Brain Tumor Res Treat.
2022 Jul;10(3):164-171. 10.14791/btrt.2022.0023.
Recent Update on Neurosurgical Management of Brain Metastasis
- Affiliations
-
- 1Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2532249
- DOI: http://doi.org/10.14791/btrt.2022.0023
Abstract
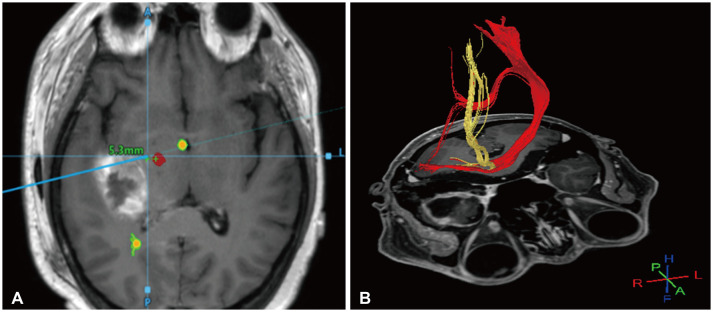
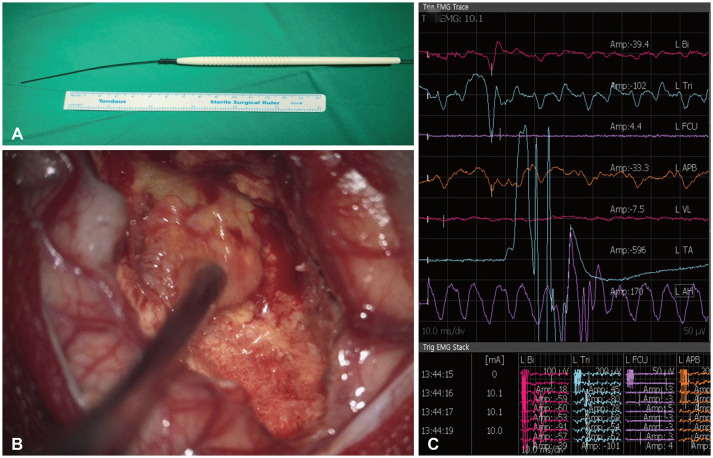
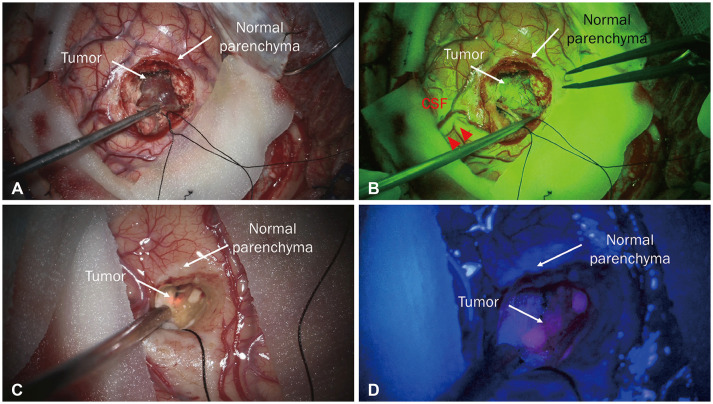
- Brain metastasis (BM), classified as a secondary brain tumor, is the most common malignant central nervous system tumor whose median overall survival is approximately 6 months. However, the survival rate of patients with BMs has increased with recent advancements in immunotherapy and targeted therapy. This means that clinicians should take a more active position in the treatment paradigm that passively treats BMs. Because patients with BM are treated in a variety of clinical settings, treatment planning requires a more sophisticated decision-making process than that for other primary malignancies. Therefore, an accurate prognostic prediction is essential, for which a graded prognostic assessment that reflects next-generation sequencing can be helpful. It is also essential to understand the indications for various treatment modalities, such as surgical resection, stereotactic radiosurgery, and whole-brain radiotherapy and consider their advantages and disadvantages when choosing a treatment plan. Surgical resection serves a limited auxiliary function in BM, but it can be an essential therapeutic approach for increasing the survival rate of specific patients; therefore, this must be thoroughly recognized during the treatment process. The ultimate goal of surgical resection is maximal safe resection; to this end, neuronavigation, intraoperative neuro-electrophysiologic assessment including evoked potential, and the use of fluorescent materials could be helpful. In this review, we summarize the considerations for neurosurgical treatment in a rapidly changing treatment environment.
