Ann Hepatobiliary Pancreat Surg.
2022 Aug;26(3):244-250. 10.14701/ahbps.21-152.
Effect of early oral nutrition supplement using Encover in patients undergoing hepato-biliary-pancreatic surgery
- Affiliations
-
- 1Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2532640
- DOI: http://doi.org/10.14701/ahbps.21-152
Abstract
- Backgrounds/Aims
Early recovery after surgery has become a popular trend. The aim of this study was to evaluate effect of nutritional intervention using Encover, an oral nutritional supplement, in patients undergoing hepato-biliary-pancreatic surgery.
Methods
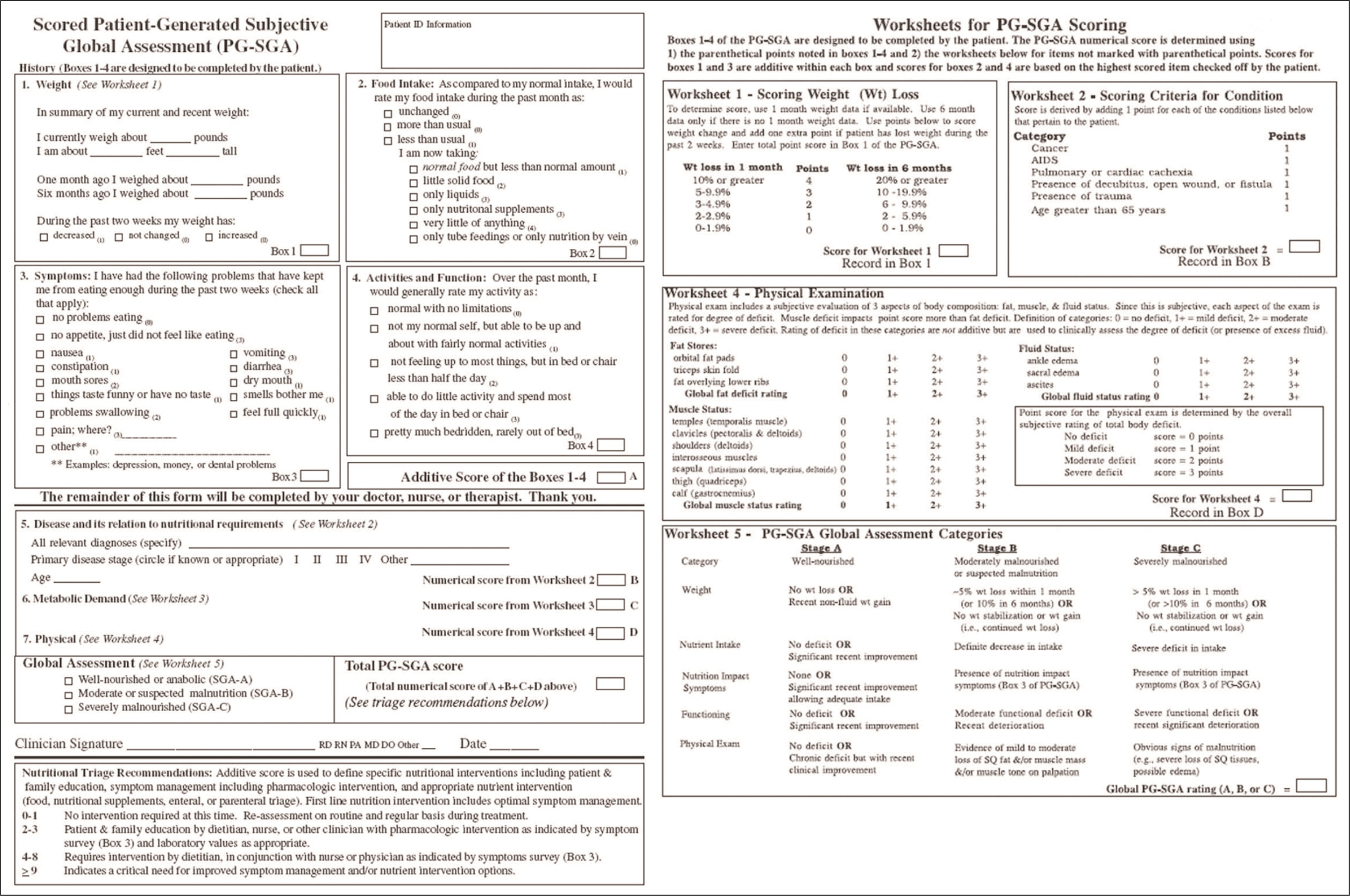
