Ann Pediatr Endocrinol Metab.
2022 Sep;27(3):207-213. 10.6065/apem.2142186.093.
The association between idiopathic scoliosis and growth hormone treatment in short children
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- KMID: 2533340
- DOI: http://doi.org/10.6065/apem.2142186.093
Abstract
- Purpose
Idiopathic scoliosis is the most common form of scoliosis, and the risk of onset and progression has been found to correlate with growth spurts. Therefore, treatment with recombinant human growth hormone (GH) treatment in short children may initiate and/or aggravate scoliosis. The aim of this study was to investigate the relationship between idiopathic scoliosis and GH treatment in short children.
Methods
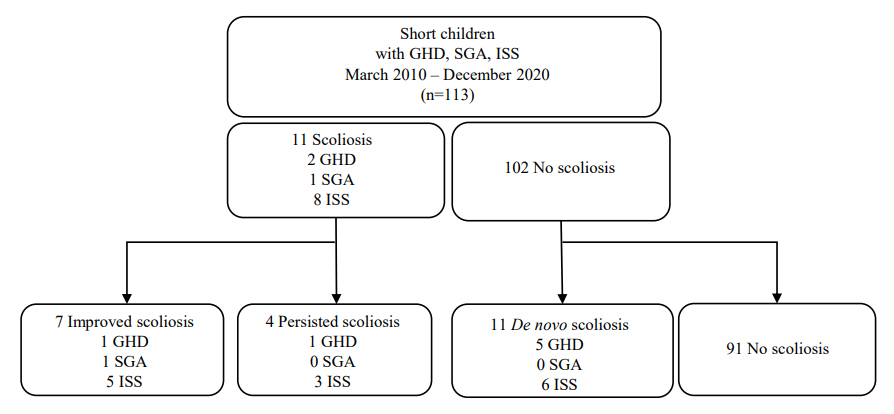
The medical records of 113 subjects seen at the participating institution between January 2010 and December 2020 and who were diagnosed with GH deficiency and small for gestational age, had idiopathic short stature, and were treated with GH for at least one year were reviewed. Scoliosis was defined as a Cobb angle greater than 10 degrees as assessed using a spine x-ray. Clinical data and laboratory findings before and 12 months after GH treatment were compared.
Results
There was significant increase in height, height-standard deviation score, insulin-like growth factor 1, and insulin-like growth factor binding protein 3 (p<0.001) with GH treatment. However, there were no significant differences in the average Cobb angle (6.2°±3.3° vs. 6.1°±3.5°, p=0.842) and the prevalence of scoliosis (9.7% vs. 13.3%, p=0.481) before and after one year of GH treatment. A comparative analysis of both initial Cobb angle and change in Cobb angle during GH treatment showed no relationship with other factors.
Conclusion
Although GH treatment in short children increased height and growth velocity, it was not associated with development or aggravation of idiopathic scoliosis.
Keyword
Figure
Reference
-
References
1. Chung LY, Nam HK, Rhie YJ, Huh R, Lee KH. Prevalence of idiopathic scoliosis in girls with central precocious puberty: effect of a gonadotropin-releasing hormone agonist. Ann Pediatr Endocrinol Metab. 2020; 25:92–6.2. Latalski M, Danielewicz-Bromberek A, Fatyga M, Latalska M, Krober M, Zwolak P. Current insights into the aetiology of adolescent idiopathic scoliosis. Arch Orthop Trauma Surg. 2017; 137:1327–33.3. Willner S, Uden A. A prospective prevalence study of scoliosis in Southern Sweden. Acta Orthop Scand. 1982; 53:233–7.4. Yilmaz H, Zateri C, Kusvuran Ozkan A, Kayalar G, Berk H. Prevalence of adolescent idiopathic scoliosis in Turkey: an epidemiological study. Spine J. 2020; 20:947–55.5. Shi B, Mao S, Liu Z, Sun X, Zhu Z, Zhu F, et al. Spinal growth velocity versus height velocity in predicting curve progression in peri-pubertal girls with idiopathic scoliosis. BMC Musculoskelet Disord. 2016; 17:368.6. Cheung JPY, Cheung PWH, Samartzis D, Luk KD. Curve progression in adolescent idiopathic scoliosis does not match skeletal growth. Clin Orthop Relat Res. 2018; 476:429–36.7. Perez-Machado G, Berenguer-Pascual E, Bovea-Marco M, Rubio-Belmar PA, Garcia-Lopez E, Garzon MJ, et al. From genetics to epigenetics to unravel the etiology of adolescent idiopathic scoliosis. Bone. 2020; 140:115563.8. Richmond E, Rogol AD. Treatment of growth hormone deficiency in children, adolescents and at the transitional age. Best Pract Res Clin Endocrinol Metab. 