J Korean Med Sci.
2022 Aug;37(31):e243. 10.3346/jkms.2022.37.e243.
The Effect of Chronic Disease Management Program on the Risk of Complications in Patients With Hypertension in Korea
- Affiliations
-
- 1BigData Strategy Department, National Health Insurance Service, Wonju, Korea
- 2HIRA Research Institute, Health Insurance Review and Assessment Service, Wonju, Korea
- 3Department of Public Health, Graduate School, College of Medicine, Yonsei University, Seoul, Korea
- 4Division of Cancer Control & Policy, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 5Division of Endocrinology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 6Department of Research and Analysis, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2532318
- DOI: http://doi.org/10.3346/jkms.2022.37.e243
Abstract
- Background
A chronic disease management program was implemented in April 2012 to lower out-of-pocket costs for repeat visits to the same clinic. The aim of this study was to investigate the association between participating in this program and the onset of complications among patients with hypertension using whole-nation claims data.
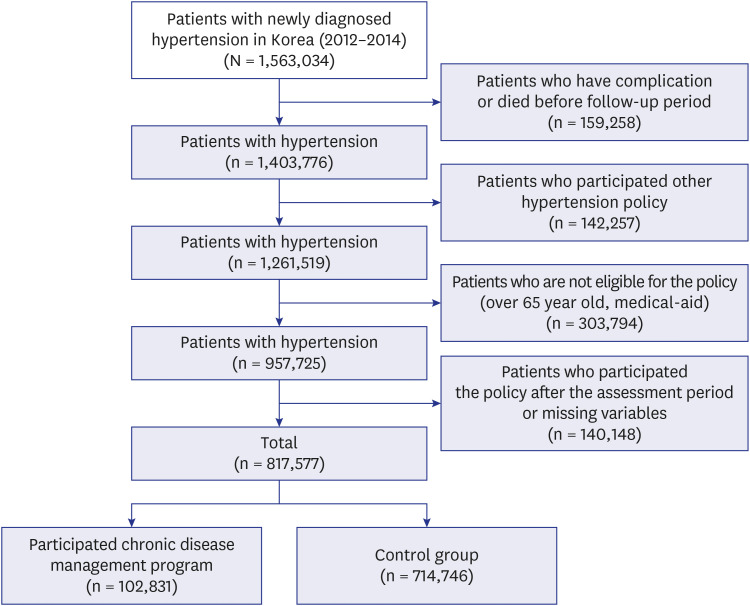
Methods
We used National Health Insurance Service data (2011–2018) and patients with newly detected hypertension from 2012 to 2014 were selected. Chronic disease management program reduces the out-of-pocket expenses of consultation fee from 30% to 20% when patients enroll in this program by agreeing to visit the same clinic for the treatment of hypertension or diabetes. As the dependent variable, acute myocardial infarction (MI), stroke, chronic kidney disease (CKD), and heart failure (HF) were selected. For analysis, cox proportional hazards model was used.
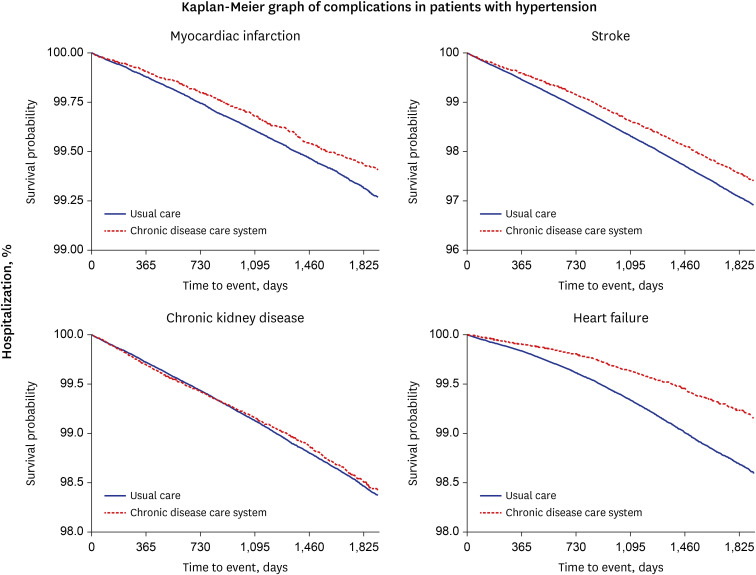
Results
Total participants were 827,577, among which 102,831(12.6%) subjects participated in the chronic disease management. Participants of the chronic disease management program were more likely to show lower hazard ratios (HRs) than those of non-participants in terms of all complications (MI: HR, 0.75; 95% confidence interval [CI], 0.68–0.82; stroke: HR, 0.75; 95% CI, 0.72–0.78; CKD: HR, 0.90; 95% CI, 0.85–0.96; HF: HR, 0.56; 95% CI, 0.52–0.61).
