J Korean Med Sci.
2022 Aug;37(32):e250. 10.3346/jkms.2022.37.e250.
The Higher Incidence of COVID-19 in Patients With Non-Tuberculous Mycobacterial Pulmonary Disease: A Single Center Experience in Korea
- Affiliations
-
- 1Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2532324
- DOI: http://doi.org/10.3346/jkms.2022.37.e250
Abstract
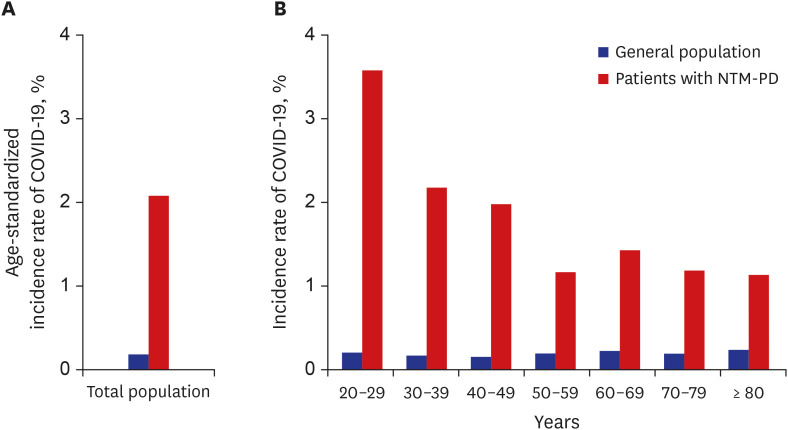
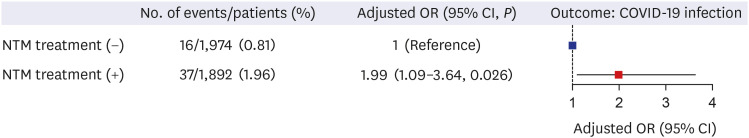
- The aim of our study was to investigate the incidence of and risk factors for coronavirus disease 2019 (COVID-19) in patients with non-tuberculous mycobacterial-pulmonary disease (NTM-PD). A total of 3,866 patients with NTM-PD were retrospectively identified from a single center. Compared to the general population of Korea, patients with NTM-PD had a substantially increased age-standardized incidence of COVID-19 from January 2020 to February 2021 (2.1% vs. 0.2%). The odds of being infected with COVID-19 was particularly higher in patients who received treatment for NTM-PD than in those who did not receive treatment for NTM-PD (adjusted odd ratio = 1.99, 95% confidence interval = 1.09–3.64, P = 0.026). Patients with NTM-PD might be regarded as a high-risk group for COVID-19 and may need a more proactive preventive strategy for COVID-19 and other pandemics in the future.
Keyword
Figure
Reference
-
1. Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015; 36(1):13–34. PMID: 25676516.
Article2. Jeon D. Infection source and epidemiology of nontuberculous mycobacterial lung disease. Tuberc Respir Dis (Seoul). 2019; 82(2):94–101. PMID: 30302953.
Article3. Floto RA, Olivier KN, Saiman L, Daley CL, Herrmann JL, Nick JA, et al. US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax. 2016; 71(Suppl 1):i1–22. PMID: 26666259.
Article4. Kartalija M, Ovrutsky AR, Bryan CL, Pott GB, Fantuzzi G, Thomas J, et al. Patients with nontuberculous mycobacterial lung disease exhibit unique body and immune phenotypes. Am J Respir Crit Care Med. 2013; 187(2):197–205. PMID: 23144328.
Article5. Marras TK, Campitelli MA, Kwong JC, Lu H, Brode SK, Marchand-Austin A, et al. Risk of nontuberculous mycobacterial pulmonary disease with obstructive lung disease. Eur Respir J. 2016; 48(3):928–931. PMID: 27288038.
Article6. Phoompoung P, Chayakulkeeree M. Chronic pulmonary aspergillosis following nontuberculous mycobacterial infections: an emerging disease. J Fungi (Basel). 2020; 6(4):E346. PMID: 33302348.
Article7. Jhun BW, Jung WJ, Hwang NY, Park HY, Jeon K, Kang ES, et al. Risk factors for the development of chronic pulmonary aspergillosis in patients with nontuberculous mycobacterial lung disease. PLoS One. 2017; 12(11):e0188716. PMID: 29190796.
Article8. Zhang X. Epidemiology of Covid-19. N Engl J Med. 2020; 382(19):1869–1870.
Article9. Jia Z, Gong W. Will mutations in the spike protein of SARS-CoV-2 lead to the failure of COVID-19 vaccines? J Korean Med Sci. 2021; 36(18):e124. PMID: 33975397.
Article10. Koh WJ. Nontuberculous mycobacteria-overview. Microbiol Spectr. 2017; 5(1):5.1.11.
Article11. Lee H, Park HJ, Cho SN, Bai GH, Kim SJ. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of the rpoB gene. J Clin Microbiol. 2000; 38(8):2966–2971. PMID: 10921960.
Article12. Kwon YS, Koh WJ, Daley CL. Treatment of Mycobacterium avium complex pulmonary disease. Tuberc Respir Dis (Seoul). 2019; 82(1):15–26. PMID: 30574687.13. Fang M, Wang D, Tang O, Selvin E. Prevalence of chronic disease in laboratory-confirmed COVID-19 cases and U.S. adults (2017–2018). Diabetes Care. 2020; 43(10):e127–e128. PMID: 32796010.
Article14. Jeong GH, Lee HJ, Lee J, Lee JY, Lee KH, Han YJ, et al. Effective control of COVID-19 in South Korea: cross-sectional study of epidemiological data. J Med Internet Res. 2020; 22(12):e22103. PMID: 33151893.
Article15. Bui LT, Winters NI, Chung MI, Joseph C, Gutierrez AJ, Habermann AC, et al. Chronic lung diseases are associated with gene expression programs favoring SARS-CoV-2 entry and severity. Nat Commun. 2021; 12(1):4314. PMID: 34262047.
Article16. Lee SC, Son KJ, Han CH, Park SC, Jung JY. Impact of COPD on COVID-19 prognosis: a nationwide population-based study in South Korea. Sci Rep. 2021; 11(1):3735. PMID: 33580190.
Article17. Banerjee A, Pasea L, Harris S, Gonzalez-Izquierdo A, Torralbo A, Shallcross L, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020; 395(10238):1715–1725. PMID: 32405103.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Contusion Similar to COVID-19 Pneumonia
- Post–Coronavirus Disease 2019 Pulmonary Fibrosis: Wait or Needs Intervention
- Vaccination Rates of Hospitalized Patients at High Risk of Severe COVID-19: A Single-Center CrossSectional Study
- New-Onset Seizures in Patients With COVID-19: A Case Series From a Single Public Hospital in Korea
- Coronavirus Disease 2019-Associated Pulmonary Aspergillosis