Korean Circ J.
2022 Sep;52(9):643-658. 10.4070/kcj.2022.0190.
Generation and Application of Directly Reprogrammed Endothelial Cells
- Affiliations
-
- 1Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Graduate School of Medical Science, Brain Korea 21 Project, Yonsei University College of Medicine, Seoul, Korea
- 3Research and Development Center, KarisBio Inc., Seoul, Korea
- 4Department of Medicine, Division of Cardiology, Emory University School of Medicine, Atlanta, GA, USA
- KMID: 2532931
- DOI: http://doi.org/10.4070/kcj.2022.0190
Abstract
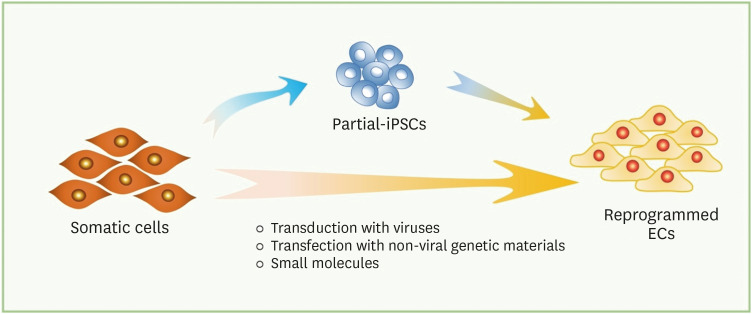
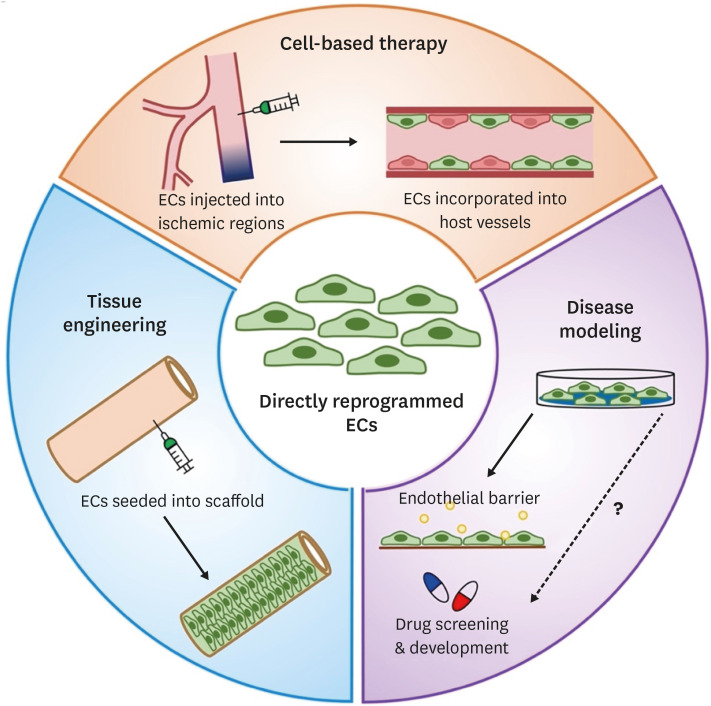
- Cell-based therapy has emerged as a promising option for treating advanced ischemic cardiovascular disease by inducing vascular regeneration. However, clinical trials with adult cells turned out disappointing in general. As a newer approach, direct reprogramming has emerged to efficiently generate endothelial cells (ECs), which can promote neovascularization and vascular regeneration. This review provides recent updates on the direct endothelial reprogramming. In general, directly reprogrammed ECs can be generated by two approaches: one by transitioning through a plastic intermediate state and the other in a one-step transition without any intermediate states toward pluripotency. Moreover, the methods to deliver reprogramming factors and chemicals for the fate conversion are highlighted. Next, the therapeutic effects of the directly reprogrammed ECs on animal models are reviewed in detail. Other applications using directly reprogrammed ECs, such as tissue engineering and disease modeling, are also discussed. Lastly, the remaining questions and foremost challenges are addressed.