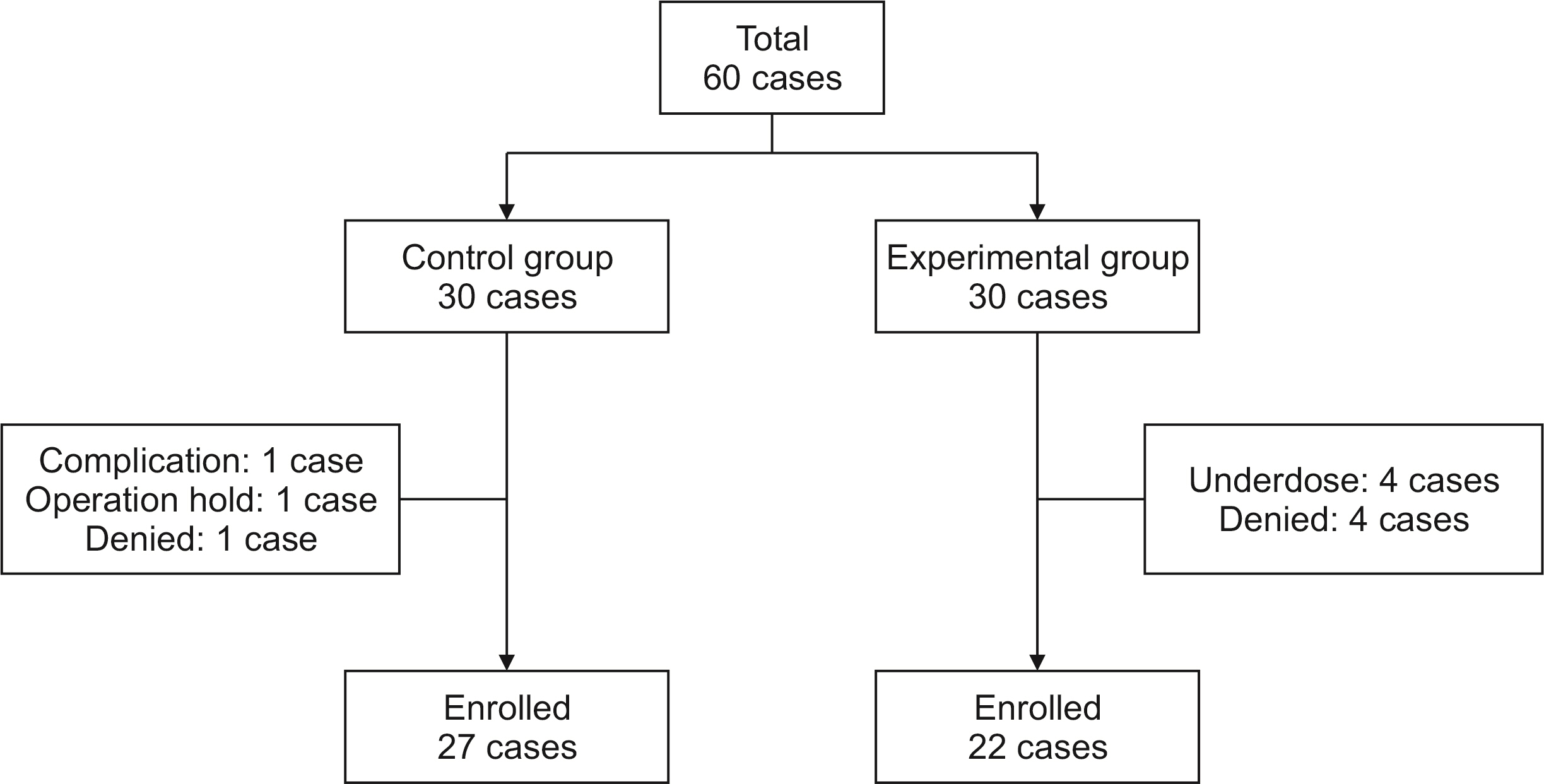
This single center, prospective case-control study was conducted in Gangnam Severance Hospital from September 2018 to April 2019. Through randomization, patients were divided into an experimental group (30 patients) and a control group (30 patients). At postoperative seven days, the experimental group was instructed to take two packs of Encover (JW Pharmaceutical, Seoul, Korea) daily for seven days. Body cell mass index was measured at seven days after surgery and 14 days after discharge and Patient-Generated Subjective Global Assessment (PG-SGA) was performed at 14 days after discharge.
