Korean J Orthod.
2022 Jul;52(4):268-277. 10.4041/kjod21.255.
Predicting patient experience of Invisalign treatment: An analysis using artificial neural network
- Affiliations
-
- 1Department of Orthodontics, State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, China
- 2Discipline of Orthodontics, Department of Oral Sciences, Sir John Walsh Research Institute, Faculty of Dentistry, University of Otago, Dunedin, New Zealand
- 3Department of Electronic Engineering, Tsinghua University, Beijing, China
- KMID: 2532105
- DOI: http://doi.org/10.4041/kjod21.255
Abstract
Objective
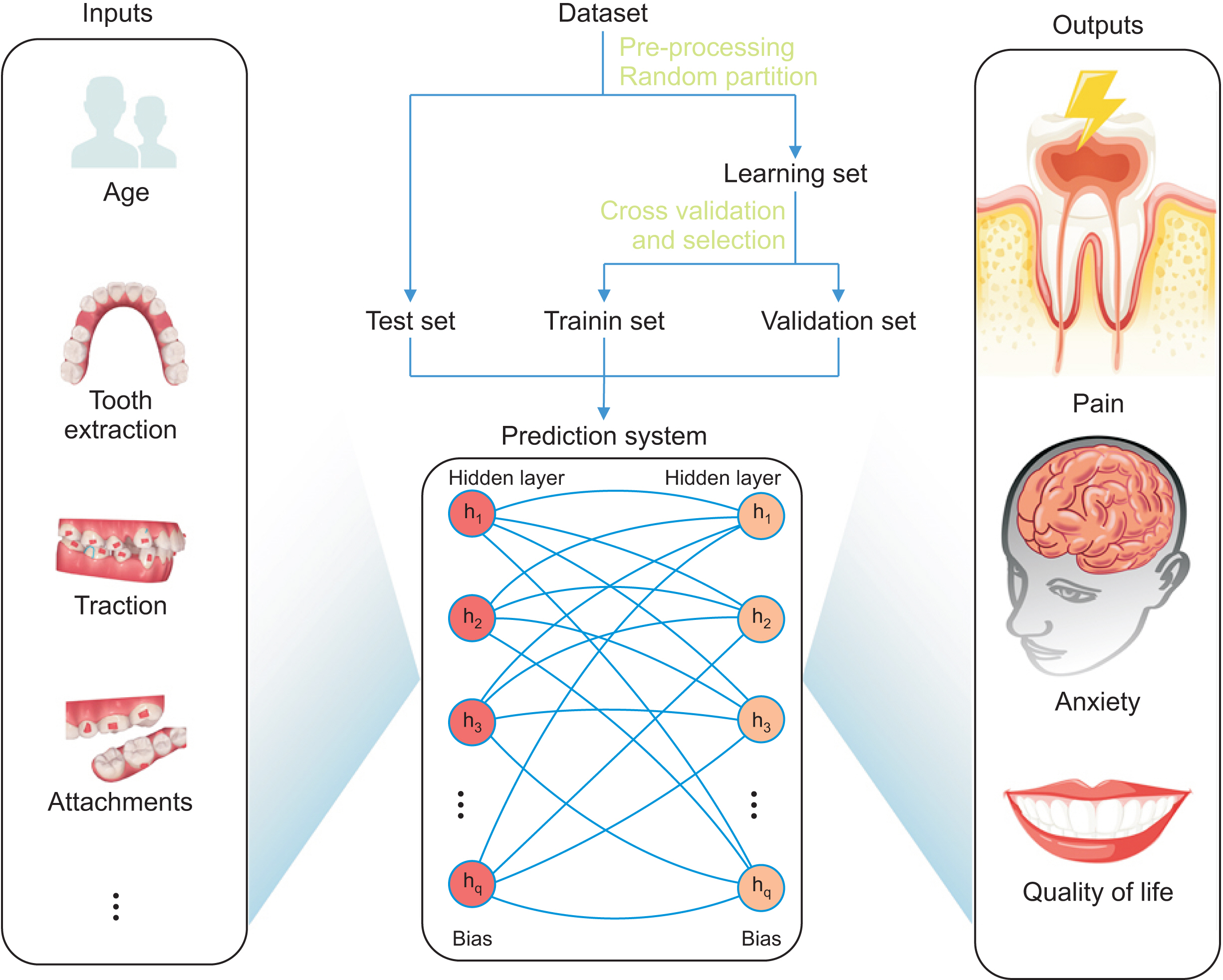
Poor experience with Invisalign treatment affects patient compliance and, thus, treatment outcome. Knowing the potential discomfort level in advance can help orthodontists better prepare the patient to overcome the difficult stage. This study aimed to construct artificial neural networks (ANNs) to predict patient experience in the early stages of Invisalign treatment.
