J Rhinol.
2022 Jul;29(2):106-111. 10.18787/jr.2021.00387.
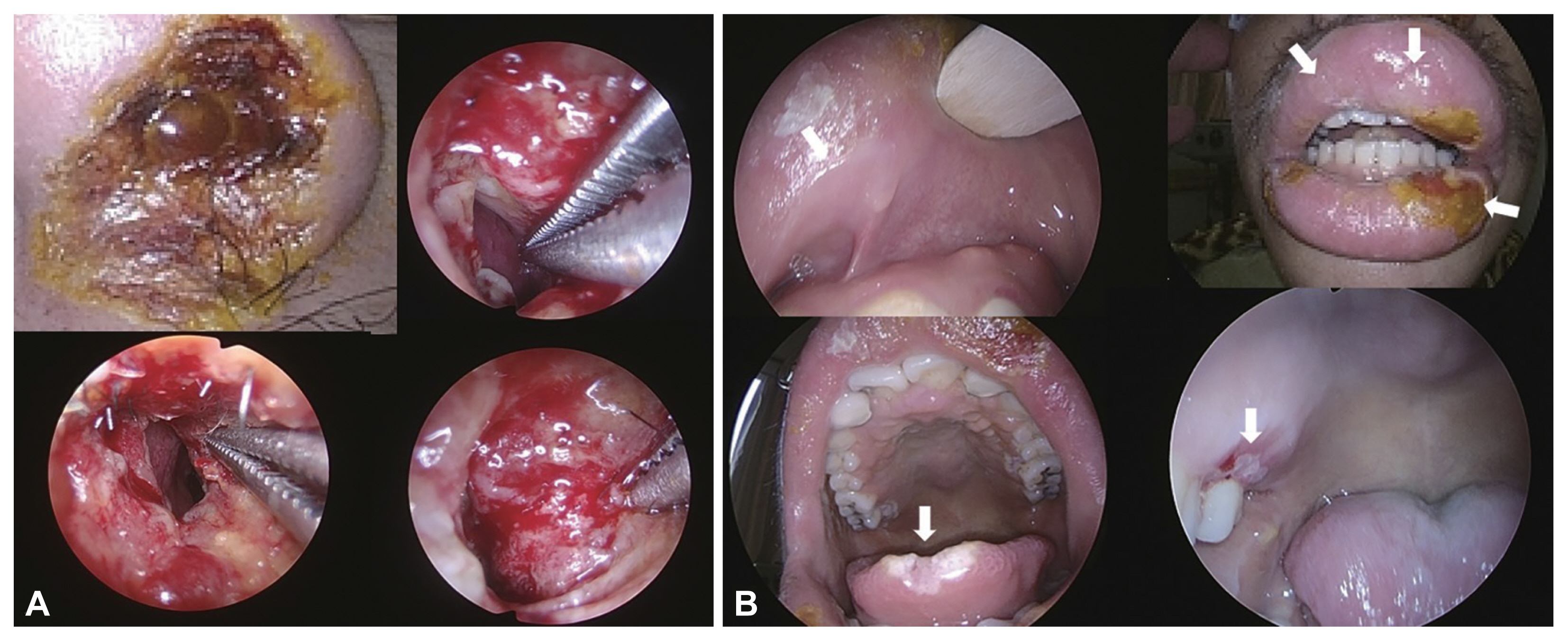
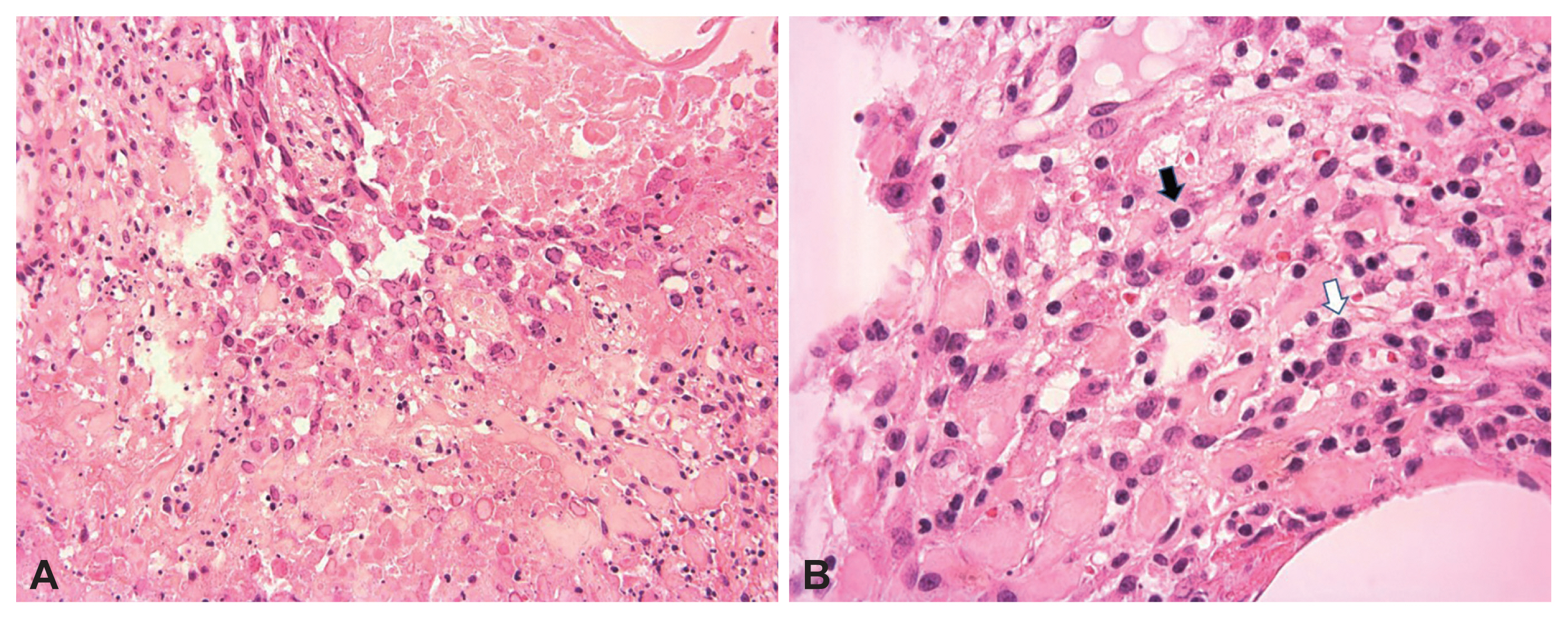
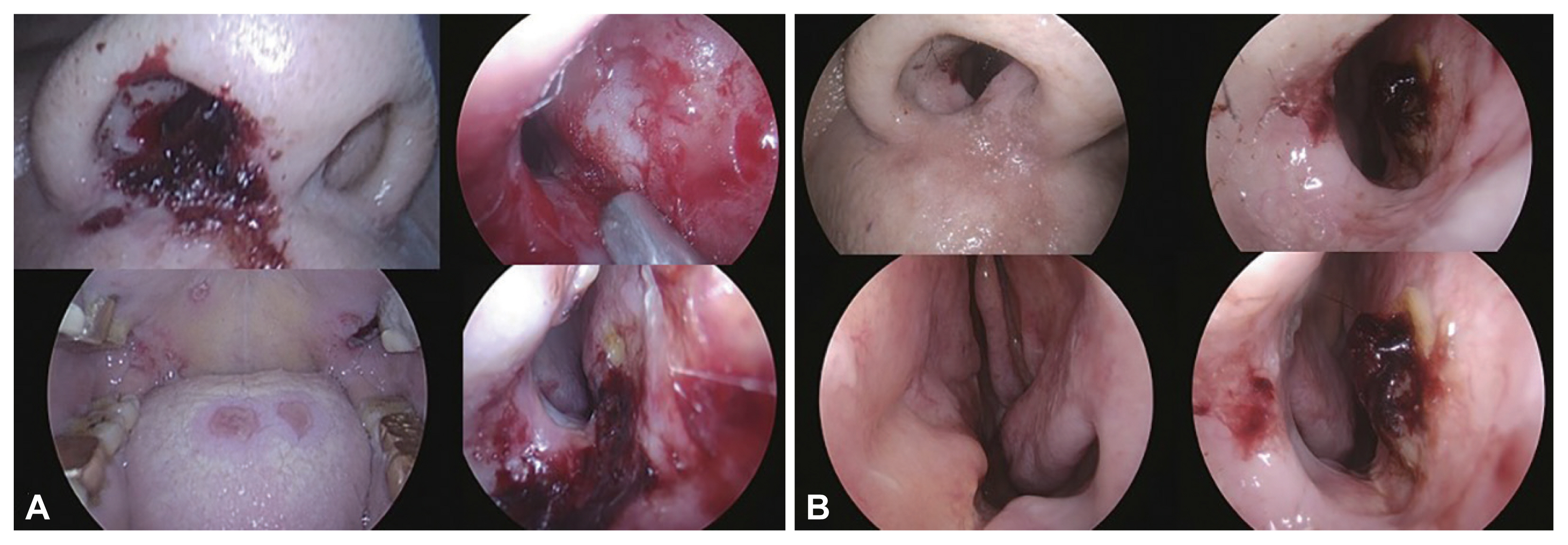
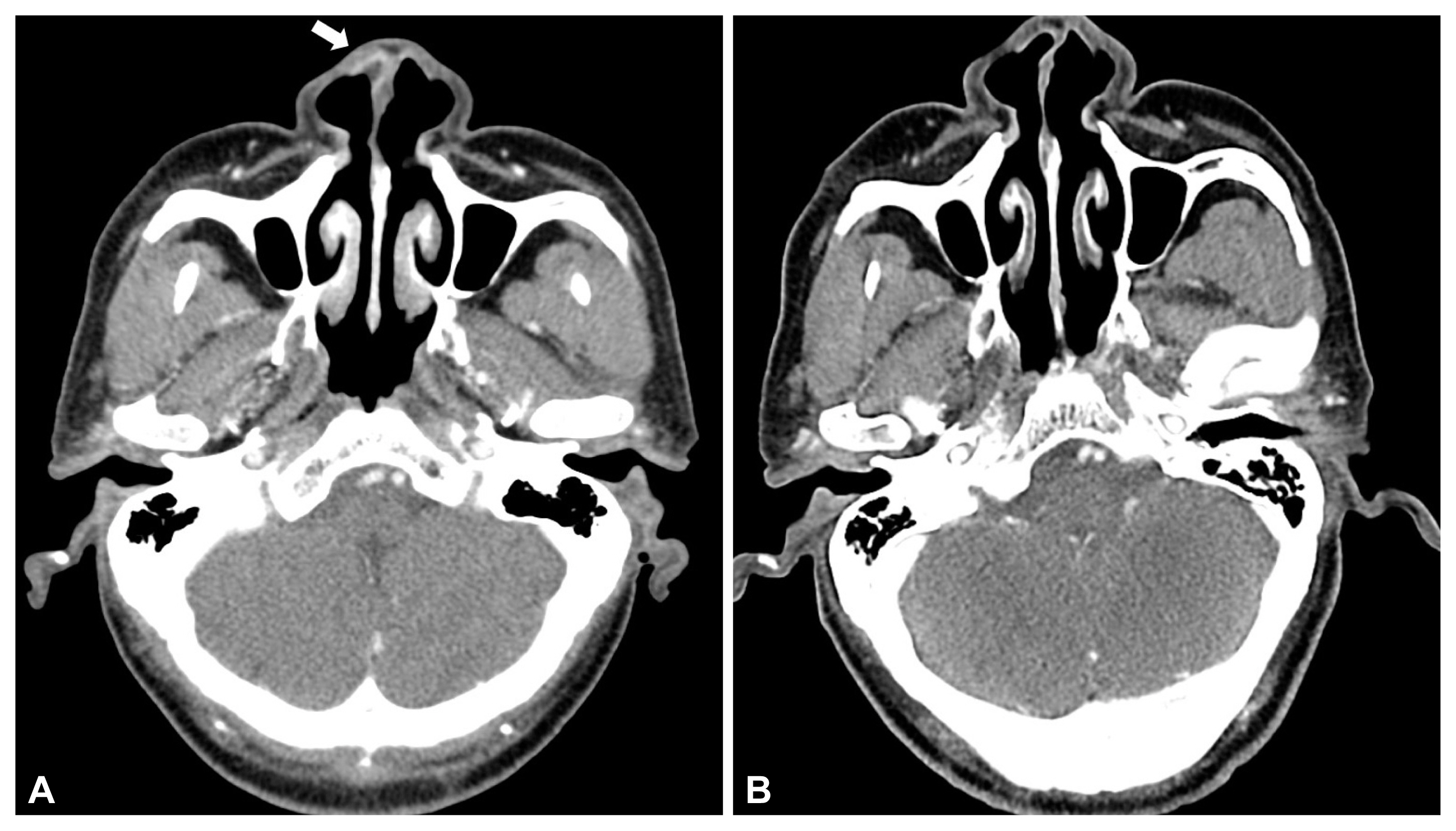
Two Cases of Herpes Virus Infection of Nose Mimicking Acute Invasive Fungal Infection in Immunocompromised Hosts
- Affiliations
-
- 1Departments of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- KMID: 2532013
- DOI: http://doi.org/10.18787/jr.2021.00387
Abstract
- Various invasive fungal infections can occur in immunocompromised hosts, and an acute invasive fungal infection (AIFI) can be fatal. Because of its high mortality rate, AIFI must be quickly diagnosed and treated, such as anti-fungal agents or surgical debridement. In an immunocompromised host, nasal herpes simplex infection, usually caused by herpes simplex virus (HSV) type-1, can have various clinical manifestations, some of which can mimic AIFI. However, the management of acute viral infection differs significantly from invasive fungal infections of the nose. A fast and accurate differential diagnosis is mandatory because a delay in the disease-specific treatment of acute invasive infections can lead to mortality. This report describes two immunocompromised patients with mucosal and skin lesions around the nose. We provide clinical clues when mucosal lesions of the nasal cavity and skin lesions around the nose develop in immunocompromised hosts.