Results
Body cell mass index during outpatient follow-up was significantly decreased compared to that at discharge in both groups. However, the amount of body cell mass index showed no significant difference between postoperative seven days and outpatient follow-up in either group. During outpatient follow-up, the experimental group had a higher mean value of PG-SGA score than the control group (11.32 ± 3.46 vs. 9.48 ± 3.97; p = 0.037).
Conclusions
Short-term Encover doses after surgery may not produce significant results in weight gain or other body cell mass index. Encover did not significantly affect other dietary conditions based on PG-SGA.
Figure
Reference
-
1. Bistrian BR, Blackburn GL, Hallowell E, Heddle R. 1974; Protein status of general surgical patients. JAMA. 230:858–860. DOI: 10.1001/jama.1974.03240060028025. PMID: 4213823.2. Kondrup J, Johansen N, Plum LM, Bak L, Larsen IH, Martinsen A, et al. 2002; Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin Nutr. 21:461–468. DOI: 10.1054/clnu.2002.0585. PMID: 12468365.3. Norman K, Pichard C, Lochs H, Pirlich M. 2008; Prognostic impact of disease-related malnutrition. Clin Nutr. 27:5–15. DOI: 10.1016/j.clnu.2007.10.007. PMID: 18061312.4. Yu YD, Han JH, Jung SW, Kim DS. 2019; Safety and efficacy of peripheral nutrition fluid (MG-TNA®) in patients undergoing surgery for hepatobiliary and pancreatic disease: results of a phase 4 trial. Ann Hepatobiliary Pancreat Surg. 23:133–137. DOI: 10.14701/ahbps.2019.23.2.133. PMID: 31225414. PMCID: PMC6558125.5. Nanashima A, Hiyoshi M, Imamura N, Yano K, Hamada T, Hamada R, et al. 2019; Clinical significance of preoperative nutritional parameter and patient outcomes after pancreatectomy: a retrospective study at two academic institute. Ann Hepatobiliary Pancreat Surg. 23:168–173. DOI: 10.14701/ahbps.2019.23.2.168. PMID: 31225419. PMCID: PMC6558137.6. Correia MI, Waitzberg DL. 2003; The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 22:235–239. DOI: 10.1016/S0261-5614(02)00215-7. PMID: 12765661.7. Schricker T, Wykes L, Eberhart L, Carli F, Meterissian S. 2005; Randomized clinical trial of the anabolic effect of hypocaloric parenteral nutrition after abdominal surgery. Br J Surg. 92:947–953. DOI: 10.1002/bjs.5105. PMID: 16034820.8. Shin SH, Kang WH, Han IW, You Y, Lee H, Kim H, et al. 2020; National survey of Korean hepatobiliary-pancreatic surgeons on attitudes about the enhanced recovery after surgery protocol. Ann Hepatobiliary Pancreat Surg. 24:477–483. DOI: 10.14701/ahbps.2020.24.4.477. PMID: 33234751. PMCID: PMC7691206.9. Fung AKY, Chong CCN, Lai PBS. 2020; ERAS in minimally invasive hepatectomy. Ann Hepatobiliary Pancreat Surg. 24:119–126. DOI: 10.14701/ahbps.2020.24.2.119. PMID: 32457255. PMCID: PMC7271107.10. Cavallaro P, Bordeianou L. 2019; Implementation of an ERAS pathway in colorectal surgery. Clin Colon Rectal Surg. 32:102–108. DOI: 10.1055/s-0038-1676474. PMID: 30833858. PMCID: PMC6395097.11. Zaghiyan K, Felder S, Ovsepyan G, Murrell Z, Sokol T, Moore B, et al. 2013; A prospective randomized controlled trial of sugared chewing gum on gastrointestinal recovery after major colorectal surgery in patients managed with early enteral feeding. Dis Colon Rectum. 56:328–335. DOI: 10.1097/DCR.0b013e31827e4971. PMID: 23392147.12. Tanaka M. 2005; Gastroparesis after a pylorus-preserving pancreatoduodenectomy. Surg Today. 