Keyword
Figure
Reference
-
1. Artzi M, Bressler I, Ben Bashat D. Differentiation between glioblastoma, brain metastasis and subtypes using radiomics analysis. J Magn Reson Imaging. 2019; 50:519–528. PMID: 30635952.2. Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012; 14:48–54. PMID: 22012633.3. Stelzer KJ. Epidemiology and prognosis of brain metastases. Surg Neurol Int. 2013; 4(Suppl 4):S192–S202. PMID: 23717790.4. Fecci PE, Champion CD, Hoj J, McKernan CM, Goodwin CR, Kirkpatrick JP, et al. The evolving modern management of brain metastasis. Clin Cancer Res. 2019; 25:6570–6580. PMID: 31213459.5. Suh JH. Stereotactic radiosurgery for the management of brain metastases. N Engl J Med. 2010; 362:1119–1127. PMID: 20335588.6. Bindal RK, Sawaya R, Leavens ME, Lee JJ. Surgical treatment of multiple brain metastases. J Neurosurg. 1993; 79:210–216. PMID: 8331402.7. Walker AE, Robins M, Weinfeld FD. Epidemiology of brain tumors: the national survey of intracranial neoplasms. Neurology. 1985; 35:219–226. PMID: 3969210.8. Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990; 322:494–500. PMID: 2405271.9. Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. 2012; 30:419–425. PMID: 22203767.10. Narita Y, Sato S, Kayama T. Review of the diagnosis and treatment of brain metastases. Jpn J Clin Oncol. 2022; 52:3–7. PMID: 34865060.11. Valiente M, Ahluwalia MS, Boire A, Brastianos PK, Goldberg SB, Lee EQ, et al. The evolving landscape of brain metastasis. Trends Cancer. 2018; 4:176–196. PMID: 29506669.12. Hatiboglu MA, Akdur K, Sawaya R. Neurosurgical management of patients with brain metastasis. Neurosurg Rev. 2020; 43:483–495. PMID: 30058049.13. Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys. 1997; 37:745–751. PMID: 9128946.14. Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, et al. Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys. 2012; 82:2111–2117. PMID: 21497451.15. Sperduto PW, Yang TJ, Beal K, Pan H, Brown PD, Bangdiwala A, et al. Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (Lung-molGPA). JAMA Oncol. 2017; 3:827–831. PMID: 27892978.16. Sperduto PW, Jiang W, Brown PD, Braunstein S, Sneed P, Wattson DA, et al. Estimating survival in melanoma patients with brain metastases: an update of the graded prognostic assessment for melanoma using molecular markers (Melanoma-molGPA). Int J Radiat Oncol Biol Phys. 2017; 99:812–816. PMID: 29063850.17. Sperduto PW, Deegan BJ, Li J, Jethwa KR, Brown PD, Lockney N, et al. Estimating survival for renal cell carcinoma patients with brain metastases: an update of the Renal Graded Prognostic Assessment tool. Neuro Oncol. 2018; 20:1652–1660. PMID: 30418657.18. Sperduto PW, Fang P, Li J, Breen W, Brown PD, Cagney D, et al. Estimating survival in patients with gastrointestinal cancers and brain metastases: an update of the graded prognostic assessment for gastrointestinal cancers (GI-GPA). Clin Transl Radiat Oncol. 2019; 18:39–45. PMID: 31341974.19. To KKW, Fong W, Cho WCS. Immunotherapy in treating EGFR-mutant lung cancer: current challenges and new strategies. Front Oncol. 2021; 11:635007. PMID: 34113560.20. Dimitriou F, Long GV, Menzies AM. Novel adjuvant options for cutaneous melanoma. Ann Oncol. 2021; 32:854–865. PMID: 33771664.21. Carapella CM, Gorgoglione N, Oppido PA. The role of surgical resection in patients with brain metastases. Curr Opin Oncol. 2018; 30:390–395. PMID: 30142093.22. Hatiboglu MA, Chang EL, Suki D, Sawaya R, Wildrick DM, Weinberg JS. Outcomes and prognostic factors for patients with brainstem metastases undergoing stereotactic radiosurgery. Neurosurgery. 2011; 69:796–806. PMID: 21508879.23. Li B, Yu J, Suntharalingam M, Kennedy AS, Amin PP, Chen Z, et al. Comparison of three treatment options for single brain metastasis from lung cancer. Int J Cancer. 