Ann Hepatobiliary Pancreat Surg.
2022 Aug;26(3):220-228. 10.14701/ahbps.22-041.
Incidence, mortality and survival of gallbladder, extrahepatic bile duct, and pancreatic cancer using Korea central cancer registry database: 1999-2019
- Affiliations
-
- 1Division of Cancer Registration and Surveillance, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 2Center for Liver and Pancreatobiliary Cancer, National Cancer Center, Goyang, Korea
- KMID: 2532637
- DOI: http://doi.org/10.14701/ahbps.22-041
Abstract
- Backgrounds/Aims
In Korea, pancreatic cancer and “gallbladder and extrahepatic bile duct cancer” were ranked the 8th and 9th most frequent cancers in 2019 and the 4th and 6th most common causes of cancer deaths in 2020, respectively.
Methods
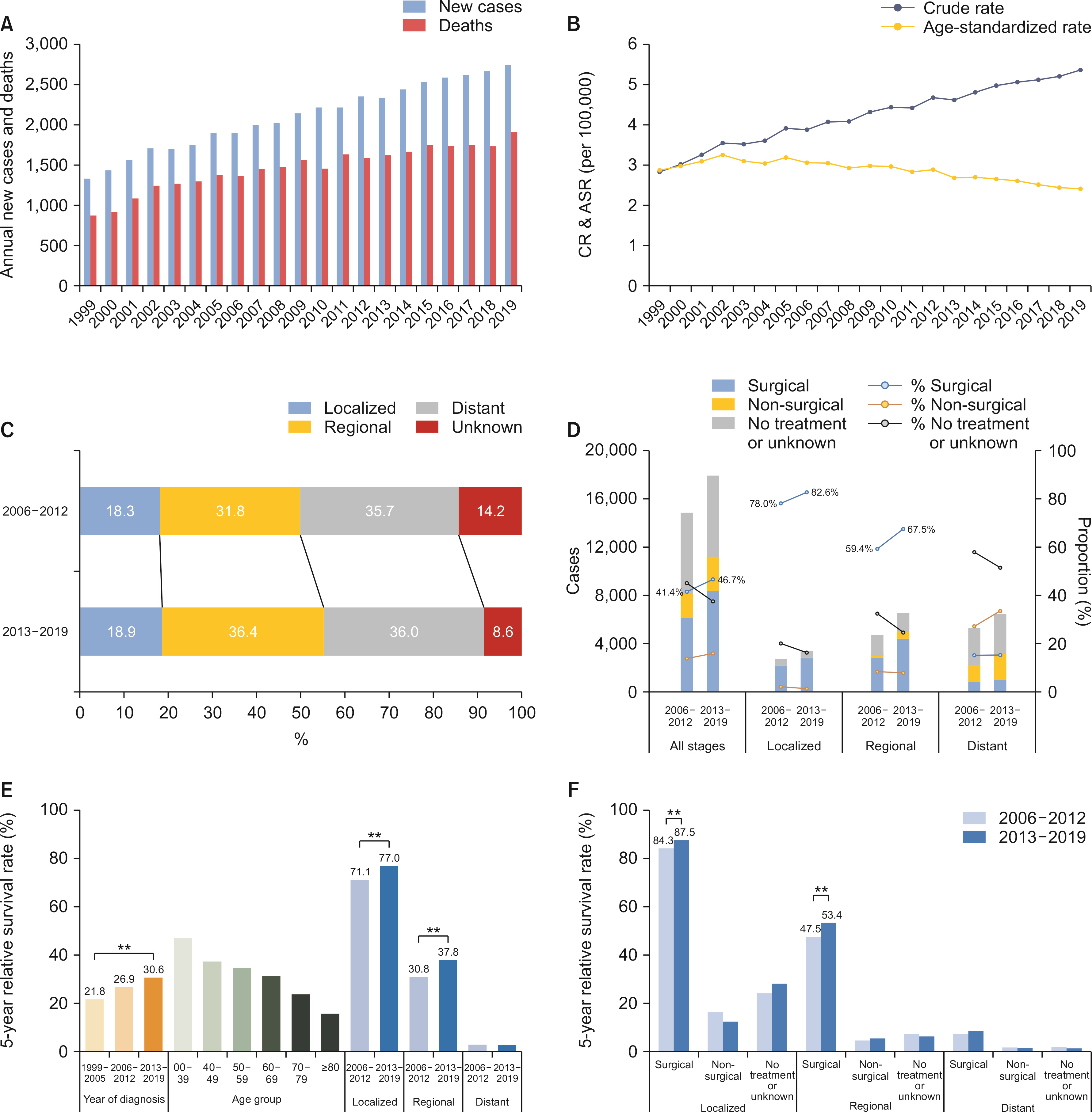
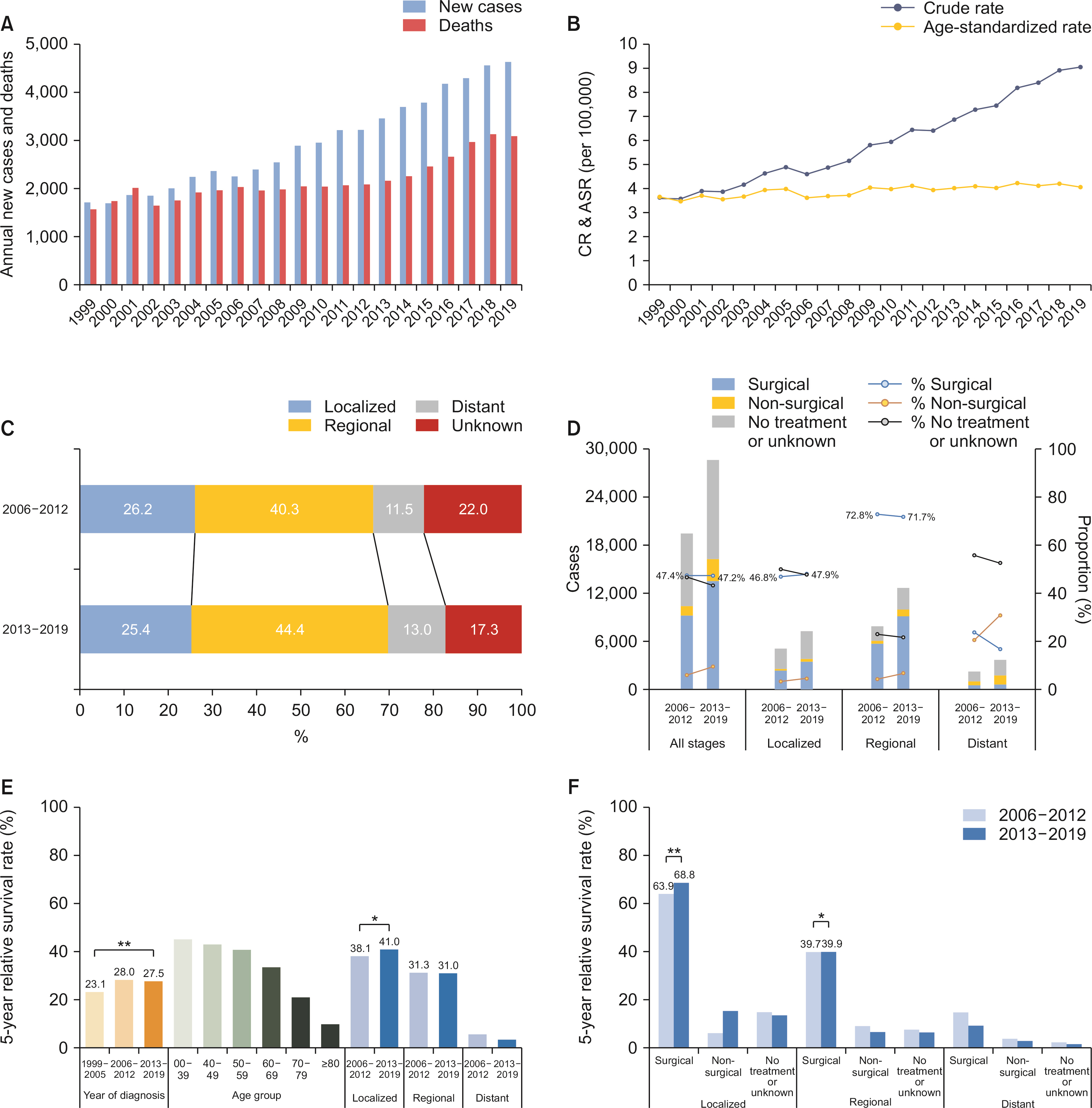
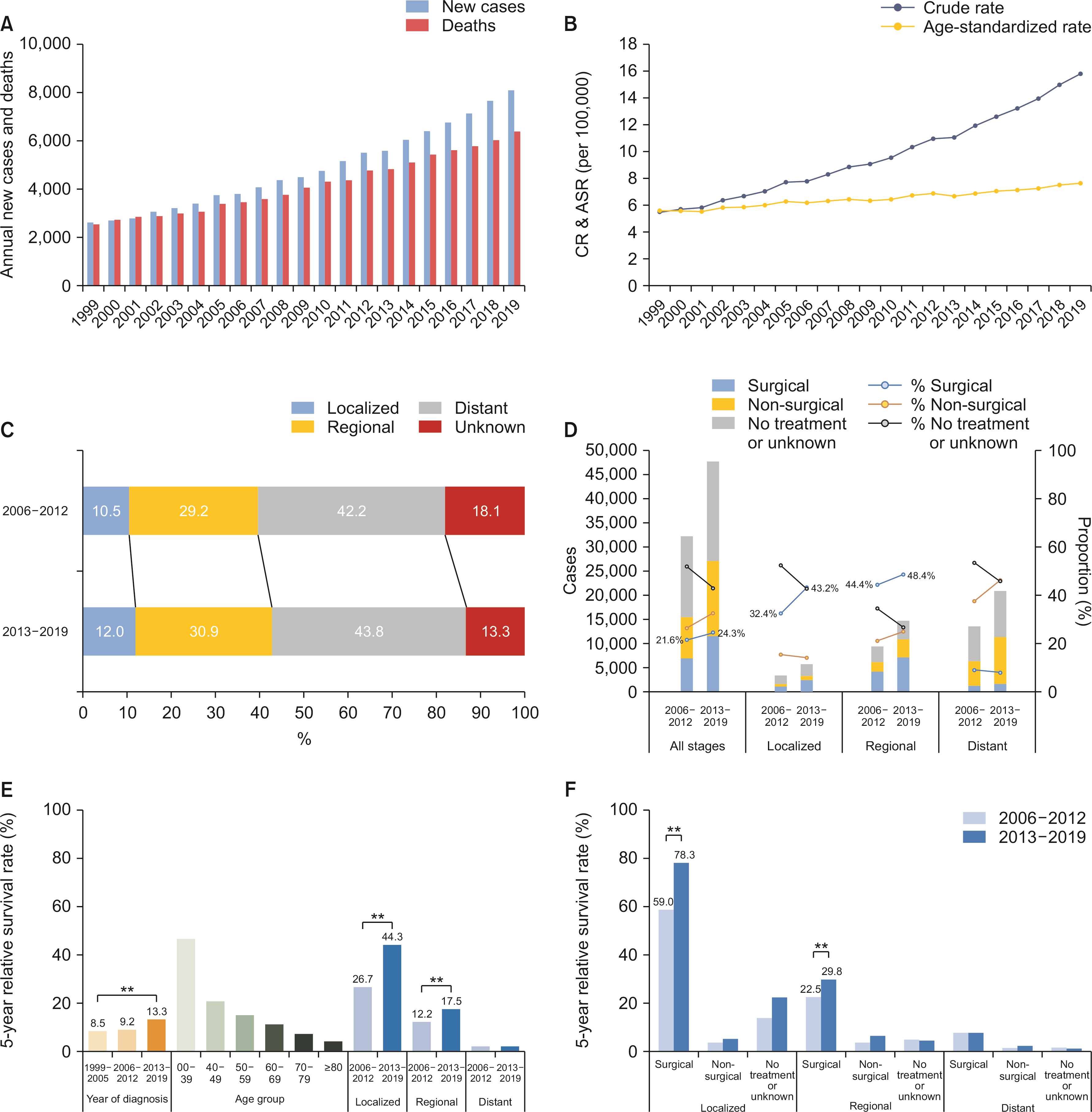
This review provides national cancer statistics and secular trends of 207,521 patients with gallbladder (n = 44,178), extrahepatic bile duct (n = 61,856), and pancreatic cancer (n = 101,487) between 1999 and 2019 in Korea.
Results
The crude incidence rate in both sexes increased in the gallbladder (2.8 to 5.4 per 100,000), extrahepatic bile duct (3.6 to 9.0), and pancreatic cancer (5.5 to 15.8). The age-standardized incidence rate in both sexes significantly increased in the extrahepatic bile duct (3.7 to 4.1) and pancreatic (5.6 to 7.6) cancers but