35:345–350. DOI: 10.1007/s00595-004-2961-8. PMID: 15864414.13. Kang Y, Park S, Kim S, Kim SY, Koh H. 2019; Therapeutic efficacy of exclusive enteral nutrition with specific polymeric diet in pediatric Crohn's disease. Pediatr Gastroenterol Hepatol Nutr. 22:72–79. DOI: 10.5223/pghn.2019.22.1.72. PMID: 30671376. PMCID: PMC6333584.14. Kong SH, Park JS, Lee IK, Ryu SW, Park YK, Yang HK, et al. 2017; Postoperative oral nutritional supplementation after major gastrointestinal surgery: a randomized controlled clinical trial. Asia Pac J Clin Nutr. 26:811–819. DOI: 10.6133/apjcn.112016.02. PMID: 28802290.15. Okamura Y, Maeda A, Matsunaga K, Kanemoto H, Uesaka K. 2012; Negative impact of low body mass index on surgical outcomes after hepatectomy for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 19:449–457. DOI: 10.1007/s00534-011-0461-y. PMID: 21983894.16. Kim SH, Shon JY, Park JS, Kim JW, Kang JH, Yun EY, et al. 2016; Change in dietary intake and nutritional status using Mealworms as hospital meal in postoperative patients. J Korean Diet Assoc. 22:292–309. DOI: 10.14373/JKDA.2016.22.4.292.17. Salacinski AJ, Howell SM, Hill DL. 2018; Validity of the InBody 520™ to predict metabolic rate in apparently healthy adults. J Sports Med Phys Fitness. 58:1275–1280. DOI: 10.23736/S0022-4707.17.06719-6. PMID: 28558441.18. Ogawa H, Fujitani K, Tsujinaka T, Imanishi K, Shirakata H, Kantani A, et al. 2011; InBody 720 as a new method of evaluating visceral obesity. Hepatogastroenterology. 58:42–44. PMID: 21510284.19. Ntineri A, Prapa S, Bountzona I, Menti A, Stergiou GS. 2021; Validation of the single-cuff oscillometric blood pressure monitor InBody BPBIO750 for public spaces according to the Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization Universal Standard. Blood Press Monit. 26:146–148. DOI: 10.1097/MBP.0000000000000507. PMID: 33323723.20. De Groot LM, Lee G, Ackerie A, van der Meij BS. 2020; Malnutrition screening and assessment in the cancer care ambulatory setting: mortality predictability and validity of the Patient-Generated Subjective Global Assessment Short form (PG-SGA SF) and the GLIM criteria. Nutrients. 12:2287. DOI: 10.3390/nu12082287. PMID: 32751724. PMCID: PMC7468976.21. Nitichai N, Angkatavanich J, Somlaw N, Voravud N, Lertbutsayanukul C. 2019; Validation of the Scored Patient-Generated Subjective Global Assessment (PG-SGA) in Thai setting and association with nutritional parameters in cancer patients. Asian Pac J Cancer Prev. 20:1249–1255. DOI: 10.31557/APJCP.2019.20.4.1249. PMID: 31030501. PMCID: PMC6948895.22. Wiegert EVM, Padilha PC, Peres WAF. 2017; Performance of Patient-Generated Subjective Global Assessment (PG-SGA) in patients with advanced cancer in palliative care. Nutr Clin Pract. 32:675–681. DOI: 10.1177/0884533617725071. PMID: 28850795.23. Du H, Liu B, Xie Y, Liu J, Wei Y, Hu H, et al. 2017; Comparison of different methods for nutrition assessment in patients with tumors. Oncol Lett. 14:165–170. DOI: 10.3892/ol.2017.6154. PMID: 28693149. PMCID: PMC5494893.24. Zhang YH, Xie FY, Chen YW, Wang HX, Tian WX, Sun WG, et al. 2018; Evaluating the nutritional status of oncology patients and its association with quality of life. Biomed Environ Sci. 31:637–644. DOI: 10.3967/bes2018.088. PMID: 30369342.25. You JW, Lee SJ, Kim YE, Cho YJ, Jeong YY, Kim HC, et al. 2013; Association between weight change and clinical outcomes in critically ill patients. J Crit Care. 28:923–927. DOI: 10.1016/j.jcrc.2013.07.055. PMID: 24075294.26. Ghorabi S, Ardehali H, Amiri Z, Vahdat Shariatpanahi Z. 2016; Association of the adductor pollicis muscle thickness with clinical outcomes in intensive care unit patients. Nutr Clin Pract. 31:523–526. DOI: 10.1177/0884533615621547. PMID: 26869610.27. Allison SP. 2000; Malnutrition, disease, and outcome. Nutrition. 16:590–593. DOI: 10.1016/S0899-9007(00)00368-3.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early history of the Korean Association of Hepato-Biliary-Pancreatic Surgery
- Surgical Treatment of Benign Biliary Stricture
- Radiological Diagnosis of Benign Biliary Stricture
- Safety and efficacy of peripheral nutrition fluid (MG-TNA®) in patients undergoing surgery for hepatobiliary and pancreatic disease: Results of a phase 4 trial
- Interventional Management of Benign Biliary Stricture