J Korean Med Sci.
2022 Sep;37(36):e270. 10.3346/jkms.2022.37.e270.
Annual Case Volume and One-Year Mortality for Endovascular Treatment in Acute Ischemic Stroke
- Affiliations
-
- 1Department of Neurology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Neurology, Korea University Guro Hospital, Seoul, Korea
- 3Department of Neurology, Inje University Ilsan Paik Hospital, Goyang, Korea
- 4Department of Neurology, Uijeongbu Eulji Medical Center, Eulji University, Uijeongbu, Korea
- 5Department of Neurology, Soonchunhyang University Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 6Department of Neurology, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea
- 7Clinical Research Center, Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea
- 8Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- 9Health Insurance Review and Assessment Service, Wonju, Korea
- 10Department of Neurology, Gyeonggi Provincial Medical Center Icheon Hospital, Icheon, Korea
- 11Davee Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, Illinois.
- KMID: 2533225
- DOI: http://doi.org/10.3346/jkms.2022.37.e270
Abstract
- Background
The association between endovascular treatment (EVT) case volume per hospital and clinical outcomes has been reported, but the exact volume threshold has not been determined. This study aimed to examine the case volume threshold in this context.
Methods
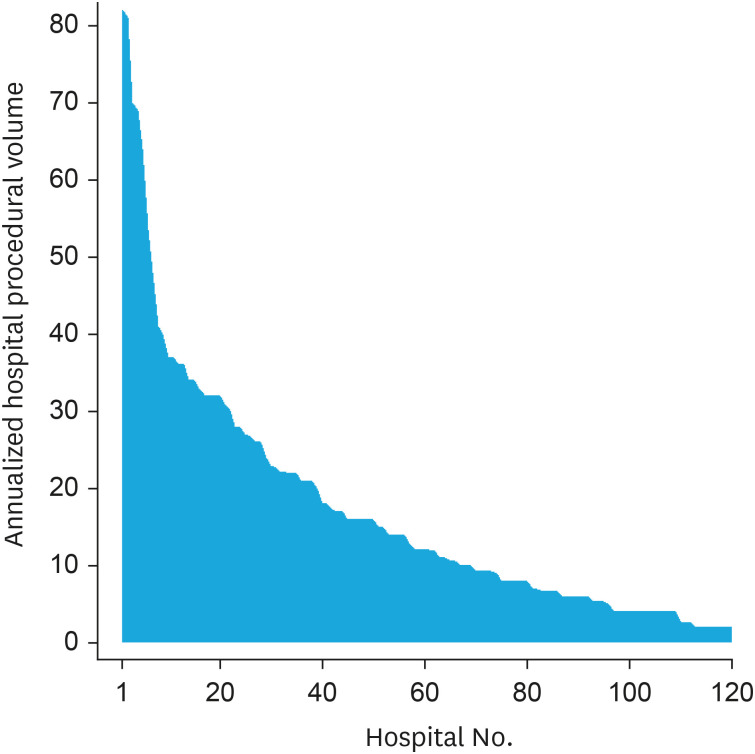
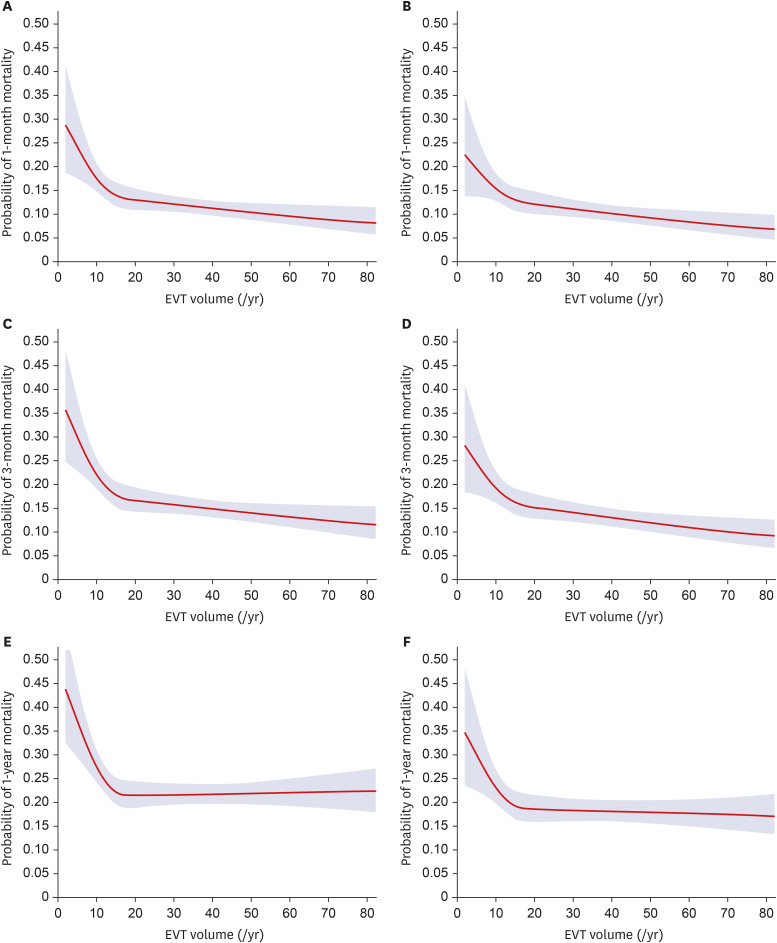
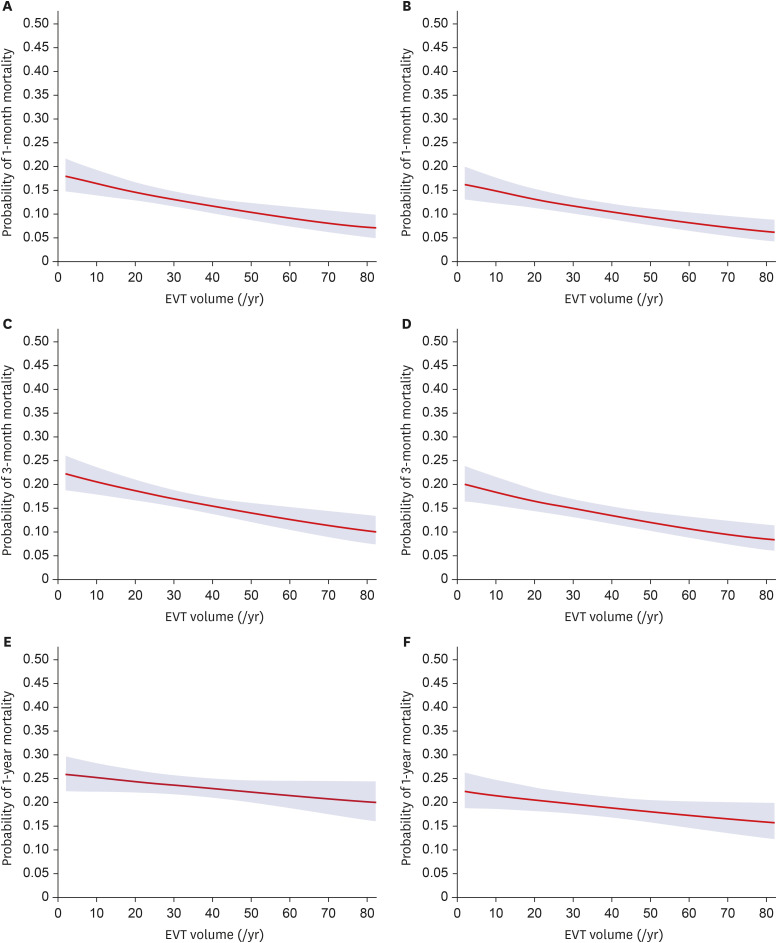
