J Neurocrit Care.
2022 Jun;15(1):69-75. 10.18700/jnc.210036.
Recanalization of the middle cerebral artery after prolonged induced hypertensive therapy to rescue early neurologic deterioration: a case report
- Affiliations
-
- 1Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Department of Neurology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2532004
- DOI: http://doi.org/10.18700/jnc.210036
Abstract
- Background
Although decades have passed since the introduction of pharmacologically induced hypertensive therapy (PIHT) against early neurologic deterioration (END) in acute ischemic stroke, the optimal duration of PIHT remains elusive.
Case Report
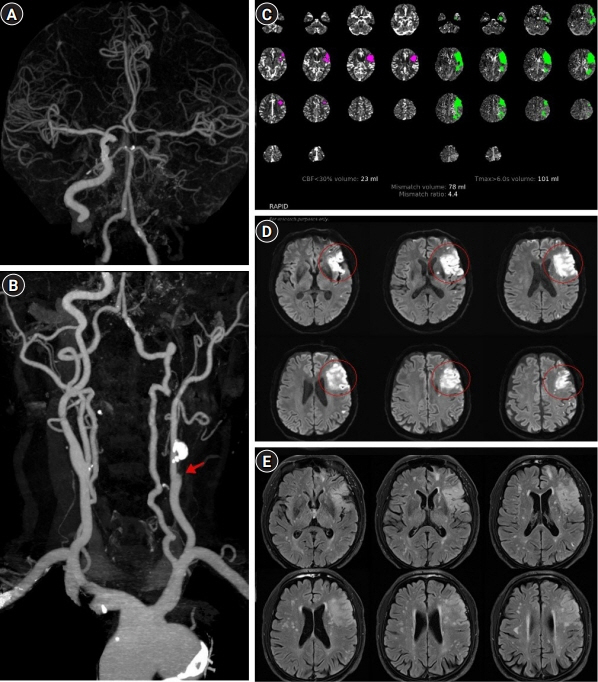
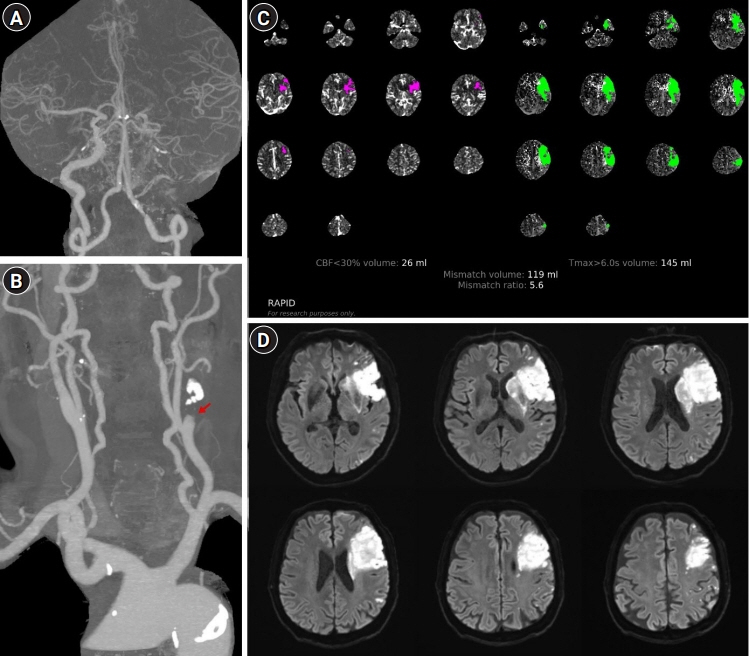
A 70-year-old man developed right hemiplegia and aphasia 25 hours before arrival. Computed tomography angiography (CTA) revealed acute infarction in the left middle cerebral artery (MCA) territory and occlusion of the left internal carotid artery. He experienced END 36 hours after admission, and CTA revealed a newly developed proximal MCA occlusion. PIHT was initiated to augment cerebral perfusion. As his neurologic symptoms were highly dependent on blood pressure, PIHT was inevitably sustained for over 3 weeks. Follow-up CTA revealed recanalization of the MCA.
Conclusion
Although further investigation is required to expedite the future clinical application, prolonged PIHT may serve as a viable collateral-enhancing treatment for a certain subset of patients with END without alternative treatment options.
Figure
Reference
-
1. Siegler JE, Martin-Schild S. Early neurological deterioration (END) after stroke: the END depends on the definition. Int J Stroke. 2011; 6:211–2.
Article2. Seners P, Turc G, Oppenheim C, Baron JC. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry. 2015; 86:87–94.
Article3. Bang OY, Chung JW, Kim SK, Kim SJ, Lee MJ, Hwang J, et al. Therapeutic-induced hypertension in patients with noncardioembolic acute stroke. Neurology. 2019; 93:e1955–63.
Article4. Koenig MA, Geocadin RG, de Grouchy M, Glasgow J, Vimal S, Restrepo L, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care. 2006; 4:3–7.
Article5. Bevan JA, Duckworth J, Laher I, Oriowo MA, McPherson GA, Bevan RD. Sympathetic control of cerebral arteries: specialization in receptor type, reserve, affinity, and distribution. FASEB J. 1987; 1:193–8.
Article6. Lee MH, Kim JG, Jeon SB, Kang DW, Kwon SU, Kim JS. Pharmacologically induced hypertension therapy for acute stroke patients. J Stroke. 2019; 21:228–30.
Article7. Alawneh JA, Moustafa RR, Baron JC. Hemodynamic factors and perfusion abnormalities in early neurological deterioration. Stroke. 2009; 40:e443–50.
Article8. Kim JT, Park MS, Chang J, Lee JS, Choi KH, Cho KH. Proximal arterial occlusion in acute ischemic stroke with low NIHSS scores should not be considered as mild stroke. PLoS One. 2013; 8:e70996.
Article9. Saleem Y, Nogueira RG, Rodrigues GM, Kim S, Sharashidze V, Frankel M, et al. Acute neurological deterioration in large vessel occlusions and mild symptoms managed medically. Stroke. 2020; 51:1428–34.
Article10. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007; 38:967–73.
Article11. Hong JM, Lee SE, Lee SJ, Lee JS, Demchuk AM. Distinctive patterns on CT angiography characterize acute internal carotid artery occlusion subtypes. Medicine (Baltimore). 2017; 96:e5722.
Article12. Asada Y, Yamashita A, Sato Y, Hatakeyama K. Thrombus formation and propagation in the onset of cardiovascular events. J Atheroscler Thromb. 2018; 25:653–64.
Article13. Mao Y, Huang Y, Zhang L, Nan G. Spontaneous recanalization of atherosclerotic middle cerebral artery occlusion: case report. Medicine (Baltimore). 2017; 96:e7372.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Induced Hypertensive Therapy in an Acute Ischemic Stroke Patient with Early Neurological Deterioration
- Late Spontaneous Recanalization of Chronic Middle Cerebral Artery Occlusion
- Meningioma Presenting as Cerebral Infarct: Case Report
- A Case of Spontaneous Spinal Epidural Hematoma Misidentified as a Middle Cerebral Artery Infarction
- Intracranial Cerebrovascular Revascularization(Extracranial-Intracranial Arterial Bypass, EIAB)