decreased in gallbladder cancer (2.9 to 2.4). The overall 5-year relative survival rate increased in the gallbladder (21.8% to 30.6%), extrahepatic bile duct (23.1% to 27.5%), and pancreatic (8.5% to 13.3%) cancers. Between 2006 and 2019, the proportion of localized or regional stages remained stable. The proportion of surgical treatment within the first 4 months after diagnosis was relatively higher in the gallbladder (42.2%) and extrahepatic bile duct (45.9%) cancers than in pancreatic cancer (22.2%).
Conclusions
The crude incidence and mortality rates of the gallbladder, extrahepatic bile duct, and pancreatic cancer are steadily increasing in Korea, and the prognosis remains poor. Early detection, active application of surgical treatment, and minimization of the proportion of untreated patients are required to improve the survival rates of these cancers.
Keyword
Figure
Reference
-
1. Kang MJ, Won YJ, Lee JJ, Jung KW, Kim HJ, Kong HJ, et al. 2022; Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treat. 54:330–344. DOI: 10.4143/crt.2022.128. PMID: 35313102. PMCID: PMC9016309.2. Statistics Korea. 2020. 236 causes of death, 2020 [Internet]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E07&vw_cd=MT_ZTITLE&list_id=F_27&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=MT_ZTITLE&path=%252FstatisticsList%252FstatisticsListIndex.do. cited 2022 May 5. Daejeon: Statistics Korea.3. Korea Central Cancer Registry. 