National audit data on the quality of acute stroke care in patients admitted via emergency department, within 7 days of onset, in hospitals that treated ≥ 10 stroke cases during the audit period were analyzed. Ischemic stroke cases treated with EVT during the last three audits (2013, 2014, and 2016) were selected for the analysis. Annual EVT case volume per hospital was estimated and analyzed as a continuous and a categorical variable (in quartiles). The primary outcome measure was 1-year mortality as a surrogate of 3-month functional outcome. As post-hoc sensitivity analysis, replication of the study results was examined using the 2018 audit data.
Results
We analyzed 1,746 ischemic stroke cases treated with EVT in 120 acute care hospitals. The median annual EVT case volume was 12.0 cases per hospital, and mortality rates at 1 month, 3 months, and 1 year were 12.7%, 16.6%, and 23.3%, respectively. Q3 and Q4 had 33% lower odds of 1-year mortality than Q1. Adjustments were made for predetermined confounders. Annual EVT case volume cut-off value for 1-year mortality was 15 cases per year (P < 0.02). The same cut-off value was replicated in the sensitivity analysis.
Conclusion
Annual EVT case volume was associated with 1-year mortality. The volume threshold per hospital was 15 cases per year.
Figure
Reference
-
1. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372(11):1019–1030. PMID: 25671798.
Article2. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378(1):11–21. PMID: 29129157.3. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378(8):708–718. PMID: 29364767.
