J Yeungnam Med Sci.
2022 Jul;39(3):250-255. 10.12701/yujm.2021.01256.
Pedunculated mucinous cystic neoplasm of the liver: a case report
- Affiliations
-
- 1Department of Surgery Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2532079
- DOI: http://doi.org/10.12701/yujm.2021.01256
Abstract
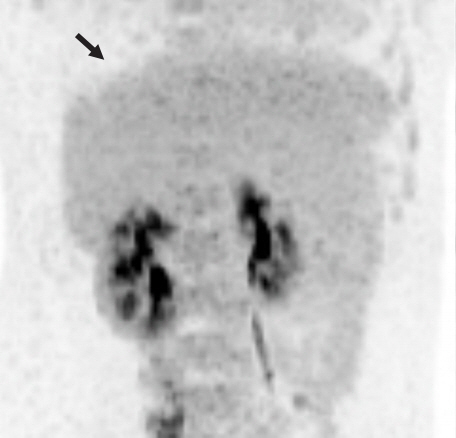
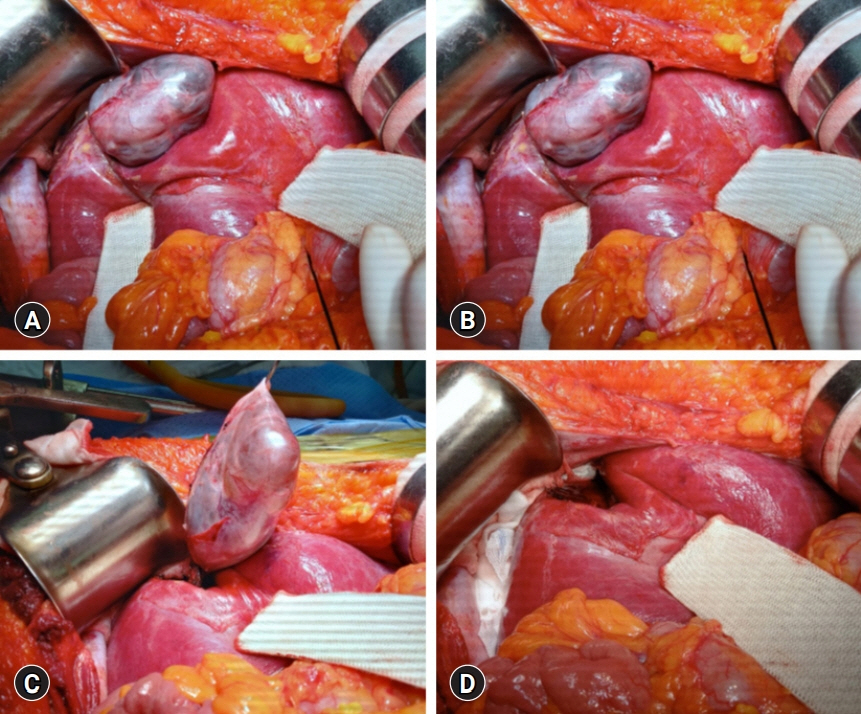
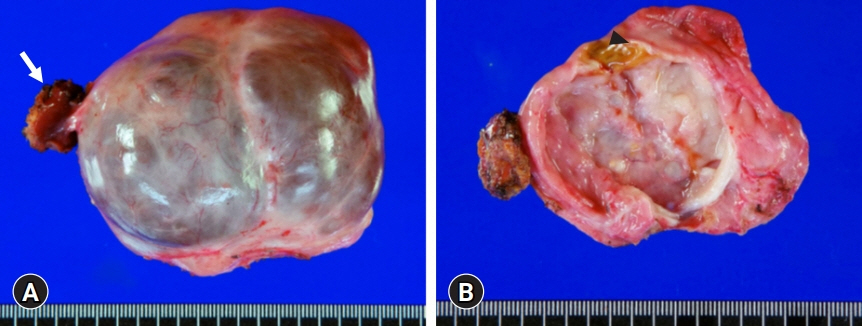
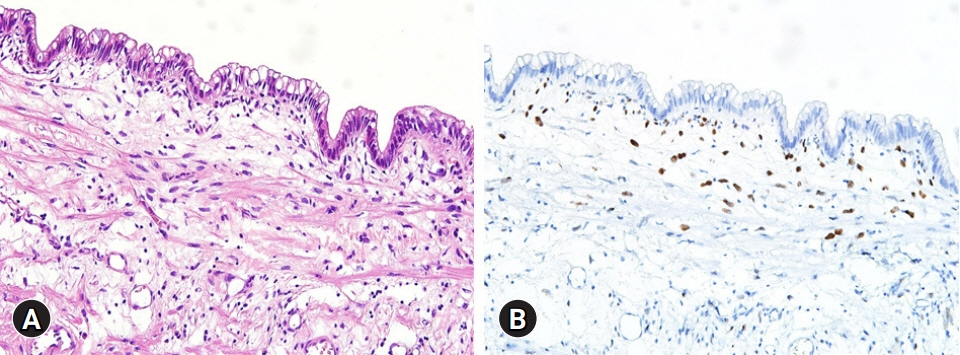
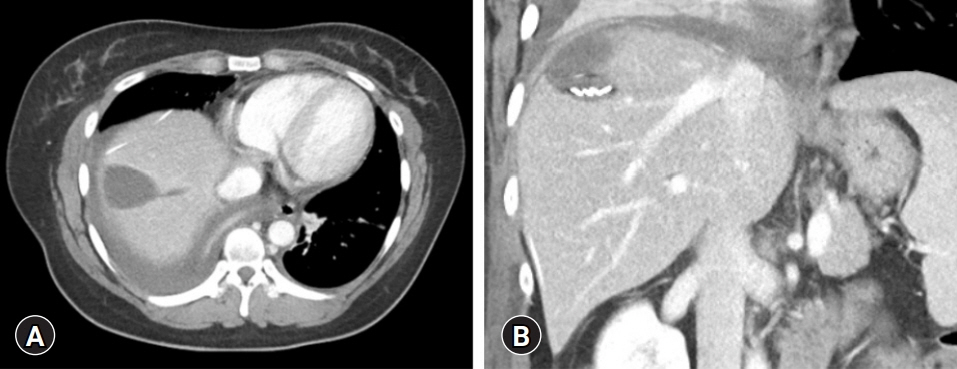
- In 2010, the World Health Organization classified mucin-producing bile duct tumors of the liver into two distinct entities; mucinous cystic neoplasm of the liver (MCN-L) and intraductal papillary mucinous neoplasm of the bile duct. We present the case of a patient with MCN-L having a uniquely pedunculated shape. A 32‐year‐old woman was referred to our institution with a diagnosis of biliary cystic neoplasm. She had undergone left salpingo-oophorectomy for ovarian cancer 15 years ago. Imaging studies showed an 8 cm-sized well defined, multiloculated cystic lesion suggesting a mucinous cystic neoplasm. The cystic mass was pedunculated at the liver capsule and pathologically diagnosed as MCN-L. The mass was resected with partial hepatectomy. The patient recovered uneventfully. She was discharged 7 days postoperatively. The patient has been doing well for 6 months after the operation. The patient will be followed up annually because of the favorable postresection prognosis of MCN-L.