2000; 90:37–45. PMID: 10725856.24. Crossen JR, Garwood D, Glatstein E, Neuwelt EA. Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy. J Clin Oncol. 1994; 12:627–642. PMID: 8120563.25. Meyers CA, Brown PD. Role and relevance of neurocognitive assessment in clinical trials of patients with CNS tumors. J Clin Oncol. 2006; 24:1305–1309. PMID: 16525186.26. Tallet AV, Azria D, Barlesi F, Spano JP, Carpentier AF, Gonçalves A, et al. Neurocognitive function impairment after whole brain radiotherapy for brain metastases: actual assessment. Radiat Oncol. 2012; 7:77. PMID: 22640600.27. Gondi V, Deshmukh S, Brown PD, Wefel JS, Tome W, Armstrong T, et al. NRG Oncology CC001: A phase III trial of hippocampal avoidance (HA) in addition to whole-brain radiotherapy (WBRT) plus memantine to preserve neurocognitive function (NCF) in patients with brain metastases (BM) [abstract]. J Clin Oncol. 2019; 37(15 Suppl):2009.28. Brown PD, Gondi V, Pugh S, Tome WA, Wefel JS, Armstrong TS, et al. Hippocampal avoidance during whole-brain radiotherapy plus memantine for patients with brain metastases: phase III trial NRG oncology CC001. J Clin Oncol. 2020; 38:1019–1029. PMID: 32058845.29. Costabile JD, Alaswad E, D’Souza S, Thompson JA, Ormond DR. Current applications of diffusion tensor imaging and tractography in intracranial tumor resection. Front Oncol. 2019; 9:426. PMID: 31192130.30. Hervey-Jumper SL, Berger MS. Insular glioma surgery: an evolution of thought and practice. J Neurosurg. 2019; 130:9–16. PMID: 30611160.31. Nimsky C, Ganslandt O, Hastreiter P, Fahlbusch R. Intraoperative compensation for brain shift. Surg Neurol. 2001; 56:357–364. discussion 364-5. PMID: 11755962.32. Catapano G, Sgulò FG, Acurio Padilla PE, Spennato P, Di Nuzzo G, Boniello V, et al. Palatal position of patient tracker for magnetic neuronavigation system: technical note. World Neurosurg. 2018; 116:105–109. PMID: 29753080.33. Krieg SM, Schäffner M, Shiban E, Droese D, Obermüller T, Gempt J, et al. Reliability of intraoperative neurophysiological monitoring using motor evoked potentials during resection of metastases in motor-eloquent brain regions: clinical article. J Neurosurg. 2013; 118:1269–1278. PMID: 23521547.34. Zuo F, Hu K, Kong J, Zhang Y, Wan J. Surgical management of brain metastases in the perirolandic region. Front Oncol. 2020; 10:572644. PMID: 33194673.35. Gutzwiller EM, Cabrilo I, Radovanovic I, Schaller K, Boëx C. Intraoperative monitoring with visual evoked potentials for brain surgeries. J Neurosurg. 2019; 130:654–660.36. Zileli M, Idiman F, Hiçdönmez T, Ovül I, Tunçbay E. A comparative study of brain-stem auditory evoked potentials and blink reflexes in posterior fossa tumor patients. J Neurosurg. 1988; 69:660–668. PMID: 3183728.37. Sayyahmelli S, Aydin I, Wheeler B, Baskaya MK. Mapping of the internal capsule with subcortical stimulation for gross-total resection of a thalamic metastatic tumor. Neurosurg Focus. 2018; 45(VideoSuppl2):V7. PMID: 30269558.38. Han SJ, Morshed RA, Troncon I, Jordan KM, Henry RG, Hervey-Jumper SL, et al. Subcortical stimulation mapping of descending motor pathways for perirolandic gliomas: assessment of morbidity and functional outcome in 702 cases. J Neurosurg. 2018; 131:201–208. PMID: 30117770.39. Duffau H, Peggy Gatignol ST, Mandonnet E, Capelle L, Taillandier L. Intraoperative subcortical stimulation mapping of language pathways in a consecutive series of 115 patients with Grade II glioma in the left dominant hemisphere. J Neurosurg. 2008; 109:461–471. PMID: 18759577.40. Duffau H. Intraoperative direct subcortical stimulation for identification of the internal capsule, combined with an image-guided stereotactic system during surgery for basal ganglia lesions. Surg Neurol. 