Article4. Powers W, Rabinstein A, Ackerson T, Adeoye O, Bambakidis N, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49(3):e46–110. PMID: 29367334.
Article5. Smith EE, Saver JL, Cox M, Liang L, Matsouaka R, Xian Y, et al. Increase in endovascular therapy in get with the guidelines-stroke after the publication of pivotal trials. Circulation. 2017; 136(24):2303–2310. PMID: 28982689.
Article6. Kang J, Kim SE, Park HK, Cho YJ, Kim JY, Lee KJ, et al. Routing to endovascular treatment of ischemic stroke in Korea: recognition of need for process improvement. J Korean Med Sci. 2020; 35(41):e347. PMID: 33107228.
Article7. The Joint Commission. Primary Stroke Centers. Updated 2022. Accessed June 21, 2022. https://www.jointcommission.org/certification/dsc_neuro2.aspx .8. Jollis JG, Peterson ED, DeLong ER, Mark DB, Collins SR, Muhlbaier LH, et al. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med. 1994; 331(24):1625–1629. PMID: 7969344.
Article9. Jolly SS, Cairns J, Yusuf S, Niemela K, Steg PG, Worthley M, et al. Procedural volume and outcomes with radial or femoral access for coronary angiography and intervention. J Am Coll Cardiol. 2014; 63(10):954–963. PMID: 24269362.
Article10. Strom JB, Wimmer NJ, Wasfy JH, Kennedy K, Yeh RW. Association between operator procedure volume and patient outcomes in percutaneous coronary intervention: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2014; 7(4):560–566. PMID: 24939939.
Article11. Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002; 346(15):1128–1137. PMID: 11948273.
Article12. Vemulapalli S, Carroll JD, Mack MJ, Li Z, Dai D, Kosinski AS, et al. Procedural volume and outcomes for transcatheter aortic-valve replacement. N Engl J Med. 2019; 380(26):2541–2550. PMID: 30946551.
Article13. Shim DH, Kim Y, Roh J, Kang J, Park KP, Cha JK, et al. Hospital volume threshold associated with higher survival after endovascular recanalization therapy for acute ischemic stroke. J Stroke. 2020; 22(1):141–149. PMID: 32027799.
Article14. Adamczyk P, Attenello F, Wen G, He S, Russin J, Sanossian N, et al. Mechanical thrombectomy in acute stroke: utilization variances and impact of procedural volume on inpatient mortality. J Stroke Cerebrovasc Dis. 2013; 22(8):1263–1269. PMID: 23017430.
Article15. Kim BM, Baek JH, Heo JH, Kim DJ, Nam HS, Kim YD. Effect of cumulative case volume on procedural and clinical outcomes in endovascular thrombectomy. Stroke. 2019; 50(5):1178–1183. PMID: 30943886.
Article16. Rinaldo L, Brinjikji W, Rabinstein AA. Transfer to high-volume centers associated with reduced mortality after endovascular treatment of acute stroke. Stroke. 2017; 48(5):1316–1321. PMID: 28336679.
Article17. Stein LK, Mocco J, Fifi J, Jette N, Tuhrim S, Dhamoon MS. Correlations between physician and hospital stroke thrombectomy volumes and outcomes: a nationwide analysis. Stroke. 2021; 52(9):2858–2865. PMID: 34092122.
Article18. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372(1):11–20. PMID: 25517348.19. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372(24):2296–2306. PMID: 25882510.
Article20. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372(24):2285–2295. PMID: 25882376.
Article21. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372(11):1009–1018. PMID: 25671797.
Article22. Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013–2014: national averages and disparities. J Korean Med Sci. 2020; 35(20):e167. PMID: 32449325.
Article23. Park HK, Kim SE, Cho YJ, Kim JY, Oh H, Kim BJ, et al. Quality of acute stroke care in Korea (2008–2014): Retrospective analysis of the nationwide and nonselective data for quality of acute stroke care. Eur Stroke J. 2019; 4(4):337–346. PMID: 31903432.
Article24. Ganesh A, Luengo-Fernandez R, Wharton RM, Gutnikov SA, Silver LE, Mehta Z, et al. Time course of evolution of disability and cause-specific mortality after ischemic stroke: implications for trial design. J Am Heart Assoc. 2017; 6(6):e005788. PMID: 28603141.25. Eriksson M, Norrving B, Terént A, Stegmayr B. Functional outcome 3 months after stroke predicts long-term survival. Cerebrovasc Dis. 2008; 25(5):423–429. PMID: 18349536.
Article26. Alawieh A, Starke RM, Chatterjee AR, Turk A, De Leacy R, Rai AT, et al. Outcomes of endovascular thrombectomy in the elderly: a ‘real-world’ multicenter study. J Neurointerv Surg. 2019; 11(6):545–553. PMID: 30389899.