Keyword
Figure
Reference
-
1. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021; 143:e254–e743. PMID: 33501848.2. Bhagra SK, Pettit S, Parameshwar J. Cardiac transplantation: indications, eligibility and current outcomes. Heart. 2019; 105:252–260. PMID: 30209127.3. Farber A. Chronic limb-threatening ischemia. N Engl J Med. 2018; 379:171–180. PMID: 29996085.4. Kim W. Critical determinants of chronic limb threatening ischemia after endovascular treatment. Korean Circ J. 2022; 52:441–443. PMID: 35656902.5. Takahashi K, Tanabe K, Ohnuki M, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007; 131:861–872. PMID: 18035408.6. Yu J, Vodyanik MA, Smuga-Otto K, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007; 318:1917–1920. PMID: 18029452.7. Wang ZZ, Au P, Chen T, et al. Endothelial cells derived from human embryonic stem cells form durable blood vessels in vivo. Nat Biotechnol. 2007; 25:317–318. PMID: 17322871.8. Taura D, Sone M, Homma K, et al. Induction and isolation of vascular cells from human induced pluripotent stem cells--brief report. Arterioscler Thromb Vasc Biol. 2009; 29:1100–1103. PMID: 19423866.9. Rufaihah AJ, Huang NF, Jamé S, et al. Endothelial cells derived from human iPSCS increase capillary density and improve perfusion in a mouse model of peripheral arterial disease. Arterioscler Thromb Vasc Biol. 2011; 31:e72–e79. PMID: 21836062.10. Lee SJ, Sohn YD, Andukuri A, et al. Enhanced therapeutic and long-term dynamic vascularization effects of human pluripotent stem cell-derived endothelial cells encapsulated in a nanomatrix gel. Circulation. 2017; 136:1939–1954. PMID: 28972000.11. Clayton ZE, Yuen GS, Sadeghipour S, et al. A comparison of the pro-angiogenic potential of human induced pluripotent stem cell derived endothelial cells and induced endothelial cells in a murine model of peripheral arterial disease. Int J Cardiol. 2017; 234:81–89. PMID: 28209385.12. Lai WH, Ho JC, Chan YC, et al. Attenuation of hind-limb ischemia in mice with endothelial-like cells derived from different sources of human stem cells. PLoS One. 2013; 8:e57876. PMID: 23472116.13. Zhou Q, Brown J, Kanarek A, Rajagopal J, Melton DA. In vivo reprogramming of adult pancreatic exocrine cells to beta-cells. Nature. 2008; 455:627–632. PMID: 18754011.14. Vierbuchen T, Ostermeier A, Pang ZP, Kokubu Y, Südhof TC, Wernig M. Direct conversion of fibroblasts to functional neurons by defined factors. Nature. 2010; 463:1035–1041. PMID: 20107439.15. Ieda M, Fu JD, Delgado-Olguin P, et al. Direct reprogramming of fibroblasts into functional cardiomyocytes by defined factors. Cell. 2010; 142:375–386. PMID: 20691899.16. Szabo E, Rampalli S, Risueño RM, et al. Direct conversion of human fibroblasts to multilineage blood progenitors. Nature. 2010; 468:521–526. PMID: 21057492.17. Sekiya S, Suzuki A. Direct conversion of mouse fibroblasts to hepatocyte-like cells by defined factors. Nature. 2011; 475:390–393. PMID: 21716291.18. Pang ZP, Yang N, Vierbuchen T, et al. Induction of human neuronal cells by defined transcription factors. Nature. 2011; 476:220–223. PMID: 21617644.19. Lee CS, Kim J, Cho HJ, Kim HS. Cardiovascular regeneration via stem cells and direct reprogramming: a review. Korean Circ J. 2022; 52:341–353. PMID: 35502566.20. Ginsberg M, James D, Ding BS, et al. Efficient direct reprogramming of mature amniotic cells into endothelial cells by ETS factors and TGFβ suppression. Cell. 2012; 151:559–575. PMID: 23084400.21. Margariti A, Winkler B, Karamariti E, et al. Direct reprogramming of fibroblasts into endothelial cells capable of angiogenesis and reendothelialization in tissue-engineered vessels. Proc Natl Acad Sci U S A. 2012; 109:13793–13798. PMID: 22869753.22. Kurian L, Sancho-Martinez I, Nivet E, et al. Conversion of human fibroblasts to angioblast-like progenitor cells. Nat Methods. 2013; 10:77–83. PMID: 23202434.23. Li J, Huang NF, Zou J, et al. Conversion of human fibroblasts to functional endothelial cells by defined factors. Arterioscler Thromb Vasc Biol. 2013; 33:1366–1375. PMID: 23520160.24. Han JK, Chang SH, Cho HJ, et al. Direct conversion of adult skin fibroblasts to endothelial cells by defined factors. Circulation. 