Korean Circ J.
2022 Aug;52(8):623-631. 10.4070/kcj.2021.0335.
A Bicentric Propensity Matched Analysis of 158 Patients Comparing Porcine Versus Bovine Stented Bioprosthetic Valves in Pulmonary Position
- Affiliations
-
- 1Congenital Cardiovascular Surgery, Hospital Universitario La Paz, Madrid, Spain
- 2Congenital Cardiovascular Surgery, Hospital Universitario Ramón y Cajal, Madrid, Spain
- 3Instituto de Investigación, Hospital Universitario La Paz, Madrid, Spain
- KMID: 2532333
- DOI: http://doi.org/10.4070/kcj.2021.0335
Abstract
- Background and Objectives
Pulmonary valve replacement (PVR) is the most common operation in adults with congenital heart disease (CHD). There is controversy regarding the best bioprosthesis. We compare the performance of stented bioprosthetic valves (the Mosaic [Medtronic™] porcine pericardial against Carpentier Perimount Magna Ease [Edwards™] bovine) in pulmonary position in patients with CHD.
Methods
Between January 1999 and December 2019, all the PVRs were identified from hospital databases in 2 congenital heart centres in Spain. Valve performance was evaluated using clinical and echocardiographic criteria. Propensity score matching was used to balance the 2 treatment groups.
Results
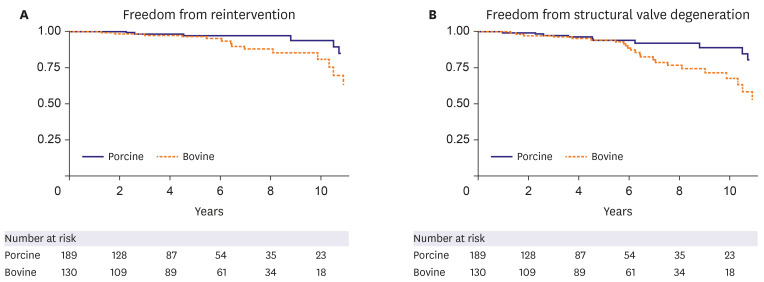
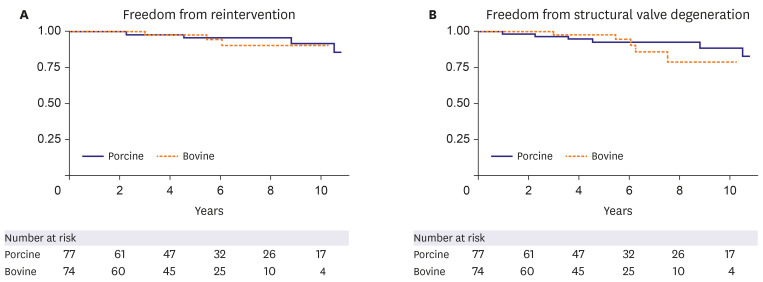
Three hundred nineteen patients were retrospectively identified. After statistical adjustment, 79 propensity-matched pairs were available for comparison Freedom from reintervention for the porcine cohort was 98.3%, 96.1%, and 91.9% at 3, 5, and 10 years and 100%, 98%, and 90.8% for the bovine cohort (p=0.88). Freedom from structural valve degeneration (SVD) for the porcine cohort was 96.9%, 92.8% and 88.7% at 3, 5, and 10 years and 100%, 98%, and 79.1% for the bovine cohort (p=0.38). Bovine prosthesis was associated with a reintervention hazard ratio (HR), 1.12; 95% confidence intervals (CIs), 0.24–5.26; p=0.89 and SVD HR, 1.69 (0.52–5.58); p=0.38. In the first 5 years, there was no difference in outcomes. After 5 years, the recipients of the bovine bioprosthesis were at higher risk for SVD (reintervention HR, 2.08 [0.27–16.0]; p=0.49; SVD HR, 6.99 [1.23–39.8]; p=0.03).
Conclusions
Both bioprosthesis have similar outcomes up to 5 years, afterwards, porcine bioprosthesis seem to have less SVD.
Figure
Cited by 1 articles
-
Beyond the Valve: Lifelong Management of Right Ventricular Outflow Tract Lesion in Adult Congenital Heart Disease
Chang-Ha Lee
Korean Circ J. 2022;52(8):632-634. doi: 10.4070/kcj.2022.0165.
Reference
-
1. Kogon BE, Rosenblum JM, Mori M. Current readings: issues surrounding pulmonary valve replacement in repaired tetralogy of fallot. Semin Thorac Cardiovasc Surg. 2015; 27:57–64. PMID: 26074110.
Article2. Fiore AC, Rodefeld M, Turrentine M, et al. Pulmonary valve replacement: a comparison of three biological valves. Ann Thorac Surg. 2008; 85:1712–1718. PMID: 18442571.
Article3. Emani SM. Options for prosthetic pulmonary valve replacement. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2012; 15:34–37. PMID: 22424506.