Article27. Sheth SA, Lee S, Warach SJ, Gralla J, Jahan R, Goyal M, et al. Sex differences in outcome after endovascular stroke therapy for acute ischemic stroke. Stroke. 2019; 50(9):2420–2427. PMID: 31412752.
Article28. Almekhlafi MA, Davalos A, Bonafe A, Chapot R, Gralla J, Pereira VM, et al. Impact of age and baseline NIHSS scores on clinical outcomes in the mechanical thrombectomy using solitaire FR in acute ischemic stroke study. AJNR Am J Neuroradiol. 2014; 35(7):1337–1340. PMID: 24557701.29. Kunz WG, Hunink MG, Dimitriadis K, Huber T, Dorn F, Meinel FG, et al. Cost-effectiveness of endovascular therapy for acute ischemic stroke: a systematic review of the impact of patient age. Radiology. 2018; 288(2):518–526. PMID: 29893641.
Article30. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316(12):1279–1288. PMID: 27673305.
Article31. The Joint Commission. Proposed requirements for the Thrombectomy-capable Stroke Center Certification Program. The Joint Commission;2018. Updated 2022. Accessed November 22, 2021. https://www.jointcommission.org/accreditation-and-certification/certification/certifications-by-setting/hospital-certifications/stroke-certification/advanced-stroke/thrombectomy-capable-stroke-center .32. Jovin TG, Gupta R, Horowitz MB, Grahovac SZ, Jungreis CA, Wechsler L, et al. Pretreatment ipsilateral regional cortical blood flow influences vessel recanalization in intra-arterial thrombolysis for MCA occlusion. AJNR Am J Neuroradiol. 2007; 28(1):164–167. PMID: 17213449.33. Prabhakaran S, Ward E, John S, Lopes DK, Chen M, Temes RE, et al. Transfer delay is a major factor limiting the use of intra-arterial treatment in acute ischemic stroke. Stroke. 2011; 42(6):1626–1630. PMID: 21527756.
Article34. Kim SE, Lee H, Kim JY, Lee KJ, Kang J, Kim BJ, et al. Three-month modified Rankin Scale as a determinant of 5-year cumulative costs after ischemic stroke: An analysis of 11,136 patients in Korea. Neurology. 2020; 94(9):e978–e991. PMID: 32029544.35. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387(10029):1723–1731. PMID: 26898852.
Article36. Moscucci M, Share D, Smith D, O’Donnell MJ, Riba A, McNamara R, et al. Relationship between operator volume and adverse outcome in contemporary percutaneous coronary intervention practice: an analysis of a quality-controlled multicenter percutaneous coronary intervention clinical database. J Am Coll Cardiol. 2005; 46(4):625–632. PMID: 16098426.
Article37. Rashid M, Sperrin M, Ludman PF, O’Neill D, Nicholas O, de Belder MA, et al. Impact of operator volume for percutaneous coronary intervention on clinical outcomes: what do the numbers say? Eur Heart J Qual Care Clin Outcomes. 2016; 2(1):16–22. PMID: 29474590.
Article38. Tie HT, Shi R, Zhou Q, Wang K, Zheng XQ, Wu QC. Annual case volume on mortality after coronary artery bypass grafting: a dose-response meta-analysis. Interact Cardiovasc Thorac Surg. 2019; 29(4):568–575. PMID: 31230080.
Article39. Jayaram N, Spertus JA, O’Byrne ML, Chan PS, Kennedy KF, Bergersen L, et al. Relationship between hospital procedure volume and complications following congenital cardiac catheterization: a report from the IMproving Pediatric and Adult Congenital Treatment (IMPACT) registry. Am Heart J. 2017; 183:118–128. PMID: 27979036.
Article40. Huo YR, Phan K, Morris DL, Liauw W. Systematic review and a meta-analysis of hospital and surgeon volume/outcome relationships in colorectal cancer surgery. J Gastrointest Oncol. 2017; 8(3):534–546. PMID: 28736640.
Article41. Jani VB, To CY, Patel A, Kelkar PS, Richards B, Fessler RD. 116 Effect of annual hospital procedure volume on outcomes after mechanical thrombectomy in acute ischemic stroke patients: an analysis of 13 502 procedures. Neurosurgery. 2016; 63(Suppl 1):149.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- National Trends in Medical Costs and Prognosis of Acute Ischemic Stroke Patients in Endovascular Thrombectomy Era: Analysis Using Medical Claim Data in Korea
- Endovascular recanalization therapy for patients with acute ischemic stroke with hidden aortic dissection: A case series
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis