J Rheum Dis.
2022 Oct;29(4):215-222. 10.4078/jrd.22.0005.
Implications of Persistent Pain in Patients With Rheumatoid Arthritis Despite Remission Status: Data From the KOBIO Registry
- Affiliations
-
- 1Department of Rheumatology, Ajou University School of Medicine, Suwon, Korea
- 2Divison of Rheumatology, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- KMID: 2533622
- DOI: http://doi.org/10.4078/jrd.22.0005
Abstract
Objective
This study aimed to assess the prevalence of pain in patients with RA in clinical remission and analyze the demographic and clinical characteristics of those who experienced persistent pain despite remission status.
Methods
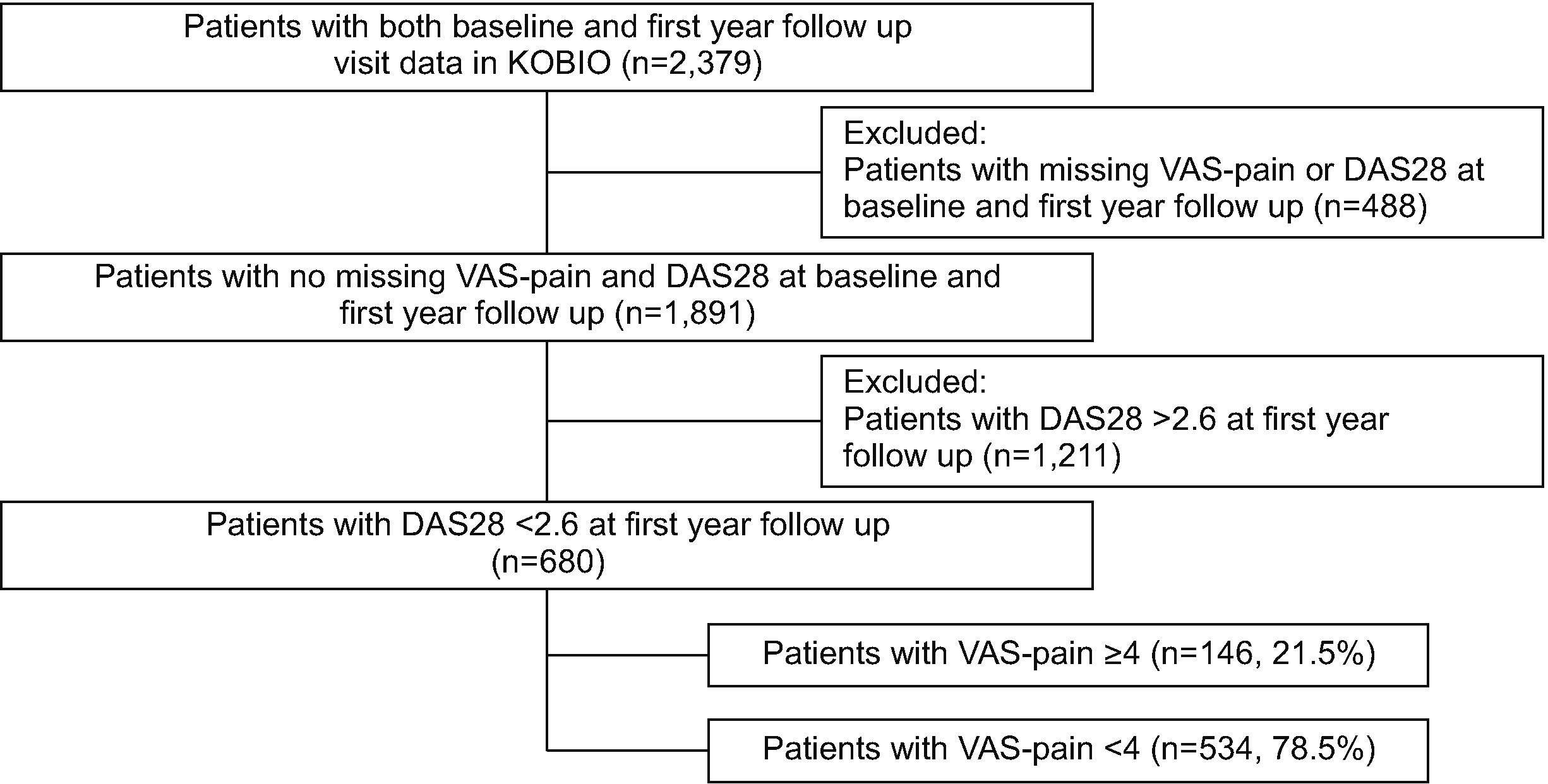
Data from 1,891 patients with RA registered on the Korean College of Rheumatology Biologics and Targeted Therapy registry were obtained. Remission was defined as a Disease Activity Score of 28 joints-erythrocyte sedimentation rate (ESR) <2.6. Pain intensity was classified as severe (pain visual analog scale [VAS] ≥7), moderate (4≤VAS<7), or mild (VAS <4).
Results
Our analysis showed that 52.6% of patients complained of severe pain at the start of or during switching biological disease-modifying anti-rheumatic drugs (bDMARDs) or targeted synthetic DMARDs (tsDMARDs). Despite having a 36.0% (n=680) remission rate after the use of bDMARDs or tsDMARDs at their 1-year follow-up, 21.5% (n=146) of these patients had moderateto-severe pain, higher frequency of foot erosions, and comorbidities, such as mental illness, endocrine, renal, and neurological disorders, than patients with a milder degree of pain. The multivariable regression analysis showed that presence of foot erosions, neurological disorders, and use of corticosteroids were independently associated with moderate-to-severe pain in patients with RA despite being in remission. The level of ESR and use of Janus kinase inhibitors were inversely associated with moderate-to-severe pain.
Conclusion
Persistent pain and discomfort continue to be a problem for patients with RA in clinical remission. Continued research on insistent pain in patients with RA is warranted to better alleviate distress and improve the quality of life in patients.
Keyword
Figure
Cited by 1 articles
-
Preoperative patient’s expectations and clinical outcomes after rheumatoid forefoot deformity reconstruction by joint sacrificing surgery
Sung-Jae Kim, Young-Woon Gil, Il-Hoon Sung
J Rheum Dis. 2024;31(1):33-40. doi: 10.4078/jrd.2023.0044.
Reference
-
1. Uhlig T, Moe RH, Kvien TK. 2014; The burden of disease in rheumatoid arthritis. Pharmacoeconomics. 32:841–51. DOI: 10.1007/s40273-014-0174-6. PMID: 24859304.
Article2. Kim J, Koh JH, Choi SJ, Jeon CH, Kwok SK, Kim SK, et al. 2021; KOBIO, the first web-based Korean biologics registry operated with a unified platform among distinct disease entities. J Rheum Dis. 28:176–82. DOI: 10.4078/jrd.2021.28.4.176.
Article3. Sugihara T, Ishizaki T, Onoguchi W, Baba H, Matsumoto T, Iga S, et al. 2021; Effectiveness and safety of treat-to-target strategy in elderly-onset rheumatoid arthritis: a 3-year prospective observational study. Rheumatology (Oxford). 60:4252–61. DOI: 10.1093/rheumatology/keaa922. PMID: 33410490.
Article4. Gossec L, Dougados M, Rincheval N, Balanescu A, Boumpas DT, Canadelo S, et al. 2009; Elaboration of the preliminary Rheumatoid Arthritis Impact of Disease (RAID) score: a EULAR initiative. Ann Rheum Dis. 68:1680–5. DOI: 10.1136/ard.2008.100271. PMID: 19054825.
Article5. Vergne-Salle P, Pouplin S, Trouvin AP, Bera-Louville A, Soubrier M, Richez C, et al. 2020; The burden of pain in rheumatoid arthritis: impact of disease activity and psychological factors. Eur J Pain. 24:1979–89. DOI: 10.1002/ejp.1651. PMID: 32841455. PMCID: PMC7692940.
Article6. Ten Klooster PM, Vonkeman HE, Oude Voshaar MA, Siemons L, van Riel PL, van de Laar MA. 2015; Predictors of satisfactory improvements in pain for patients with early rheumatoid arthritis in a treat-to-target study. Rheumatology (Oxford). 54:1080–6. DOI: 10.1093/rheumatology/keu449. PMID: 25433041.
Article7. Choi IA. 2017; Comparison of the disease activity score-28 based on the erythrocyte sedimentation rate and C-reactive protein in rheumatoid arthritis. J Rheum Dis. 24:287–92. DOI: 10.4078/jrd.2017.24.5.287.
