J Korean Med Sci.
2022 Sep;37(37):e279. 10.3346/jkms.2022.37.e279.
Epidemiological Trends of Pediatric Inflammatory Bowel Disease in Korea: A Multicenter Study of the Last 3 Years Including the COVID-19 Era
- Affiliations
-
- 1Department of Pediatrics, Kosin University College of Medicine, Kosin University Gospel Hospital, Busan, Korea
- 2Department of Pediatrics, School of Medicine, Kyungpook National University, Kyungpook National University Children’s Hospital, Daegu, Korea
- 3Department of Pediatrics, Pusan National University Children’s Hospital, Yangsan, Korea
- 4Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea
- 5Department of Pediatrics, Gyeongsang National University Changwon Hospital, Changwon, Korea
- 6Department of Pediatrics, Dankook University Hospital, Cheonan, Korea
- 7Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Korea
- 8Department of Pediatrics, Jeju National University Hospital, Jeju, Korea
- 9Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 10Department of Pediatrics, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- 11Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 12Department of Pediatrics, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 13Department of Pediatrics, Chung-Ang University Hospital, College of Medicine, Chung-Ang University, Seoul, Korea
- 14Department of Pediatrics, Daegu Catholic University School of Medicine, Daegu, Korea
- 15Department of Pediatrics, Inje University College of Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea
- 16Department of Pediatrics, Kangwon National University School of Medicine, Chuncheon, Korea
- 17Department of Pediatrics, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- 18Research Institute of Clinical Medicine of Jeonbuk National University - Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2533557
- DOI: http://doi.org/10.3346/jkms.2022.37.e279
Abstract
- Background
Studies on how the coronavirus pandemic has affected pediatric inflammatory bowel disease (PIBD) are lacking. We aimed to investigate the trends in epidemiology, characteristics, initial management, and short-term outcomes of PIBD in South Korea over the recent three years including the era of coronavirus disease 2019 (COVID-19).
Methods
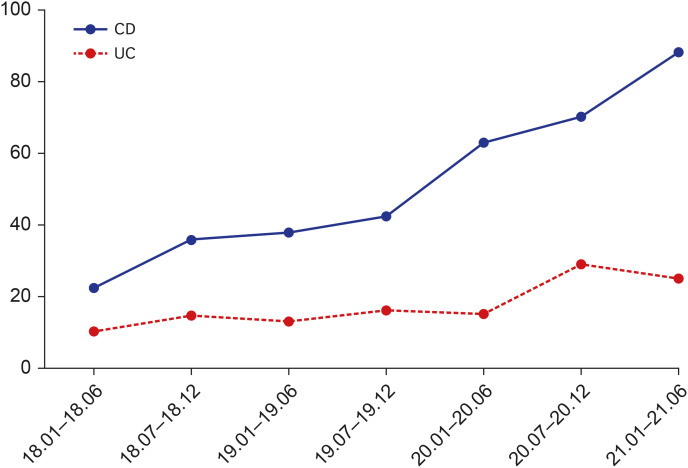
This multicenter study retrospectively investigated temporal trends in the epidemiology of PIBD in Korea. Annual occurrences, disease phenotypes, and initial management at diagnosis were analyzed from January 2018 to June 2021.
Results
A total of 486 patients from 17 institutions were included in this epidemiological evaluation. Analysis of the occurrence trend confirmed a significant increase in PIBD, regardless of the COVID-19 pandemic. In Crohn’s disease, patients with post-coronavirus outbreaks had significantly higher fecal calprotectin levels than those with previous onset 1,339.4 ± 717.04 vs. 1,595.5 ± 703.94, P = 0.001). Patients with post-coronavirus-onset ulcerative colitis had significantly higher Pediatric Ulcerative Colitis Activity Index scores than those with previous outbreaks (48 ± 17 vs. 36 ± 15, P = 0.004). In the initial treatment of Crohn’s disease, the use of 5-aminosalicylic acid (5-ASA) and steroids significantly decreased (P = 0.006 and 0.001, respectively), and enteral nutrition and the use of infliximab increased significantly (P = 0.045 and 0.009, respectively). There was a significant increase in azathioprine use during the initial treatment of ulcerative colitis (P = 0.020).
Conclusion
Regardless of the COVID-19 pandemic, the number of patients with PIBD is increasing significantly annually in Korea. The initial management trends for PIBD have also changed. More research is needed to establish appropriate treatment guidelines considering the epidemiological and clinical characteristics of Korean PIBD.
Keyword
Figure
Reference
-
1. Perlman S. Another decade, another coronavirus. N Engl J Med. 2020; 382(8):760–762. PMID: 31978944.
Article2. Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020; 76:71–76. PMID: 32112977.
Article3. Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020; 35(5):e61. PMID: 32030925.
Article4. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223):507–513. PMID: 32007143.
Article5. Bezzio C, Saibeni S, Variola A, Allocca M, Massari A, Gerardi V, et al. Outcomes of COVID-19 in 79 patients with IBD in Italy: an IG-IBD study. Gut. 2020; 69(7):1213–1217. PMID: 32354990.
Article6. Dulai PS, Thompson KD, Blunt HB, Dubinsky MC, Siegel CA. Risks of serious infection or lymphoma with anti-tumor necrosis factor therapy for pediatric inflammatory bowel disease: a systematic review. Clin Gastroenterol Hepatol. 2014; 12(9):1443–1451. PMID: 24462626.