2016; 30:749–55.9. Devesa J, Almenglo C, Devesa P. Multiple effects of growth hormone in the body: is it really the hormone for growth? Clin Med Insights Endocrinol Diabetes. 2016; 9:47–71.10. Hintz RL, Attie KM, Baptista J, Roche A. Effect of growth hormone treatment on adult height of children with idiopathic short stature. Genentech Collaborative Group. N Engl J Med. 1999; 340:502–7.11. Vance ML, Mauras N. Growth hormone therapy in adults and children. N Engl J Med. 1999; 341:1206–16.12. de Zegher F, Ong KK, Ibanez L, Dunger DB. Growth hormone therapy in short children born small for gestational age. Horm Res. 2006; 65 Suppl 3:145–52.13. Yun YH, Kwon SS, Koh Y, Kim DJ, Ahn J, Lee SY. Influence of growth hormone treatment on radiographic indices of the spine: propensity-matched analysis. J Orthop Surg Res. 2017; 12:130.14. Wang ED, Drummond DS, Dormans JP, Moshang T, Davidson RS, Gruccio D. Scoliosis in patients treated with growth hormone. J Pediatr Orthop. 1997; 17:708–11.15. Park SJ, Lee KH, Lee CS, Kim KT, Jang JH, Shin DH, et al. Impact of growth hormone treatment on scoliosis development and progression: analysis of 1128 patients with idiopathic short stature. J Pediatr Endocrinol Metab. 2020; 34:243–50.16. Rhee N, Oh KY, Yang EM, Kim CJ. Growth hormone responses to provocative tests in children with short stature. Chonnam Med J. 2015; 51:33–8.17. Stanley T. Diagnosis of growth hormone deficiency in childhood. Curr Opin Endocrinol Diabetes Obes. 2012; 19:47–52.18. Pedicelli S, Peschiaroli E, Violi E, Cianfarani S. Controversies in the definition and treatment of idiopathic short stature (ISS). J Clin Res Pediatr Endocrinol. 2009; 1:105–15.19. Gilbert SR, Savage AJ, Whitesell R, Conklin MJ, Fineberg NS. BMI and magnitude of scoliosis at presentation to a specialty clinic. Pediatrics. 2015; 135:e1417–24.20. Hyun SE, Lee BC, Suh BK, Chung SC, Ko CW, Kim HS, et al. Reference values for serum levels of insulin-like growth factor-I and insulin-like growth factor binding protein-3 in Korean children and adolescents. Clin Biochem. 2012; 45:16–21.21. Kaufman FR, Sy JP. Regular monitoring of bone age is useful in children treated with growth hormone. Pediatrics. 1999; 104:1039–42.22. Horng MH, Kuok CP, Fu MJ, Lin CJ, Sun YN. Cobb angle measurement of spine from x-ray images using convolutional neural network. Comput Math Methods Med. 2019; 2019:6357171.23. Wang J, Zhang J, Xu R, Chen TG, Zhou KS, Zhang HH. Measurement of scoliosis Cobb angle by end vertebra tilt angle method. J Orthop Surg Res. 2018; 13:223.24. Backeljauw P, Cappa M, Kiess W, Law L, Cookson C, Sert C, et al. Impact of short stature on quality of life: a systematic literature review. Growth Horm IGF Res. 2021; 57-58:101392.25. Darendeliler F, Karagiannis G, Wilton P. Headache, idiopathic intracranial hypertension and slipped capital femoral epiphysis during growth hormone treatment: a safety update from the KIGS database. Horm Res. 2007; 68 Suppl 5:41–7.26. Coutant R, Bosch Munoz J, Dumitrescu CP, Schnabel D, Sert C, Perrot V, et al. Effectiveness and overall safety of NutropinAq((R)) for growth hormone deficiency and other paediatric growth hormone disorders: completion of the international cooperative growth study, NutropinAq((R)) European Registry (iNCGS). Front Endocrinol (Lausanne). 