2021. Annual report of cancer statistics in Korea in 2019. National Cancer Center;Goyang:4. Statistics Korea. 2021. Annual report on the causes of death statistics 2020. Statistics Korea;Daejeon: DOI: 10.1787/a7f257f8-en.5. World Health Organization. 2010. ICD-10: international statistical classification of diseases and related health problems. 10th rev. World Health Organization;Geneva:6. Hong SY, Kang MJ, Kim T, Jung KW, Kim BW. 2022; Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999-2019. Ann Hepatobiliary Pancreat Surg. 26:211–219. DOI: 10.14701/ahbps.22-044. PMID: 35934831.7. National Cancer Institute. 2022. SEER training modules [Internet]. Available from: https://training.seer.cancer.gov/. cited 2022 Apr 17. Bethesda: U.S. National Institutes of Health, National Cancer Institute.8. Kang MJ, Lim J, Han SS, Park HM, Park SJ, Won YJ, et al. 2022; First course of treatment and prognosis of exocrine pancreatic cancer in Korea from 2006 to 2017. Cancer Res Treat. 54:208–217. DOI: 10.4143/crt.2021.421. PMID: 34030432. PMCID: PMC8756130.9. Segi M. 1960. Cancer mortality for selected sites in 24 countries (1950-1957). Sendai: Tohoku University School of Medicine.10. Ederer F, Heise H. 1959. Instructions to IBM 650 programmers in processing survival computations. Vol. 10. Bethesda: National Cancer Institute.11. Centers for Disease Control, Prevention. 