Article7. Neurath MF. COVID-19 and immunomodulation in IBD. Gut. 2020; 69(7):1335–1342. PMID: 32303609.
Article8. Monteleone G, Ardizzone S. Are patients with inflammatory bowel disease at increased risk for Covid-19 infection? J Crohn’s Colitis. 2020; 14(9):1334–1336. PMID: 32215548.
Article9. Manivannan M, Jogalekar MP, Kavitha MS, Maran BA, Gangadaran P. A mini-review on the effects of COVID-19 on younger individuals. Exp Biol Med (Maywood). 2021; 246(3):293–297. PMID: 33210552.
Article10. Hyams JS, Ferry GD, Mandel FS, Gryboski JD, Kibort PM, Kirschner BS, et al. Development and validation of a pediatric Crohn’s disease activity index. J Pediatr Gastroenterol Nutr. 1991; 12(4):439–447. PMID: 1678008.
Article11. Turner D, Otley AR, Mack D, Hyams J, de Bruijne J, Uusoue K, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology. 2007; 133(2):423–432. PMID: 17681163.
Article12. Daperno M, D’Haens G, Van Assche G, Baert F, Bulois P, Maunoury V, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc. 2004; 60(4):505–512. PMID: 15472670.
Article13. Lobatón T, Bessissow T, De Hertogh G, Lemmens B, Maedler C, Van Assche G, et al. The Modified Mayo Endoscopic Score (MMES): a new index for the assessment of extension and severity of endoscopic activity in ulcerative colitis patients. J Crohn’s Colitis. 2015; 9(10):846–852. PMID: 26116558.
Article14. Huang JG, Aw MM. Pediatric inflammatory bowel disease in Asia: epidemiology and natural history. Pediatr Neonatol. 2020; 61(3):263–271. PMID: 32005607.
Article15. Sýkora J, Pomahačová R, Kreslová M, Cvalínová D, Štych P, Schwarz J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J Gastroenterol. 2018; 24(25):2741–2763. PMID: 29991879.
Article16. Choe JY, Choi S, Song KH, Jang HJ, Choi KH, Yi DY, et al. Incidence and prevalence trends of pediatric inflammatory bowel disease in the Daegu-Kyungpook province from 2017 to 2020. Front Pediatr. 2022; 9:810173. PMID: 35059365.
Article17. Nogueira-de-Almeida CA, Del Ciampo LA, Ferraz IS, Del Ciampo IR, Contini AA, Ued FD. COVID-19 and obesity in childhood and adolescence: a clinical review. J Pediatr (Rio J). 2020; 96(5):546–558. PMID: 32768388.
Article18. Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. 2021; 36(24):e180. PMID: 34155841.
Article19. Park S, Kang Y, Koh H, Kim S. Increasing incidence of inflammatory bowel disease in children and adolescents: significance of environmental factors. Clin Exp Pediatr. 2020; 63(9):337–344. PMID: 32024322.
Article20. Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, et al. ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014; 58(6):795–806. PMID: 24231644.
Article21. Wong K, Isaac DM, Wine E. Growth delay in inflammatory bowel diseases: significance, causes, and management. Dig Dis Sci. 2021; 66(4):954–964. PMID: 33433805.
Article22. Ishige T. Growth failure in pediatric onset inflammatory bowel disease: mechanisms, epidemiology, and management. Transl Pediatr. 2019; 8(1):16–22. PMID: 30881894.
Article23. Ruemmele FM, Veres G, Kolho KL, Griffiths A, Levine A, Escher JC, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohn’s Colitis. 2014; 8(10):1179–1207. PMID: 24909831.
Article24. van Rheenen PF, Aloi M, Assa A, Bronsky J, Escher JC, Fagerberg UL, et al. The medical management of paediatric Crohn’s disease: an ECCO-ESPGHAN guideline update. J Crohn’s Colitis. 2020.
Article25. Yu Y, Chen KC, Chen J. Exclusive enteral nutrition versus corticosteroids for treatment of pediatric Crohn’s disease: a meta-analysis. World J Pediatr. 2019; 15(1):26–36. PMID: 30666565.
Article26. Gong D, Yu X, Wang L, Kong L, Gong X, Dong Q. Exclusive enteral nutrition induces remission in pediatric crohn’s disease via modulation of the gut microbiota. BioMed Res Int. 2017; 2017:8102589. PMID: 29124070.
Article27. Grover Z, Burgess C, Muir R, Reilly C, Lewindon PJ. Early mucosal healing with exclusive enteral nutrition is associated with improved outcomes in newly diagnosed children with luminal Crohn’s disease. J Crohn’s Colitis. 2016; 10(10):1159–1164. PMID: 26980840.
Article28. Allocca M, Fiorino G, Zallot C, Furfaro F, Gilardi D, Radice S, et al. Incidence and patterns of COVID-19 among inflammatory bowel disease patients from the Nancy and Milan cohorts. Clin Gastroenterol Hepatol. 2020; 18(9):2134–2135. PMID: 32360811.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to Cope with COVID-19 in Patients with Inflammatory Bowel Disease
- Food service industry in the era of COVID-19: trends and research implications
- Management of inflammatory bowel disease in the COVID-19 era
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era
- Epidemiological and clinical characteristics of 5,628 patients with coronavirus disease 2019 in South Korea: A nationwide multicenter study