Article4. Akins CW, Miller DC, Turina MI, et al. Guidelines for reporting mortality and morbidity after cardiac valve interventions. J Thorac Cardiovasc Surg. 2008; 135:732–738. PMID: 18374749.
Article5. Bermudez CA, Dearani JA, Puga FJ, et al. Late results of the peel operation for replacement of failing extracardiac conduits. Ann Thorac Surg. 2004; 77:881–887. PMID: 14992892.
Article6. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014; 49:1701–1720. PMID: 24779867.
Article7. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014; 33:1242–1258. PMID: 24122911.
Article8. Koziarz A, Makhdoum A, Butany J, Ouzounian M, Chung J. Modes of bioprosthetic valve failure: a narrative review. Curr Opin Cardiol. 2020; 35:123–132. PMID: 31972604.
Article9. Kostyunin AE, Yuzhalin AE, Rezvova MA, Ovcharenko EA, Glushkova TV, Kutikhin AG. Degeneration of bioprosthetic heart valves: update 2020. J Am Heart Assoc. 2020; 9:e018506. PMID: 32954917.
Article10. Salaun E, Mahjoub H, Girerd N, et al. Rate, timing, correlates, and outcomes of hemodynamic valve deterioration after bioprosthetic surgical aortic valve replacement. Circulation. 2018; 138:971–985. PMID: 30354532.
Article11. Barakat A, Mittal A, Ricketts D, Rogers BA. Understanding survival analysis: actuarial life tables and the Kaplan-Meier plot. Br J Hosp Med (Lond). 2019; 80:642–646. PMID: 31707885.
Article12. Cuerpo Caballero G, López Menéndez J, Polo López L, et al. Cirugía cardiovascular en España en el año 2019. Registro de intervenciones de la Sociedad Española de Cirugía Cardiovascular y Endovascular. Cirugía Cardiovasc. 2021; 28:162–176.
Article13. Raghav V, Okafor I, Quach M, Dang L, Marquez S, Yoganathan AP. Long-term durability of Carpentier-Edwards magna ease valve: a one billion cycle in vitro study. Ann Thorac Surg. 2016; 101:1759–1765. PMID: 26806168.
Article14. Forcillo J, Pellerin M, Perrault LP, et al. Carpentier-Edwards pericardial valve in the aortic position: 25-years experience. Ann Thorac Surg. 2013; 96:486–493. PMID: 23684486.
Article15. Pragt H, van Melle JP, Verkerke GJ, Mariani MA, Ebels T. Pulmonary versus aortic pressure behavior of a bovine pericardial valve. J Thorac Cardiovasc Surg. 2020; 159:1051–1059.e1. PMID: 31383558.
Article16. Kwak JG, Bang JH, Cho S, et al. Long-term durability of bioprosthetic valves in pulmonary position: pericardial versus porcine valves. J Thorac Cardiovasc Surg. 2020; 160:476–484. PMID: 32014323.
Article17. Pragt H, Schoots MH, Accord RE, et al. A stented bovine pericardial prosthesis in the pulmonary position. J Thorac Cardiovasc Surg. 2020; 159:1063–1071.e1. PMID: 31400815.
Article18. Abbas JR, Hoschtitzky JA. Which is the best tissue valve used in the pulmonary position, late after previous repair of tetralogy of fallot? Interact Cardiovasc Thorac Surg. 2013; 17:854–860. PMID: 23929900.
Article19. Dorobantu DM, Sharabiani MT, Taliotis D, et al. Age over 35 years is associated with increased mortality after pulmonary valve replacement in repaired tetralogy of Fallot: results from the UK National Congenital Heart Disease Audit database. Eur J Cardiothorac Surg. 2020; 58:825–831. PMID: 32187367.
Article20. Aroca Á, Polo L, Pérez-Farinós N, et al. ¿Funcionan igual las prótesis pulmonares porcinas en menores de edad que en adultos? Una llamada a la prudencia. Cirugía Cardiovasc. 2017; 24:135–141.
Article21. Marathe SP, Bell D, Betts K, et al. Homografts versus stentless bioprosthetic valves in the pulmonary position: a multicentre propensity-matched comparison in patients younger than 20 years. Eur J Cardiothorac Surg. 2019; 2019:1–8.
Article22. Tatewaki H, Shiose A. Pulmonary valve replacement after repaired tetralogy of fallot. Gen Thorac Cardiovasc Surg. 2018; 66:509–515. PMID: 29779123.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bioprosthesis in the Mitral Position: Bovine Pericardial versus Porcine Xenograft
- Pericardial Versus Porcine Valves for Surgical Aortic Valve Replacement
- Biaxial Strain Analysis of Various Fixation Models in Porcine Aortic and Pulmonary Valves
- Measurement of Porcine Aortic and Pulmonary Valve Geometry and Design for Implantable Tissue Valve
- Comparison of the Uniaxial Tensile Strength, Elasticity and Thermal Stability between Glutaraldehyde and Glutaraldehyde with Solvent Fixation in Xenograft Cardiovascular Tissue