Methods
In total, 196 patients were enrolled. Data collection included questionnaires on pain, anxiety, and quality of life (QoL). A four-layer fully connected multilayer perception with three backpropagations was constructed to predict patient experience of the treatment. The input data comprised 17 clinical features. The partial derivative method was used to calculate the relative contributions of each input in the ANNs.
Results
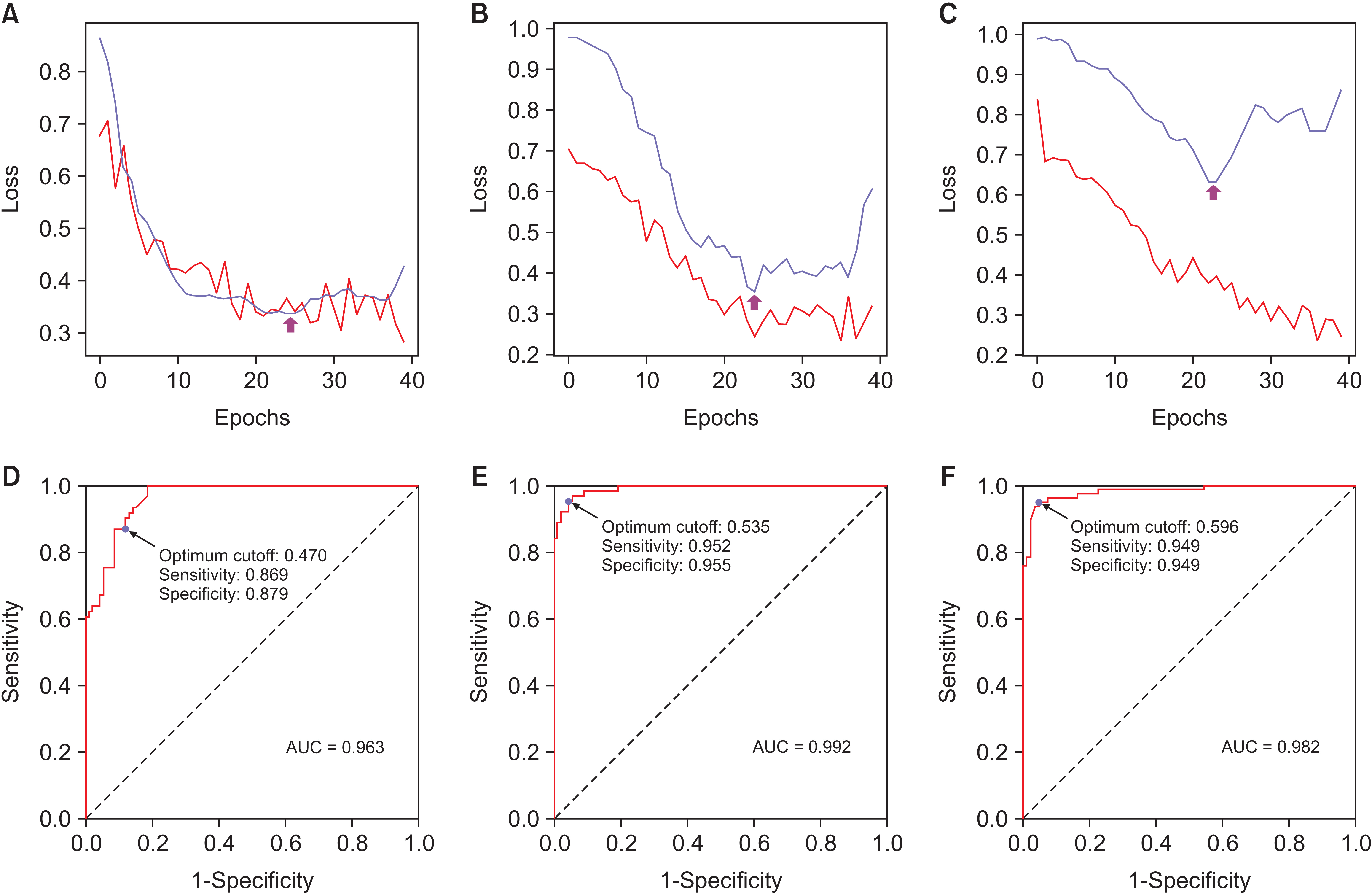
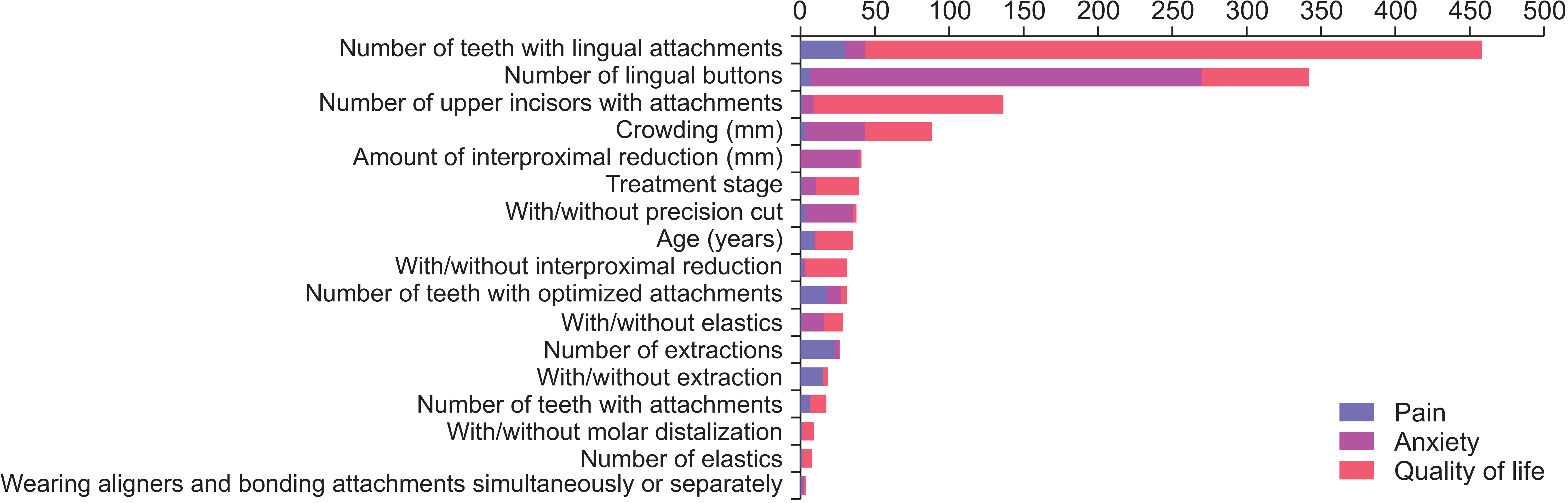
The predictive success rates for pain, anxiety, and QoL were 87.7%, 93.4%, and 92.4%, respectively. ANNs for predicting pain, anxiety, and QoL yielded areas under the curve of 0.963, 0.992, and 0.982, respectively. The number of teeth with lingual attachments was the most important factor affecting the outcome of negative experience, followed by the number of lingual buttons and upper incisors with attachments.