Conclusion
The results showed that participants of the chronic disease management program were less likely to have hypertension complications compared to non-participants. Enhancing the participation rate may be related to better outcomes and reducing medical expenses among patients with chronic diseases.
Keyword
Figure
Reference
-
1. Kim HC, Cho MC. Korean Society Hypertension (KSH). Hypertension Epidemiology Research Working Group. Korea hypertension fact sheet 2018. Clin Hypertens. 2018; 24(1):13. PMID: 30288297.
Article2. World Health Organization. Hypertension. Accessed November 10, 2020. https://www.who.int/health-topics/hypertension/#tab=tab_1 .3. Victor RG, Kaplan NM. Kaplan’s Clinical Hypertension. 10th ed. Philadelphia, PA, USA: Lippincott Williams & Wilkins;2010.4. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006; 367(9524):1747–1757. PMID: 16731270.
Article5. van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010; 16(5):947–956. PMID: 20553366.
Article6. Gill JM, Mainous AG 3rd, Diamond JJ, Lenhard MJ. Impact of provider continuity on quality of care for persons with diabetes mellitus. Ann Fam Med. 2003; 1(3):162–170. PMID: 15043378.
Article7. O’Connor PJ, Desai J, Rush WA, Cherney LM, Solberg LI, Bishop DB. Is having a regular provider of diabetes care related to intensity of care and glycemic control? J Fam Pract. 1998; 47(4):290–297. PMID: 9789515.8. Park YH. Strategy for noncommunicable disease control and prevention. J Korean Med Assoc. 2014; 57(10):808–814.
Article9. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800. PMID: 27794523.
Article10. Dubow J, Fink ME. Impact of hypertension on stroke. Curr Atheroscler Rep. 2011; 13(4):298–305. PMID: 21626308.
Article11. Ghaderian SB, Beladi-Mousavi SS. The role of diabetes mellitus and hypertension in chronic kidney disease. J Renal Inj Prev. 2014; 3(4):109–110. PMID: 25610891.12. Messerli FH, Rimoldi SF, Bangalore S. The transition from hypertension to heart failure: contemporary update. JACC Heart Fail. 2017; 5(8):543–551. PMID: 28711447.13. Rakugi H, Yu H, Kamitani A, Nakamura Y, Ohishi M, Kamide K, et al. Links between hypertension and myocardial infarction. Am Heart J. 1996; 132(1 Pt 2 Su):213–221. PMID: 8677859.
Article14. Kim W, Choy YS, Lee SA, Park EC. Implementation of the chronic disease care system and its association with health care costs and continuity of care in Korean adults with type 2 diabetes mellitus. BMC Health Serv Res. 2018; 18(1):991. PMID: 30577787.15. Back J, Lee S, Kuark TS, Ghang HY, Yun YD. Analysis of the Effectiveness of Medical Use of Health Support Services Through Chronic Disease Management System. Seoul, Korea: Health Insurance Policy Research Institute, National Health Insurance Service;2015.16. Rijken M, Bekkema N, Boeckxstaens P, Schellevis FG, De Maeseneer JM, Groenewegen PP. Chronic disease management programmes: an adequate response to patients’ needs? Health Expect. 2014; 17(5):608–621. PMID: 22712877.
Article17. Liu LS. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi. 2011; 39(7):579–615. PMID: 22088239.18. Kim JA, Lee EK. Effect of the clinic-based chronic disease management program on the appropriateness of medication adherence and persistence in hypertension patients in Korea. Pharm Soc Korea. 2017; 61(3):135–146.
Article19. Chen CC, Chen SH. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011; 17(6):420–427. PMID: 21756012.20. Oh IH. Health management service system and clinic-level chronic disease management system. Med Policy Forum. 2012; 10(4):21–27.21. Kim KH, Lee JC, Kim HN. A study on institutional improvement measures for re-establishing the function of medical institutions. Nat Policy Res. 2011; 25(4):161–178.22. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998–2005. Diabetes Care. 2009; 32(11):2016–2020. PMID: 19675201.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors Management in Diabetic Patients
- Preoperative management of chronic disease
- Evaluation of Oral Health Promotion Program Connected with Hypertension and Diabetes Management Programs: Use of a Logical Model
- Impact of a Primary Health Care Chronic Diseases Management Pilot Program
- Management of Hypertension in Diabetic Patients