2014; 130:1168–1178. PMID: 25186941.25. Morita R, Suzuki M, Kasahara H, et al. ETS transcription factor ETV2 directly converts human fibroblasts into functional endothelial cells. Proc Natl Acad Sci U S A. 2015; 112:160–165. PMID: 25540418.26. Wong WT, Cooke JP. Therapeutic transdifferentiation of human fibroblasts into endothelial cells using forced expression of lineage-specific transcription factors. J Tissue Eng. 2016; 7:2041731416628329. PMID: 27081470.27. Lee S, Park C, Han JW, et al. Direct reprogramming of human dermal fibroblasts into endothelial cells using ER71/ETV2. Circ Res. 2017; 120:848–861. PMID: 28003219.28. Cheng F, Zhang Y, Wang Y, et al. Conversion of human adipose-derived stem cells into functional and expandable endothelial-like cells for cell-based therapies. Stem Cell Res Ther. 2018; 9:350. PMID: 30558659.29. Chen T, Karamariti E, Hong X, et al. DKK3 (Dikkopf-3) transdifferentiates fibroblasts into functional endothelial cells-brief report. Arterioscler Thromb Vasc Biol. 2019; 39:765–773. PMID: 30816803.30. Kim JJ, Kim DH, Lee JY, et al. cAMP/EPAC signaling enables ETV2 to induce endothelial cells with high angiogenesis potential. Mol Ther. 2020; 28:466–478. PMID: 31864907.31. Bersini S, Schulte R, Huang L, Tsai H, Hetzer MW. Direct reprogramming of human smooth muscle and vascular endothelial cells reveals defects associated with aging and Hutchinson-Gilford progeria syndrome. eLife. 2020; 9:e54383. PMID: 32896271.32. Han JK, Shin Y, Sohn MH, et al. Direct conversion of adult human fibroblasts into functional endothelial cells using defined factors. Biomaterials. 2021; 272:120781. PMID: 33848809.33. Rezvani M, Español-Suñer R, Malato Y, et al. In vivo hepatic reprogramming of myofibroblasts with AAV vectors as a therapeutic strategy for liver fibrosis. Cell Stem Cell. 2016; 18:809–816. PMID: 27257763.34. Okita K, Nakagawa M, Hyenjong H, Ichisaka T, Yamanaka S. Generation of mouse induced pluripotent stem cells without viral vectors. Science. 2008; 322:949–953. PMID: 18845712.35. Yu J, Hu K, Smuga-Otto K, et al. Human induced pluripotent stem cells free of vector and transgene sequences. Science. 2009; 324:797–801. PMID: 19325077.36. Cho J, Kim S, Lee H, et al. Regeneration of infarcted mouse hearts by cardiovascular tissue formed via the direct reprogramming of mouse fibroblasts. Nat Biomed Eng. 2021; 5:880–896. PMID: 34426676.37. Sayed N, Wong WT, Ospino F, et al. Transdifferentiation of human fibroblasts to endothelial cells: role of innate immunity. Circulation. 2015; 131:300–309. PMID: 25359165.38. Li J, Zhu Y, Li N, et al. Upregulation of ETV2 expression promotes endothelial differentiation of human dental pulp stem cells. Cell Transplant. 2021; 30:963689720978739. PMID: 33522307.39. Pavathuparambil Abdul Manaph N, Al-Hawwas M, Bobrovskaya L, Coates PT, Zhou XF. Urine-derived cells for human cell therapy. Stem Cell Res Ther. 2018; 9:189. PMID: 29996911.40. Zhou T, Benda C, Dunzinger S, et al. Generation of human induced pluripotent stem cells from urine samples. Nat Protoc. 2012; 7:2080–2089. PMID: 23138349.41. Zhang XB. Cellular reprogramming of human peripheral blood cells. Genomics Proteomics Bioinformatics. 2013; 11:264–274. PMID: 24060839.42. Kim EY, Page P, Dellefave-Castillo LM, McNally EM, Wyatt EJ. Direct reprogramming of urine-derived cells with inducible MyoD for modeling human muscle disease. Skelet Muscle. 2016; 6:32. PMID: 27651888.43. Tang W, Guo R, Shen SJ, et al. Chemical cocktails enable hepatic reprogramming of human urine-derived cells with a single transcription factor. Acta Pharmacol Sin. 2019; 40:620–629. PMID: 30315254.44. Omrani MR, Yaqubi M, Mohammadnia A. Transcription factors in regulatory and protein subnetworks during generation of neural stem cells and neurons from direct reprogramming of non-fibroblastic cell sources. Neuroscience. 2018; 380:63–77. PMID: 29653196.45. Horisawa K, Suzuki A. Direct cell-fate conversion of somatic cells: toward regenerative medicine and industries. Proc Jpn Acad Ser B Phys Biol Sci. 2020; 96:131–158.46. Engle SJ, Puppala D. Integrating human pluripotent stem cells into drug development. Cell Stem Cell. 2013; 12:669–677. PMID: 23746976.47. Merkle FT, Eggan K. Modeling human disease with pluripotent stem cells: from genome association to function. Cell Stem Cell. 2013; 12:656–668. PMID: 23746975.48. Gu M, Shao NY, Sa S, et al. Patient-specific iPSC-derived endothelial cells uncover pathways that protect against pulmonary hypertension in BMPR2 mutation carriers. Cell Stem Cell. 2017; 20:490–504.e5. PMID: 28017794.49. Sa S, Gu M, Chappell J, et al. Induced pluripotent stem cell model of pulmonary arterial hypertension reveals novel gene expression and patient specificity. Am J Respir Crit Care Med. 2017; 195:930–941. PMID: 27779452.50. West JD, Austin ED, Gaskill C, et al. Identification of a common Wnt-associated genetic signature across multiple cell types in pulmonary arterial hypertension. Am J Physiol Cell Physiol. 