Article8. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. 2010; 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 62:2569–81. DOI: 10.1002/art.27584. PMID: 20872595.
Article9. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. 1988; The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 31:315–24. DOI: 10.1002/art.1780310302. PMID: 3358796.
Article10. Lee YC, Bingham CO 3rd, Edwards RR, Marder W, Phillips K, Bolster MB, et al. 2018; Association between pain sensitization and disease activity in patients with rheumatoid arthritis: a cross-sectional study. Arthritis Care Res (Hoboken). 70:197–204. Erratum. DOI: 10.1002/acr.23266. PMID: 28437846. PMCID: PMC5654691.
Article11. Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, et al. 2011; American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 63:573–86. DOI: 10.1002/art.30129. PMID: 21294106. PMCID: PMC3115717.12. Studenic P, Radner H, Smolen JS, Aletaha D. 2012; Discrepancies between patients and physicians in their perceptions of rheumatoid arthritis disease activity. Arthritis Rheum. 64:2814–23. DOI: 10.1002/art.34543. PMID: 22810704.
Article13. Vladimirova N, Jespersen A, Bartels EM, Christensen AW, Bliddal H, Danneskiold-Samsøe B. 2015; Pain sensitisation in women with active rheumatoid arthritis: a comparative cross-sectional study. Arthritis. 2015:434109. DOI: 10.1155/2015/434109. PMID: 26266046. PMCID: PMC4523644.14. Lee YC, Frits ML, Iannaccone CK, Weinblatt ME, Shadick NA, Williams DA, et al. 2014; Subgrouping of patients with rheumatoid arthritis based on pain, fatigue, inflammation, and psychosocial factors. Arthritis Rheumatol. 66:2006–14. DOI: 10.1002/art.38682. PMID: 24782222. PMCID: PMC4188637.
Article15. Zhao SS, Duffield SJ, Goodson NJ. 2019; The prevalence and impact of comorbid fibromyalgia in inflammatory arthritis. Best Pract Res Clin Rheumatol. 33:101423. DOI: 10.1016/j.berh.2019.06.005. PMID: 31703796.
Article16. Lee YC. 2013; Effect and treatment of chronic pain in inflammatory arthritis. Curr Rheumatol Rep. 15:300. DOI: 10.1007/s11926-012-0300-4. PMID: 23292816. PMCID: PMC3552517.17. Foley HE, Knight JC, Ploughman M, Asghari S, Audas R. 2021; Association of chronic pain with comorbidities and health care utilization: a retrospective cohort study using health administrative data. Pain. 162:2737–49. DOI: 10.1097/j.pain.0000000000002264. PMID: 33902092.
Article18. Roodenrijs NMT, van der Goes MC, Welsing PMJ, Tekstra J, Lafeber FPJG, Jacobs JWG, et al. 2021; Difficult-to-treat rheumatoid arthritis: contributing factors and burden of disease. Rheumatology (Oxford). 60:3778–88. DOI: 10.1093/rheumatology/keaa860. PMID: 33331946.
Article19. Raoof R, Willemen HLDM, Eijkelkamp N. 2018; Divergent roles of immune cells and their mediators in pain. Rheumatology (Oxford). 57:429–40. DOI: 10.1093/rheumatology/kex308. PMID: 28968842. PMCID: PMC5850827.
Article20. Hess A, Axmann R, Rech J, Finzel S, Heindl C, Kreitz S, et al. 2011; Blockade of TNF-α rapidly inhibits pain responses in the central nervous system. Proc Natl Acad Sci U S A. 108:3731–6. DOI: 10.1073/pnas.1011774108. PMID: 21245297. PMCID: PMC3048151.
Article21. Simon LS, Taylor PC, Choy EH, Sebba A, Quebe A, Knopp KL, et al. 2021; The Jak/STAT pathway: a focus on pain in rheumatoid arthritis. Semin Arthritis Rheum. 51:278–84. DOI: 10.1016/j.semarthrit.2020.10.008. PMID: 33412435.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonographic Findings in Rheumatoid Arthritis
- Toward the cure of rheumatoid arthritis
- Defining Remission of Korean Patients with Rheumatoid Arthritis
- A Study on the Pain, Fatigue Perceived by Rheumatoid Arthritis Patients
- KOBIO, the First Web-based Korean Biologics Registry Operated With a Unified Platform Among Distinct Disease Entities