Conclusions
The constructed ANNs in this preliminary study show good accuracy in predicting patient experience (i.e., pain, anxiety, and QoL) of Invisalign treatment. Artificial intelligence system developed for predicting patient comfort has potential for clinical application to enhance patient compliance.
Keyword
Figure
Reference
-
1. Schwendicke F, Samek W, Krois J. 2020; Artificial intelligence in dentistry: chances and challenges. J Dent Res. 99:769–74. DOI: 10.1177/0022034520915714. PMID: 32315260. PMCID: PMC7309354. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85084049434&origin=inward.2. Shahmoradi L, Safdari R, Mirhosseini MM, Arji G, Jannat B, Abdar M. 2018; Predicting risk of acute appendicitis: a comparison of artificial neural network and logistic regression models predicting risk of acute appendicitis: a comparison of artificial neural network and logistic regression models. Acta Med Iran. 56:784–95.3. Kök H, Acilar AM, İzgi MS. 2019; Usage and comparison of artificial intelligence algorithms for determination of growth and development by cervical vertebrae stages in orthodontics. Prog Orthod. 20:41. DOI: 10.1186/s40510-019-0295-8. PMID: 31728776. PMCID: PMC6856254. PMID: 9e00597c2a594eeeac0d562615036f6b. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85075037534&origin=inward.4. Wang H, Minnema J, Batenburg KJ, Forouzanfar T, Hu FJ, Wu G. 2021; Multiclass CBCT image segmentation for orthodontics with deep learning. J Dent Res. 100:943–9. DOI: 10.1177/00220345211005338. PMID: 33783247. PMCID: PMC8293763. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85103916050&origin=inward.5. Djeu G, Shelton C, Maganzini A. 2005; Outcome assessment of Invisalign and traditional orthodontic treatment compared with the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 128:292–8. discussion 8DOI: 10.1016/j.ajodo.2005.06.002. PMID: 16168325. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=24944502756&origin=inward.6. Cardoso PC, Espinosa DG, Mecenas P, Flores-Mir C, Normando D. 2020; Pain level between clear aligners and fixed appliances: a systematic review. Prog Orthod. 21:3. DOI: 10.1186/s40510-019-0303-z. PMID: 31956934. PMCID: PMC6970090. PMID: d90f3c99fb084e88a62487e5f7c13cf0. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85078024714&origin=inward.7. Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. 2015; Periodontal health during clear aligners treatment: a systematic review. Eur J Orthod. 37:539–43. DOI: 10.1093/ejo/cju083. PMID: 25548145. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84943399285&origin=inward.8. Gao M, Yan X, Zhao R, Shan Y, Chen Y, Jian F, et al. 2021; Comparison of pain perception, anxiety, and impacts on oral health-related quality of life between patients receiving clear aligners and fixed appliances during the initial stage of orthodontic treatment. Eur J Orthod. 43:353–9. DOI: 10.1093/ejo/cjaa037. PMID: 32613250. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85108021587&origin=inward.9. Flores-Mir C, Brandelli J, Pacheco-Pereira C. 2018; Patient satisfaction and quality of life status after 2 treatment modalities: Invisalign and conventional fixed appliances. Am J Orthod Dentofacial Orthop. 154:639–44. DOI: 10.1016/j.ajodo.2018.01.013. PMID: 30384934. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85055710082&origin=inward.10. Nedwed V, Miethke RR. 2005; Motivation, acceptance and problems of invisalign patients. J Orofac Orthop. 66:162–73. DOI: 10.1007/s00056-005-0429-0. PMID: 15827703. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=17144367311&origin=inward.11. Allareddy V, Nalliah R, Lee MK, Rampa S, Allareddy V. 2017; Adverse clinical events reported during Invisalign treatment: analysis of the MAUDE database. Am J Orthod Dentofacial Orthop. 