2022. United States cancer statistics: incidence and death rates [Internet]. Available from: https://www.cdc.gov/cancer/uscs/technical_notes/stat_methods/rates.htm. cited 2022 May 5. Atlanta: Centers for Disease Control and Prevention.12. National Cancer Institute. Surveillance, epidemiology, and end results program: recent trends in seer age-adjusted incidence rates, 2000-2019 [Internet]. Available from: https://seer.cancer.gov/statistics-network/explorer/application.html?site=40&data_type=1&graph_type=2&compareby=sex&chk_sex_3=3&chk_sex_2=2&rate_type=2&race=1&age_range=1&stage=101&advopt_precision=1&advopt_show_ci=on&advopt_display=2. cited 2022 May 5. Bethesda: National Cancer Institute.13. Kang MJ, Lim JW, Han SS, Park HM, Kim SW, Lee WJ, et al. 2022; Distinct prognosis of biliary tract cancer according to tumor location, stage, and treatment: a population-based study. Sci Rep. 12:10206. DOI: 10.1038/s41598-022-13605-3. PMID: 35715440. PMCID: PMC9205970.14. Walter D, Ferstl P, Waidmann O, Trojan J, Hartmann S, Schnitzbauer AA, et al. 2019; Cholangiocarcinoma in Germany: epidemiologic trends and impact of misclassification. Liver Int. 39:316–323. DOI: 10.1111/liv.13954. PMID: 30176117.15. Khan SA, Emadossadaty S, Ladep NG, Thomas HC, Elliott P, Taylor-Robinson SD, et al. 2012; Rising trends in cholangiocarcinoma: is the ICD classification system misleading us? J Hepatol. 