Keyword
Figure
Reference
-
References
1. Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 2014; 21:176–85.
Article2. Obara S, Nomi T, Yamato I, Hokuto D, Yasuda S, Nishiwada S, et al. Laparoscopic resection of a hepatic mucinous cystic neoplasm: a case report. Int J Surg Case Rep. 2016; 24:18–21.
Article3. Nakayama Y, Kato Y, Okubo S, Takahashi D, Okada R, Nishida Y, et al. A case of mucinous cystic neoplasm of the liver: a case report. Surg Case Rep. 2015; 1:9.
Article4. Li T, Ji Y, Zhi XT, Wang L, Yang XR, Shi GM, et al. A comparison of hepatic mucinous cystic neoplasms with biliary intraductal papillary neoplasms. Clin Gastroenterol Hepatol. 2009; 7:586–93.
Article5. Budzynska A, Hartleb M, Nowakowska-Dulawa E, Krol R, Remiszewski P, Mazurkiewicz M. Simultaneous liver mucinous cystic and intraductal papillary mucinous neoplasms of the bile duct: a case report. World J Gastroenterol. 2014; 20:4102–5.
Article6. Ghatak S, Ray S, Sonar PK, Das S, Basu K, Mridha AR, et al. Giant mucinous cystic neoplasms of pancreas and liver with unusual adipose tissue component: a case report. J Gastrointest Oncol. 2012; 3:353–7.7. Zen Y, Pedica F, Patcha VR, Capelli P, Zamboni G, Casaril A, et al. Mucinous cystic neoplasms of the liver: a clinicopathological study and comparison with intraductal papillary neoplasms of the bile duct. Mod Pathol. 2011; 24:1079–89.
Article8. Simo KA, Mckillop IH, Ahrens WA, Martinie JB, Iannitti DA, Sindram D. Invasive biliary mucinous cystic neoplasm: a review. HPB (Oxford). 2012; 14:725–40.
Article9. Jwa EK, Hwang S. Clinicopathological features and post-resection outcomes of biliary cystadenoma and cystadenocarcinoma of the liver. Ann Hepatobiliary Pancreat Surg. 2017; 21:107–13.
Article10. Wang X, Cai YQ, Chen YH, Liu XB. Biliary tract intraductal papillary mucinous neoplasm: report of 19 cases. World J Gastroenterol. 2015; 21:4261–7.
Article11. Zen Y, Jang KT, Ahn S, Kim DH, Choi DW, Choi SH, et al. Intraductal papillary neoplasms and mucinous cystic neoplasms of the hepatobiliary system: demographic differences between Asian and Western populations, and comparison with pancreatic counterparts. Histopathology. 2014; 65:164–73.
Article12. Takano Y, Nagahama M, Yamamura E, Maruoka N, Mizukami H, Tanaka J, et al. Prolapse into the bile duct and expansive growth is characteristic behavior of mucinous cystic neoplasm of the liver: report of two cases and review of the literature. Clin J Gastroenterol. 2015; 8:148–55.
Article13. Kim KM, Lee JK, Shin JU, Lee KH, Lee KT, Sung JY, et al. Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype. Am J Gastroenterol. 2012; 107:118–25.
Article14. Wan XS, Xu YY, Qian JY, Yang XB, Wang AQ, He L, et al. Intraductal papillary neoplasm of the bile duct. World J Gastroenterol. 2013; 19:8595–604.
Article15. Kunovsky L, Kala Z, Svaton R, Moravcik P, Mazanec J, Husty J, et al. Mucinous cystic neoplasm of the liver or intraductal papillary mucinous neoplasm of the bile duct? A case report and a review of literature. Ann Hepatol. 2018; 17:519–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreatic Collision Tumor of Desmoid-Type Fibromatosis and Mucinous Cystic Neoplasm: A Case Report
- Duodenal Mucinous Carcinoma: A Case Report
- Multilocular cystic hemangioma of the liver mimicking mucinous cystic neoplasm: a case report
- Fine Needle Aspiration Cytology of Mucinous Cystic Carcinoma of the Pancreas: A Case Report
- Cystic Degeneration of Hepatocellular Carcinoma Mimicking Mucinous Cystic Neoplasm