152:706–10. DOI: 10.1016/j.ajodo.2017.06.014. PMID: 29103448. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85037680411&origin=inward.12. Aljudaibi S, Duane B. 2018; Non-pharmacological pain relief during orthodontic treatment. Evid Based Dent. 19:48–9. DOI: 10.1038/sj.ebd.6401305. PMID: 29930369. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85049040205&origin=inward.13. Al-Moghrabi D, Salazar FC, Pandis N, Fleming PS. 2017; Compliance with removable orthodontic appliances and adjuncts: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 152:17–32. DOI: 10.1016/j.ajodo.2017.03.019. PMID: 28651764. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85027989284&origin=inward.14. Charavet C, Le Gall M, Albert A, Bruwier A, Leroy S. 2019; Patient compliance and orthodontic treatment efficacy of Planas functional appliances with TheraMon microsensors. Angle Orthod. 89:117–22. DOI: 10.2319/122917-888.1. PMID: 30080129. PMCID: PMC8137129. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85060064942&origin=inward.15. Xie X, Wang L, Wang A. 2010; Artificial neural network modeling for deciding if extractions are necessary prior to orthodontic treatment. Angle Orthod. 80:262–6. DOI: 10.2319/111608-588.1. PMID: 19905850. PMCID: PMC8973232. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=73349109176&origin=inward.16. Tanikawa C, Yamashiro T. 2021; Development of novel artificial intelligence systems to predict facial morphology after orthognathic surgery and orthodontic treatment in Japanese patients. Sci Rep. 11:15853. DOI: 10.1038/s41598-021-95002-w. PMID: 34349151. PMCID: PMC8339122. PMID: bb2f34d5f53b4b17816e592c84a123ca. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85111995713&origin=inward.17. Jung SK, Kim TW. 2016; New approach for the diagnosis of extractions with neural network machine learning. Am J Orthod Dentofacial Orthop. 149:127–33. DOI: 10.1016/j.ajodo.2015.07.030. PMID: 26718386. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84951823832&origin=inward.18. He SL, Wang JH. 2015; Reliability and validity of a Chinese version of the Oral Health Impact Profile for edentulous subjects. Qual Life Res. 24:1011–6. DOI: 10.1007/s11136-014-0822-5. PMID: 25298052. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84925510890&origin=inward.19. Zhang Y, Liu R, Li G, Mao S, Yuan Y. 2015; The reliability and validity of a Chinese-version Short Health Anxiety Inventory: an investigation of university students. Neuropsychiatr Dis Treat. 11:1739–47. DOI: 10.2147/NDT.S83501. PMID: 26213472. PMCID: PMC4509540. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84937547929&origin=inward.20. Katz J, Melzack R. 1999; Measurement of pain. Surg Clin North Am. 79:231–52. DOI: 10.1016/S0039-6109(05)70381-9. PMID: 10352653. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0032915924&origin=inward.21. Simonyan K, Zisserman A. 2014. Very deep convolutional networks for large-scale image recognition. arXiv. 1409.1556 [Preprint]. Available from: https://doi.org/10.48550/arXiv.1409.1556. cited 2020 Apr 1.22. Wanto A, Windarto AP, Hartama D, Parlina I. 2017; Use of binary sigmoid function and linear identity in artificial neural networks for forecasting population density. IJISTECH. 1:43–54. DOI: 10.30645/ijistech.v1i1.6.23. Li P, Kong D, Tang T, Su D, Yang P, Wang H, et al. 2019; Orthodontic treatment planning based on artificial neural networks. Sci Rep. 9:2037. DOI: 10.1038/s41598-018-38439-w. PMID: 30765756. PMCID: PMC6375961. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85061613078&origin=inward.24. Kingma DP, Ba J. 2014. Adam: a method for stochastic optimization. arXiv. 