J Rhinol.
2022 Jul;29(2):112-117. 10.18787/jr.2021.00397.
A Case of Primary Diffuse Large B Cell Lymphoma of the Maxillary Sinus Presenting as Epiphora
- Affiliations
-
- 1Department of Otorhinolaryngology, Head and Neck Surgery, Dong-A University, College of Medicine, Busan, Republic of Korea
- 2Department of Pathology, Dong-A University, College of Medicine, Busan, Republic of Korea
- KMID: 2532014
- DOI: http://doi.org/10.18787/jr.2021.00397
Abstract
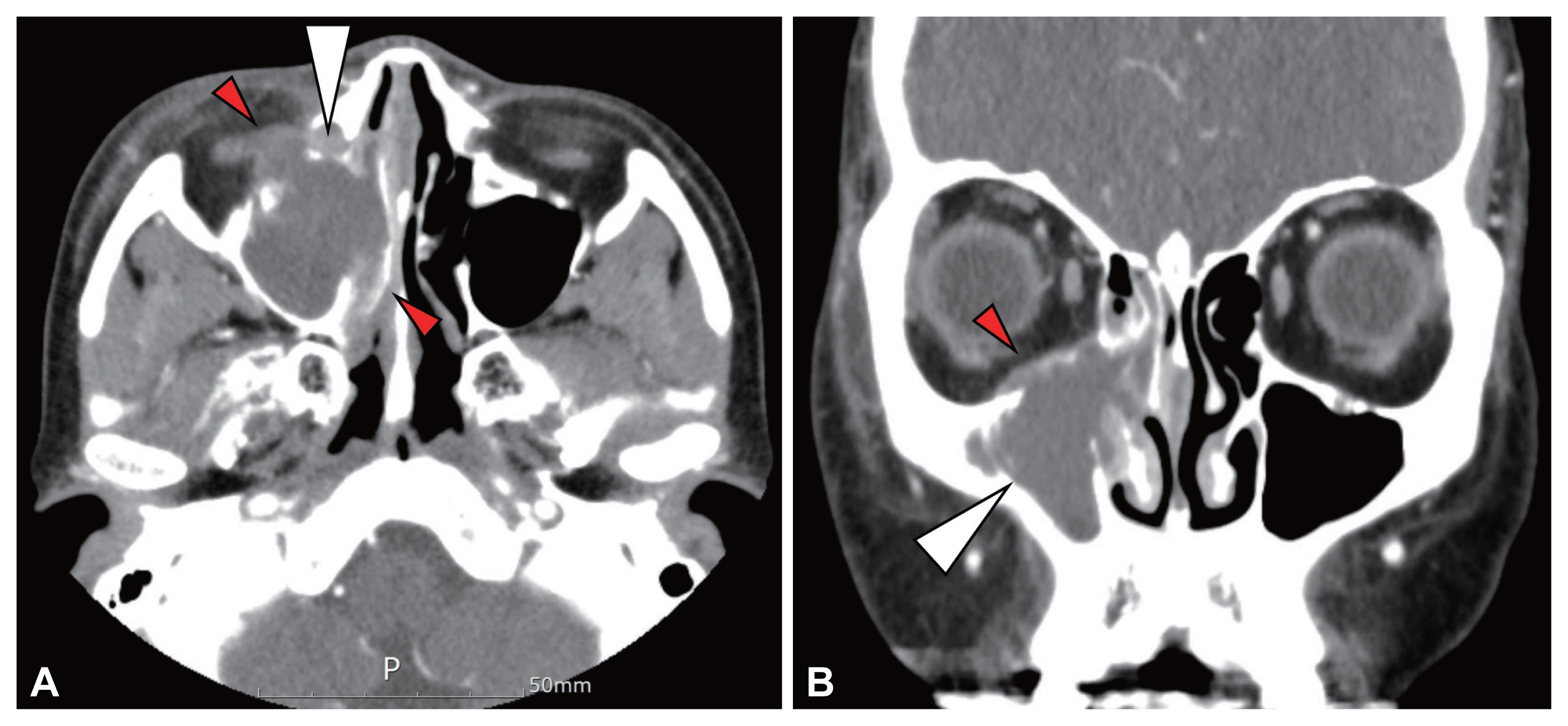
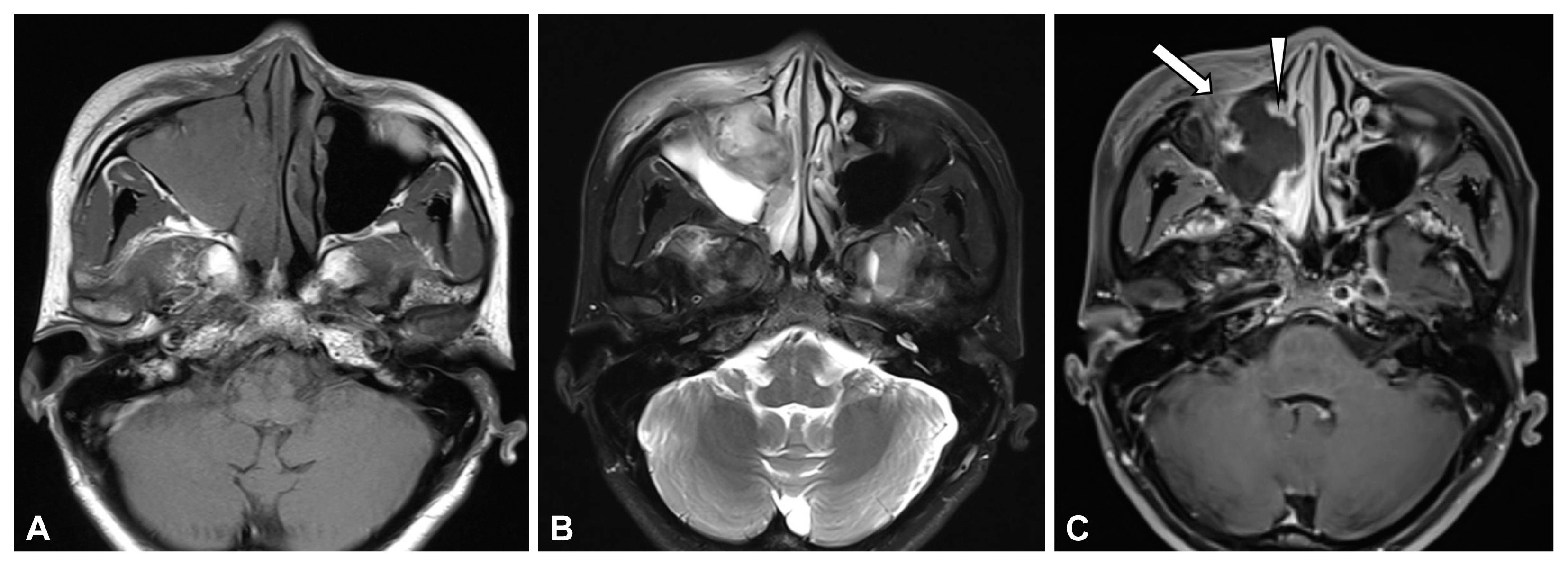
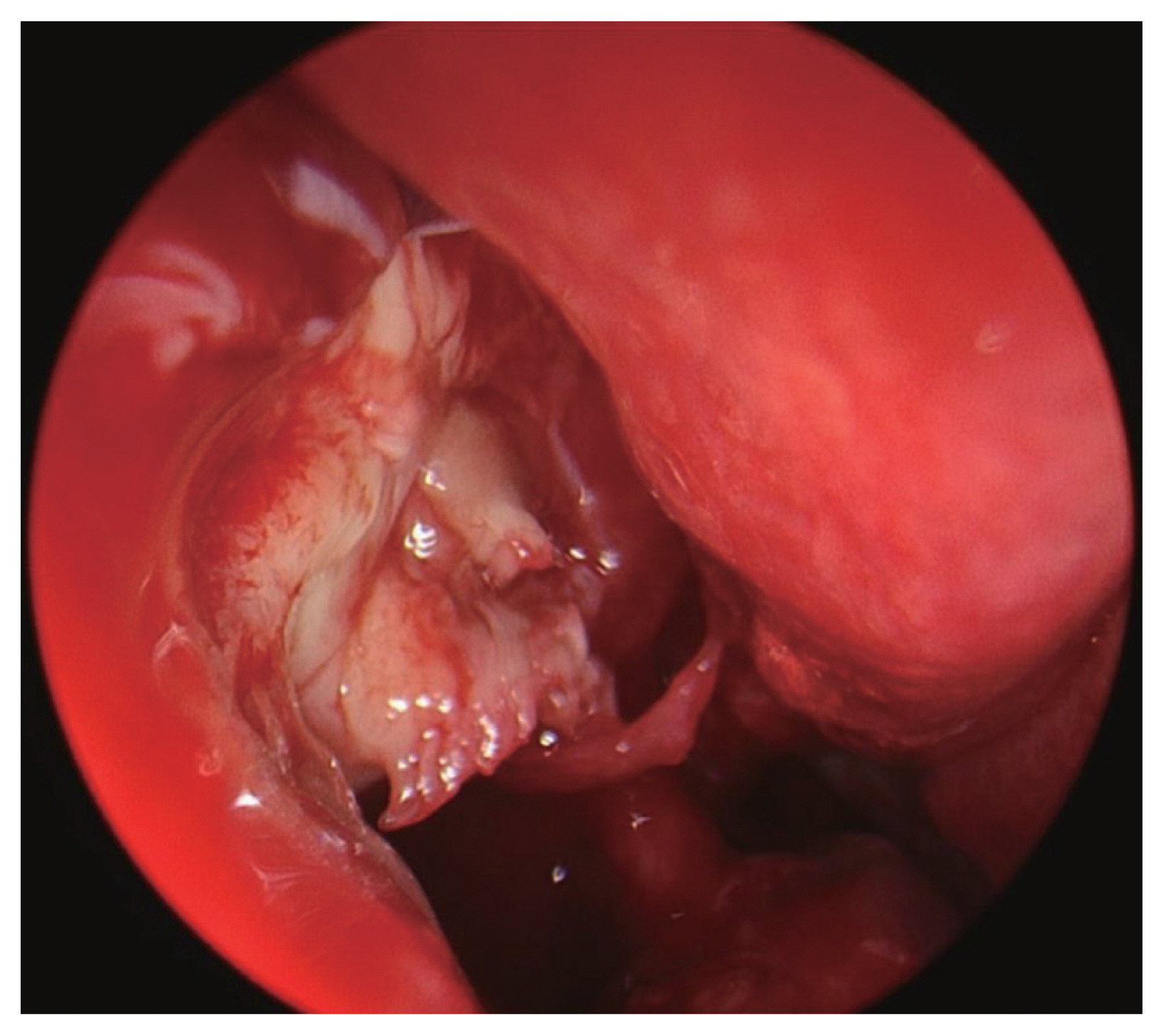
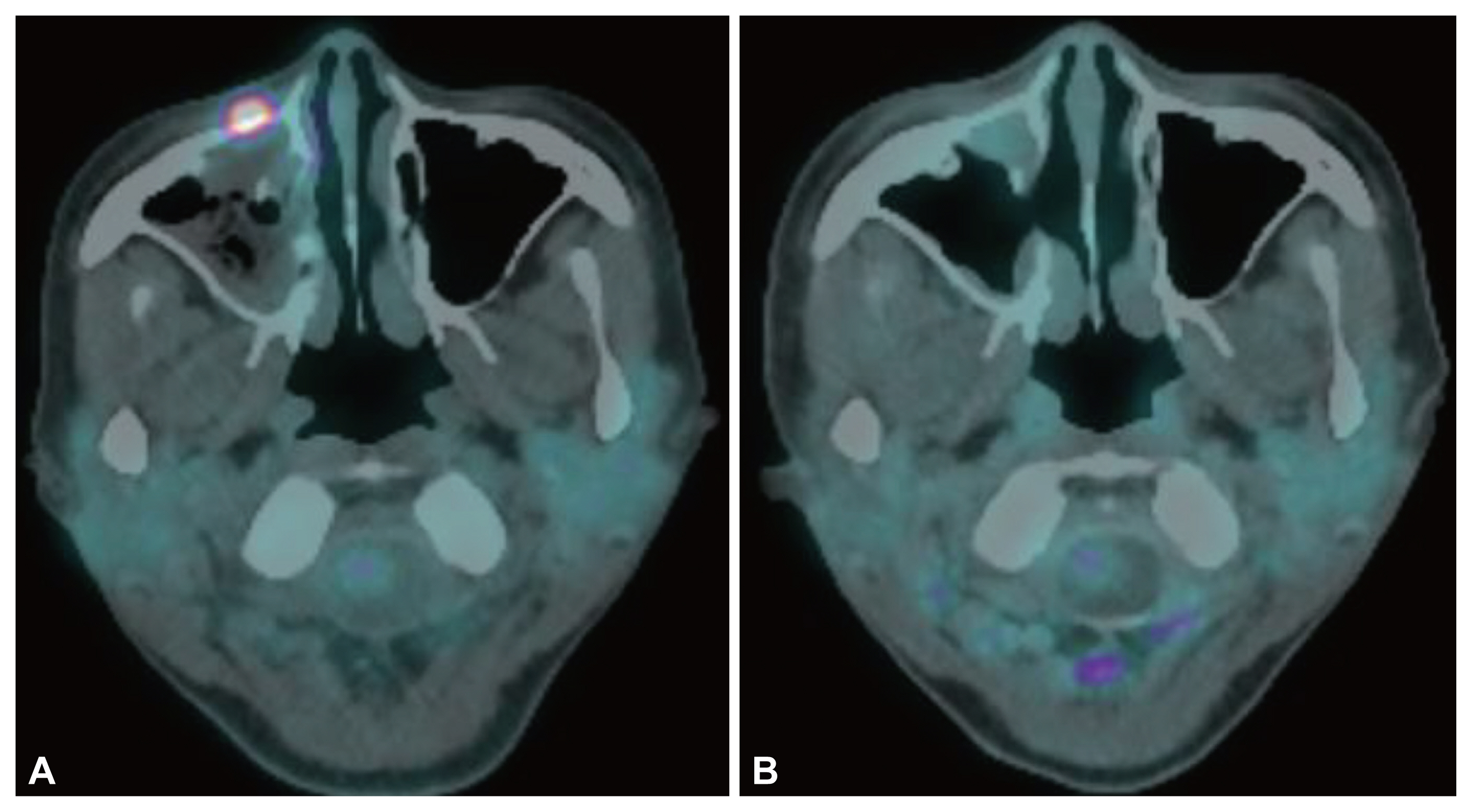
- Primary sinusoidal non-Hodgkin’s lymphoma (NHL) is a very rare disease. The main symptoms of sinusoidal NHL are rhinorrhea, nasal obstruction, and post-nasal drip. Symptoms such as eye protrusion, diplopia, trismus, and periorbital pain can also