2000; 53:250–254. PMID: 10773257.41. Raabe A, Beck J, Schucht P, Seidel K. Continuous dynamic mapping of the corticospinal tract during surgery of motor eloquent brain tumors: evaluation of a new method. J Neurosurg. 2014; 120:1015–1024. PMID: 24628613.42. Yingling CD, Ojemann S, Dodson B, Harrington MJ, Berger MS. Identification of motor pathways during tumor surgery facilitated by multichannel electromyographic recording. J Neurosurg. 1999; 91:922–927. PMID: 10584836.43. Nossek E, Korn A, Shahar T, Kanner AA, Yaffe H, Marcovici D, et al. Intraoperative mapping and monitoring of the corticospinal tracts with neurophysiological assessment and 3-dimensional ultrasonography-based navigation. J Neurosurg. 2011; 114:738–746. PMID: 20799862.44. Shiban E, Krieg SM, Haller B, Buchmann N, Obermueller T, Boeckh-Behrens T, et al. Intraoperative subcortical motor evoked potential stimulation: how close is the corticospinal tract? J Neurosurg. 2015; 123:711–720. PMID: 26047412.45. Okuda T, Kataoka K, Yabuuchi T, Yugami H, Kato A. Fluorescence-guided surgery of metastatic brain tumors using fluorescein sodium. J Clin Neurosci. 2010; 17:118–121. PMID: 19969462.46. Hamamcıoğlu MK, Akçakaya MO, Göker B, Kasımcan MÖ, Kırış T. The use of the YELLOW 560 nm surgical microscope filter for sodium fluorescein-guided resection of brain tumors: our preliminary results in a series of 28 patients. Clin Neurol Neurosurg. 2016; 143:39–45. PMID: 26895208.47. Marhold F, Mercea PA, Scheichel F, Berghoff AS, Heicappell P, Kiesel B, et al. Detailed analysis of 5-aminolevulinic acid induced fluorescence in different brain metastases at two specialized neurosurgical centers: experience in 157 cases. J Neurosurg. 2020; 133:1032–1043.48. Kamp MA, Grosser P, Felsberg J, Slotty PJ, Steiger HJ, Reifenberger G, et al. 5-Aminolevulinic acid (5-ALA)-induced fluorescence in intracerebral metastases: a retrospective study. Acta Neurochir (Wien). 2012; 154:223–228. PMID: 22080159.49. Baumert BG, Rutten I, Dehing-Oberije C, Twijnstra A, Dirx MJ, Debougnoux-Huppertz RM, et al. A pathology-based substrate for target definition in radiosurgery of brain metastases. Int J Radiat Oncol Biol Phys. 2006; 66:187–194. PMID: 16814946.50. Neves S, Mazal PR, Wanschitz J, Rudnay AC, Drlicek M, Czech T, et al. Pseudogliomatous growth pattern of anaplastic small cell carcinomas metastatic to the brain. Clin Neuropathol. 2001; 20:38–42. PMID: 11220694.51. Yoo H, Kim YZ, Nam BH, Shin SH, Yang HS, Lee JS, et al. Reduced local recurrence of a single brain metastasis through microscopic total resection. J Neurosurg. 2009; 110:730–736. PMID: 19072310.52. Kamp MA, Dibué M, Niemann L, Reichelt DC, Felsberg J, Steiger HJ, et al. Proof of principle: supramarginal resection of cerebral metastases in eloquent brain areas. Acta Neurochir (Wien). 2012; 154:1981–1986. PMID: 22875595.53. Patel P, Patel NV, Danish SF. Intracranial MR-guided laser-induced thermal therapy: single-center experience with the Visualase thermal therapy system. J Neurosurg. 2016; 125:853–860. PMID: 26722845.54. Kamath AA, Friedman DD, Hacker CD, Smyth MD, Limbrick DD Jr, Kim AH, et al. MRI-guided interstitial laser ablation for intracranial lesions: a large single-institution experience of 133 cases. Stereotact Funct Neurosurg. 2017; 95:417–428. PMID: 29339639.55. Missios S, Bekelis K, Barnett GH. Renaissance of laser interstitial thermal ablation. Neurosurg Focus. 2015; 38:E13.56. Asher AL, Burri SH, Wiggins WF, Kelly RP, Boltes MO, Mehrlich M, et al. A new treatment paradigm: neoadjuvant radiosurgery before surgical resection of brain metastases with analysis of local tumor recurrence. Int J Radiat Oncol Biol Phys. 2014; 88:899–906. PMID: 24606851.