1412.6980 [Preprint]. Available from: https://doi.org/10.48550/arXiv.1412.6980. cited 2020 Apr 1.25. Guyon I. 1997. A scaling law for the validation-set training-set size ratio. AT & T Bell Laboratories;Murray Hill: DOI: 10.30645/ijistech.v1i1.6.26. Sug H. 2010; The effect of training set size for the performance of neural networks of classification. WSEAS Trans Comput. 9:1297–306. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0032915924&origin=inward.27. Youden WJ. 1950; Index for rating diagnostic tests. Cancer. 3:32–5. DOI: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3. PMID: 15405679.28. Gevrey M, Dimopoulos I, Lek S. 2003; Review and comparison of methods to study the contribution of variables in artificial neural network models. Ecol Model. 160:249–64. DOI: 10.1016/S0304-3800(02)00257-0. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0037442845&origin=inward.29. Keith DJ, Rinchuse DJ, Kennedy M, Zullo T. 2013; Effect of text message follow-up on patient's self-reported level of pain and anxiety. Angle Orthod. 83:605–10. DOI: 10.2319/091812-742.1. PMID: 23210546. PMCID: PMC8754025. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84881045228&origin=inward.30. Bartlett BW, Firestone AR, Vig KW, Beck FM, Marucha PT. 2005; The influence of a structured telephone call on orthodontic pain and anxiety. Am J Orthod Dentofacial Orthop. 128:435–41. DOI: 10.1016/j.ajodo.2004.06.033. PMID: 16214624. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=26444491029&origin=inward.31. Liu JL, Li SH, Cai YM, Lan DP, Lu YF, Liao W, et al. 2021; Automated radiographic evaluation of adenoid hypertrophy based on VGG-lite. J Dent Res. 100:1337–43. DOI: 10.1177/00220345211009474. PMID: 33913367. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85105719954&origin=inward.32. Yu HJ, Cho SR, Kim MJ, Kim WH, Kim JW, Choi J. 2020; Automated skeletal classification with lateral cephalometry based on artificial intelligence. J Dent Res. 99:249–56. DOI: 10.1177/0022034520901715. PMID: 31977286. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85078321951&origin=inward.33. Thai JK, Araujo E, McCray J, Schneider PP, Kim KB. 2020; Esthetic perception of clear aligner therapy attachments using eye-tracking technology. Am J Orthod Dentofacial Orthop. 158:400–9. DOI: 10.1016/j.ajodo.2019.09.014. PMID: 32620476. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85087220324&origin=inward.34. Masood Y, Masood M, Zainul NN, Araby NB, Hussain SF, Newton T. 2013; Impact of malocclusion on oral health related quality of life in young people. Health Qual Life Outcomes. 11:25. DOI: 10.1186/1477-7525-11-25. PMID: 23443041. PMCID: PMC3598523. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84874218610&origin=inward.35. Wang J, Tang X, Shen Y, Shang G, Fang L, Wang R, et al. 2015; The correlations between health-related quality of life changes and pain and anxiety in orthodontic patients in the initial stage of treatment. Biomed Res Int. 2015:725913. DOI: 10.1155/2015/725913. PMID: 25685804. PMCID: PMC4317575. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84922391022&origin=inward.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Classification and prediction of the effects of nutritional intake on diabetes mellitus using artificial neural network sensitivity analysis: 7th Korea National Health and Nutrition Examination Survey
- A Narrative Review on the Application of Artificial Intelligence on the Diagnosis and Outcome Prediction for Spinal Diseases
- Artificial neural network model for predicting sex using dental and orthodontic measurements
- On the Use of Neural Networks for the Risk Factor Analysis of NIDDM
- Artificial Neural Network: Understanding the Basic Concepts without Mathematics