2014; 307:C415–C430. PMID: 24871858.51. Theodoris CV, Li M, White MP, et al. Human disease modeling reveals integrated transcriptional and epigenetic mechanisms of NOTCH1 haploinsufficiency. Cell. 2015; 160:1072–1086. PMID: 25768904.52. Wu Y, Hu Z, Li Z, et al. In situ genetic correction of F8 intron 22 inversion in hemophilia A patient-specific iPSCs. Sci Rep. 2016; 6:18865. PMID: 26743572.53. Ang YS, Rivas RN, Ribeiro AJ, et al. Disease model of GATA4 mutation reveals transcription factor cooperativity in human cardiogenesis. Cell. 2016; 167:1734–1749.e22. PMID: 27984724.54. Maherali N, Sridharan R, Xie W, et al. Directly reprogrammed fibroblasts show global epigenetic remodeling and widespread tissue contribution. Cell Stem Cell. 2007; 1:55–70. PMID: 18371336.55. Studer L, Vera E, Cornacchia D. Programming and reprogramming cellular age in the era of induced pluripotency. Cell Stem Cell. 2015; 16:591–600. PMID: 26046759.56. Hong X, Margariti A, Le Bras A, et al. Transdifferentiated human vascular smooth muscle cells are a new potential cell source for endothelial regeneration. Sci Rep. 2017; 7:5590. PMID: 28717251.57. Baum C, Düllmann J, Li Z, et al. Side effects of retroviral gene transfer into hematopoietic stem cells. Blood. 2003; 101:2099–2114. PMID: 12511419.58. Ranzani M, Cesana D, Bartholomae CC, et al. Lentiviral vector-based insertional mutagenesis identifies genes associated with liver cancer. Nat Methods. 2013; 10:155–161. PMID: 23314173.59. Li Z, Düllmann J, Schiedlmeier B, et al. Murine leukemia induced by retroviral gene marking. Science. 2002; 296:497. PMID: 11964471.60. Suknuntha K, Tao L, Brok-Volchanskaya V, D’Souza SS, Kumar A, Slukvin I. Optimization of synthetic mRNA for highly efficient translation and its application in the generation of endothelial and hematopoietic cells from human and primate pluripotent stem cells. Stem Cell Rev Rep. 2018; 14:525–534. PMID: 29520567.61. Wang K, Lin RZ, Hong X, et al. Robust differentiation of human pluripotent stem cells into endothelial cells via temporal modulation of ETV2 with modified mRNA. Sci Adv. 2020; 6:eaba7606. PMID: 32832668.62. Cho HJ, Lee N, Lee JY, et al. Role of host tissues for sustained humoral effects after endothelial progenitor cell transplantation into the ischemic heart. J Exp Med. 2007; 204:3257–3269. PMID: 18070934.63. van der Bogt KE, Sheikh AY, Schrepfer S, et al. Comparison of different adult stem cell types for treatment of myocardial ischemia. Circulation. 2008; 118:S121–S129. PMID: 18824743.64. Vasu S, Zhou J, Chen J, Johnston PV, Kim DH. Biomaterials-based approaches for cardiac regeneration. Korean Circ J. 2021; 51:943–960. PMID: 34854577.65. Oh JE, Jung C, Yoon YS. Human induced pluripotent stem cell-derived vascular cells: recent progress and future directions. J Cardiovasc Dev Dis. 2021; 8:148. PMID: 34821701.66. Garlanda C, Dejana E. Heterogeneity of endothelial cells. Specific markers. Arterioscler Thromb Vasc Biol. 1997; 17:1193–1202. PMID: 9261246.67. Paik DT, Tian L, Williams IM, et al. Single-cell RNA sequencing unveils unique transcriptomic signatures of organ-specific endothelial cells. Circulation. 2020; 142:1848–1862. PMID: 32929989.68. Nolan DJ, Ginsberg M, Israely E, et al. Molecular signatures of tissue-specific microvascular endothelial cell heterogeneity in organ maintenance and regeneration. Dev Cell. 2013; 26:204–219. PMID: 23871589.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Induced Pluripotent Stem Cells: Next Generation Stem Cells to Clinical Applications
- In Vitro Culture of Endothelial Cell and Smooth Muscle Cell for Studying Vascular Diseases
- Trends and clinical application of induced pluripotent stem cells
- Angiogenesis and cell therapy
- Detection of Circulating Tumor Cells Using Three-dimensional and Conditionally Reprogrammed Culture Methods