2021; 12:676083.27. Grimberg A, DiVall SA, Polychronakos C, Allen DB, Cohen LE, Quintos JB, et al. Guidelines for growth hormone and insulin-like growth factor-I treatment in children and adolescents: growth hormone deficiency, idiopathic short stature, and primary insulin-like growth factor-I deficiency. Horm Res Paediatr. 2016; 86:361–97.28. Kemp SF, Kuntze J, Attie KM, Maneatis T, Butler S, Frane J, et al. Efficacy and safety results of long-term growth hormone treatment of idiopathic short stature. J Clin Endocrinol Metab. 2005; 90:5247–53.29. Morais T, Bernier M, Turcotte F. Age- and sex-specific prevalence of scoliosis and the value of school screening programs. Am J Public Health. 1985; 75:1377–80.30. Kim JY, Rosenfeld SR, Keyak JH. Increased prevalence of scoliosis in Turner syndrome. J Pediatr Orthop. 2001; 21:765–6.31. Craig ME, Cowell CT, Larsson P, Zipf WB, Reiter EO, Albertsson Wikland K, et al. Growth hormone treatment and adverse events in Prader-Willi syndrome: data from KIGS (the Pfizer International Growth Database). Clin Endocrinol (Oxf). 2006; 65:178–85.32. Modi HN, Suh SW, Yang JH, Hong JY, Venkatesh K, Muzaffar N. Spontaneous regression of curve in immature idiopathic scoliosis - does spinal column play a role to balance? An observation with literature review. J Orthop Surg Res. 2010; 5:80.33. Soucacos PN, Zacharis K, Gelalis J, Soultanis K, Kalos N, Beris A, et al. Assessment of curve progression in idiopathic scoliosis. Eur Spine J. 1998; 7:270–7.34. Trobisch P, Suess O, Schwab F. Idiopathic scoliosis. Dtsch Arztebl Int. 2010; 107:875–83. quiz 84.35. Nakamura Y, Murakami N, Iida T, Asano S, Ozeki S, Nagai T. Growth hormone treatment for osteoporosis in patients with scoliosis of Prader-Willi syndrome. J Orthop Sci. 2014; 19:877–82.36. Grootjen LN, Rutges J, Damen L, Donze SH, Juriaans AF, Kerkhof GF, et al. Effects of 8 years of growth hormone treatment on scoliosis in children with Prader-Willi syndrome. Eur J Endocrinol. 2021; 185:47–55.37. Addai D, Zarkos J, Bowey AJ. Current concepts in the diagnosis and management of adolescent idiopathic scoliosis. Childs Nerv Syst. 2020; 36:1111–9.38. Cheng JC, Castelein RM, Chu WC, Danielsson AJ, Dobbs MB, Grivas TB, et al. Adolescent idiopathic scoliosis. Nat Rev Dis Primers. 2015; 1:15030.39. Ahl T, Albertsson-Wikland K, Kalen R. Twenty-four-hour growth hormone profiles in pubertal girls with idiopathic scoliosis. Spine (Phila Pa 1976). 1988; 13:139–42.40. Blum WF, Alherbish A, Alsagheir A, El Awwa A, Kaplan W, Koledova E, et al. The growth hormone-insulin-like growth factor-I axis in the diagnosis and treatment of growth disorders. Endocr Connect. 2018; 7:R212–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Growth Hormone Therapy in Short Stature Children
- Commentary on "The association between idiopathic scoliosis and growth hormone treatment in short children"
- Short Stature and Growth Hormone Therapy
- Comparison of Growth Hormone Treatment in Patients with Idiopathic Short Stature and Idiopathic Growth Hormone Deficiency
- The Effects of Growth Hormone on Carbohydrate and Lipid Metabolism