56:848–854. DOI: 10.1016/j.jhep.2011.11.015. PMID: 22173164.16. Kang MJ, Lim J, Han SS, Park HM, Kim SW, Won YJ, et al. 2021; Impact of changes in the topographic classification of Klatskin tumor on incidence of intra- and extrahepatic bile duct cancer: a population-based national cancer registry study. J Hepatobiliary Pancreat Sci. 28:740–750. DOI: 10.1002/jhbp.916. PMID: 33615747.17. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. 2013. International classification of diseases for oncology, 3rd ed, 1st revision [Internet]. Available from: https://apps.who.int/iris/handle/10665/96612. cited 2022 May 19. Geneva: World Health Organization.18. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. 2019. International classification of diseases for oncology, 3rd ed, 2nd revision [Internet]. Available from: http://www.iacr.com.fr/index.php?option=com_content&view=article&id=149:icd-o-3-2&catid=80&itemid=545. cited 2022 May 19. Lyon: IARC.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence and Overall Survival of Biliary Tract Cancers in South Korea from 2006 to 2015: Using the National Health Information Database
- Clinical Review of Carcinomas of the Extrahepatic Bile Ducts and Gallbladders
- Trend Analysis and Prediction of Hepatobiliary Pancreatic Cancer Incidence and Mortality in Korea
- Recurrent pyogenic cholangitis: The pattern of thickening of the extrahepatic bile duct on CT
- Introduction of 7th AJCC Cancer Staging: Gallbladder, Perihilar Bile Duct and Distal Common Bile Duct