Berthoux F, Alamartine E, et al. 2001; Induction versus noninduction in renal transplant recipients with tacrolimus-based immunosuppression. Transplantation. 72:1050–5. DOI: 10.1097/00007890-200109270-00012. PMID: 11579299.15. Brennan DC, Daller JA, Lake KD, Cibrik D. Del Castillo D; Thymoglobulin Induction Study Group. 2006; Rabbit antithymocyte globulin versus basiliximab in renal transplantation. N Engl J Med. 355:1967–77. DOI: 10.1056/NEJMoa060068. PMID: 17093248.16. Schold J, Poggio E, Goldfarb D, Kayler L, Flechner S. 2015; Clinical outcomes associated with induction regimens among retransplant kidney recipients in the United States. Transplantation. 99:1165–71. DOI: 10.1097/TP.0000000000000507. PMID: 25606788.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcomes of Spousal Donor Kidney Transplantation: Single Center Experience
- Hand-assisted Laparoscopic Donor Surgery for Living Donor Pancreas and Kidney Transplantation: A Single Center Experience
- Psychosocial Pre-Transplant Assessment of Living Kidney Donors
- Solid Organ Transplantation in Korea: 1997
- Exchange-donor Program in Renal Transplantation: A single center experience