Figure
Reference
-
1. Wandell GM, Miller C, Rathor A, Wai TH, Guyer RA, Schmidt RA, et al. A multi-institutional review of outcomes in biopsy-proven acute invasive fungal sinusitis. Int Forum Allergy Rhinol. 2018; 8(12):1459–68.2. deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R. A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 1997; 123(11):1181–8.3. Montone KT. Infectious diseases of the head and neck: a review. Am J Clin Pathol. 2007; 128(1):35–67.4. Hoyt B, Bhawan J. Histological spectrum of cutaneous herpes infections. Am J Dermatopathol. 2014; 36(8):609–19.5. Turner JH, Soudry E, Nayak JV, Hwang PH. Survival outcomes in acute invasive fungal sinusitis: a systematic review and quantitative synthesis of published evidence. Laryngoscope. 2013; 123(5):1112–8.6. Yohai RA, Bullock JD, Aziz AA, Markert RJ. Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994; 39(1):3–22.7. DelGaudio JM, Clemson LA. An early detection protocol for invasive fungal sinusitis in neutropenic patients successfully reduces extent of disease at presentation and long term morbidity. Laryngoscope. 2009; 119(1):180–3.8. Rizk SS, Kraus DH, Gerresheim G, Mudan S. Aggressive combination treatment for invasive fungal sinusitis in immunocompromised patients. Ear Nose Throat J. 2000; 79(4):278–80. 282284–5.9. DelGaudio JM, Swain RE Jr, Kingdom TT, Muller S, Hudgins PA. Computed tomographic findings in patients with invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 2003; 129(2):236–40.10. Montone KT. Pathology of fungal rhinosinusitis: a review. Head Neck Pathol. 2016; 10(1):40–6.11. Montone KT, Livolsi VA, Feldman MD, Palmer J, Chiu AG, Lanza DC, et al. Fungal rhinosinusitis: a retrospective microbiologic and pathologic review of 400 patients at a single university medical center. Int J Otolaryngol. 2012; 2012:684835.12. Montone KT. Differential diagnosis of necrotizing sinonasal lesions. Arch Pathol Lab Med. 2015; 139(12):1508–14.13. Patel NA, Kessel R, Zahtz G. Herpes simplex virus of the nose masquerading as invasive fungal sinusitis: a pediatric case series. Am J Otolaryngol. 2019; 40(4):609–11.14. Ramchandani M, Kong M, Tronstein E, Selke S, Mikhaylova A, Magaret A, et al. Herpes simplex virus type 1 shedding in tears and nasal and oral mucosa of healthy adults. Sex Transm Dis. 2016; 43(12):756–60.15. Powell HR, Almeyda J. An immunocompetent patient presenting with severe nasal herpes simplex: a case report. Cases J. 2009; 2:9079.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Disseminated Herpes Simplex Virus Infection in Immunocompromised Patient
- A Case of Herpes Zoster Duplex Bilateralis, a Diagnostic Clue of Human Immunodeficiency Virus Infection
- Two Cases of Chickenpox Developed from an Immunocompromised Patient with Localized Herpes Zoster
- Fulminant hepatitis and myocarditis associated with varicella zoster virus infection in a kidney transplant recipient: a case report
- A Case of Postoperative Herpes Simplex Pneumonia