occur. Epiphora is a very rare symptom of sinusoidal NHL, which can lead to a misdiagnosis of dacryocystitis or dacryostenosis. The authors report the case of a 46-year-old female patient who visited hospital for symptoms of epiphora, which did not improve even after 3 months of eye treatment, leading to a final diagnosis of maxillary NHL.
Figure
Reference
-
1. Quraishi MS, Bessell EM, Clark D, Jones NS, Bradley PJ. Non-Hodgkin’s lymphoma of the sinonasal tract. Laryngoscope. 2000; 110(9):1489–92.2. Swain SK, Acharya S. Extranodal non-Hodgkin’s lymphoma of the sinonasal tract: a review. BLDE Univ J Health Sci. 2021; 6(1):1–6.3. Kolokotronis A, Konstantinou N, Christakis I, Papadimitriou P, Matiakis A, Zaraboukas T, et al. Localized B-cell non-Hodgkin’s lymphoma of oral cavity and maxillofacial region: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99(3):303–10.4. Nemet AY. The etiology of epiphora: a multifactorial issue. Semin Ophthalmol. 2016; 31(3):275–9.5. Merkonidis C, Brewis C, Yung M, Nussbaumer M. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol. 2005; 89(12):1589–91.6. Capra GG, Carbone PN, Mullin DP. Paranasal sinus mucocele. Head Neck Pathol. 2012; 6(3):369–72.7. Sandner A, Surov A, Bach AG, Kösling S. Primary extranodal non-Hodgkin lymphoma of the orbital and paranasal region-a retrospective study. Eur J Radiol. 2013; 82(2):302–8.8. Wilder RB, Romaguera JE, Tucker SL, Ha CS, Hess MA, Cabanillas F, et al. Results with chemotherapy comprised of cyclophosphamide, doxorubicin, vincristine, and prednisone followed by radiotherapy with or without prechemotherapy surgical debulking for patients with bulky, aggressive lymphoma. Cancer. 2002; 94(3):601–5.9. Hanna E, Wanamaker J, Adelstein D, Tubbs R, Lavertu P. Extranodal lymphomas of the head and neck. A 20-year experience. Arch Otolaryngol Head Neck Surg. 1997; 123(12):1318–23.10. Logsdon MD, Ha CS, Kavadi VS, Cabanillas F, Hess MA, Cox JD. Lymphoma of the nasal cavity and paranasal sinuses: improved outcome and altered prognostic factors with combined modality therapy. Cancer. 1997; 80(3):477–88.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non Hodgkin lymphoma in the maxillary sinus mimicking dental abscess: a case report
- Imaging characteristics of diffuse large cell extra nodal non-Hodgkin's lymphoma involving the palate and maxillary sinus: a case report
- Radiation Therapy of the Maxillary Sinus Lymphoma: A Case Report and Review of Literature
- Relapse of Ocular Lymphoma following Primary Testicular Diffuse Large B-cell Lymphoma
- A Case of Primary Cutaneous Diffuse Large B-cell Lymphoma