Clin Endosc.
2022 Jul;55(4):558-563. 10.5946/ce.2022.001.
Bispectral index-guided propofol sedation during endoscopic ultrasonography
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Kindai University Faculty of Medicine, Osakasayama, Japan
- 2Clinical Research Center, Kindai University Hospital, Osakasayama, Japan
- 3Second Department of Internal Medicine, Wakayama Medical University School of Medicine, Wakayama, Japan
- KMID: 2531950
- DOI: http://doi.org/10.5946/ce.2022.001
Abstract
- Background/Aims
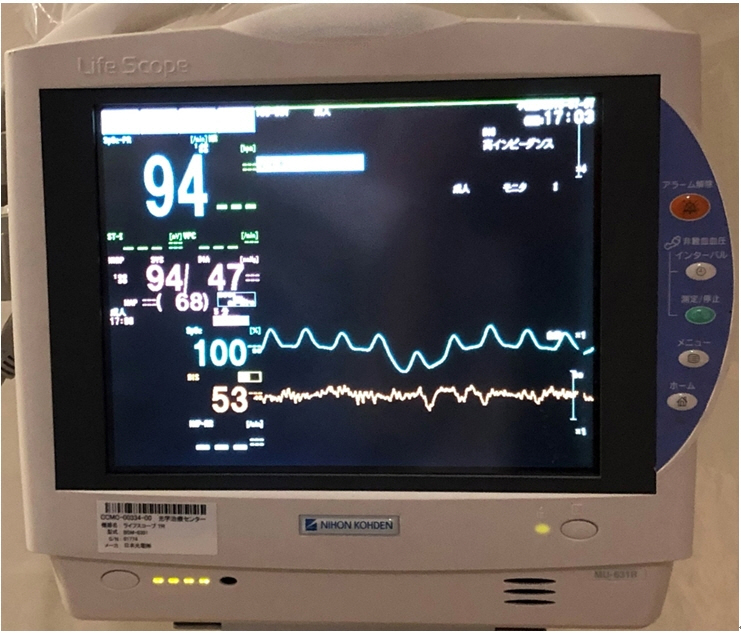
Bispectral index (BIS) monitors process and display electroencephalographic data are used to assess the depth of anesthesia. This study retrospectively evaluated the usefulness of BIS monitoring during endoscopic ultrasonography (EUS).
Methods
This study included 725 consecutive patients who underwent EUS under sedation with propofol. BIS monitoring was used in 364 patients and was not used in 361. The following parameters were evaluated: (1) median dose of propofol; (2) respiratory and circulatory depression; (3) occurrence of body movements; (4) awakening score >8 at the time; and (5) awakening score 2 hours after leaving the endoscopy room.
Results
The BIS group received a significantly lower median dose of propofol than the non-BIS group (159.2 mg vs. 167.5 mg; p=0.015) in all age groups. For patients aged ≥75 years, the reduction in heart rate was significantly lower in the BIS group than in the non-BIS group (1.2% vs. 9.1%; p=0.023). Moreover, the occurrence of body movements was markedly lower in the BIS group than in the non-BIS group (8.5% vs. 39.4%; p<0.001).
Conclusions
During EUS examination, BIS monitoring is useful for maintaining a constant depth of anesthesia, especially in patients 75 years of age or older.
Keyword
Figure
Reference
-
1. Kamata K, Takenaka M, Kitano M, et al. Contrast-enhanced harmonic endoscopic ultrasonography for differential diagnosis of localized gallbladder lesions. Dig Endosc. 2018; 30:98–106.2. Kamata K, Takenaka M, Kitano M, et al. Contrast-enhanced harmonic endoscopic ultrasonography for differential diagnosis of submucosal tumors of the upper gastrointestinal tract. J Gastroenterol Hepatol. 2017; 32:1686–1692.3. Cheriyan DG, Byrne MF. Propofol use in endoscopic retrograde cholangiopancreatography and endoscopic ultrasound. World J Gastroenterol. 2014; 20:5171–5176.4. Amornyotin S, Leelakusolvong S, Chalayonnawin W, et al. Age-dependent safety analysis of propofol-based deep sedation for ERCP and EUS procedures at an endoscopy training center in a developing country. Clin Exp Gastroenterol. 2012; 5:123–128.5. Lee TH, Lee CK, Park SH, et al. Balanced propofol sedation versus propofol monosedation in therapeutic pancreaticobiliary endoscopic procedures. Dig Dis Sci. 2012; 57:2113–2121.6. Pagano N, Arosio M, Romeo F, et al. Balanced propofol sedation in patients undergoing EUS-FNA: a pilot study to assess feasibility and safety. Diagn Ther Endosc. 2011; 2011:542159.7. Yusoff IF, Raymond G, Sahai AV. Endoscopist administered propofol for upper-GI EUS is safe and effective: a prospective study in 500 patients. Gastrointest Endosc. 2004; 60:356–360.8. Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology. 1998; 89:980–1002.9. Glass PS, Bloom M, Kearse L, et al. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology. 1997; 86:836–847.10. Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970; 49:924–934.11. Lovett P, Gómez V, Hodge DO, et al. Propofol versus midazolam/fentanyl sedation for colonoscopy in the elderly patient population. J Perianesth Nurs. 2017; 32:210–214.12. Schmitz A, Weiss M, Kellenberger C, et al. Sedation for magnetic resonance imaging using propofol with or without ketamine at induction in pediatrics: a prospective randomized double-blinded study. Paediatr Anaesth. 2018; 28:264–274.13. Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008; 358:1097–1108.14. O’Connor MF, Daves SM, Tung A, et al. BIS monitoring to prevent awareness during general anesthesia. Anesthesiology. 2001; 94:520–522.15. Gan TJ, Glass PS, Windsor A, et al. Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology. 1997; 87:808–815.16. Choi WJ, Kim YH. How do you use bispectral index effectively for preventing re-awareness during general anesthesia? Korean J Anesthesiol. 2012; 62:1–2.17. Sandler NA, Hodges J, Sabino M. Assessment of recovery in patients undergoing intravenous conscious sedation using bispectral analysis. J Oral Maxillofac Surg. 2001; 59:603–611.18. Jang SY, Park HG, Jung MK, et al. Bispectral index monitoring as an adjunct to nurse-administered combined sedation during endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012; 18:6284–6289.19. von Delius S, Salletmaier H, Meining A, et al. Bispectral index monitoring of midazolam and propofol sedation during endoscopic retrograde cholangiopancreatography: a randomized clinical trial (the EndoBIS study). Endoscopy. 2012; 44:258–264.20. Paspatis GA, Chainaki I, Manolaraki MM, et al. Efficacy of bispectral index monitoring as an adjunct to propofol deep sedation for ERCP: a randomized controlled trial. Endoscopy. 2009; 41:1046–1051.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bispectral Index Monitoring during Anesthesiologist-Directed Propofol and Remifentanil Sedation for Endoscopic Submucosal Dissection: A Prospective Randomized Controlled Trial
- Evaluation of Auditory Evoked Potential and Bispectral Index in Patient-Controlled Sedation with Propofol
- Titration of Effect Site Concentration of Propofol for Conscious Sedation in Elderly Patients
- The Influences of Clonidine Premedication on the Bispectral Index and Hemodynamics during the Induction of Anesthesia and Endotracheal Intubation with Propofol
- Sedation for routine gastrointestinal endoscopic procedures: a review on efficacy, safety, efficiency, cost and satisfaction