Child Kidney Dis.
2022 Jun;26(1):63-67. 10.3339/ckd.22.027.
Idiopathic infantile hypercalcemia with severe nephrocalcinosis, associated with CYP24A1 mutations: a case report
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- 3Kidney Research Institute, Medical Research Center, Seoul National University College of Medicine, Seoul, Republic of Korea
- 4Wide River Institute of Immunology, Seoul National University, Hongcheon, Republic of Korea
- KMID: 2531937
- DOI: http://doi.org/10.3339/ckd.22.027
Abstract
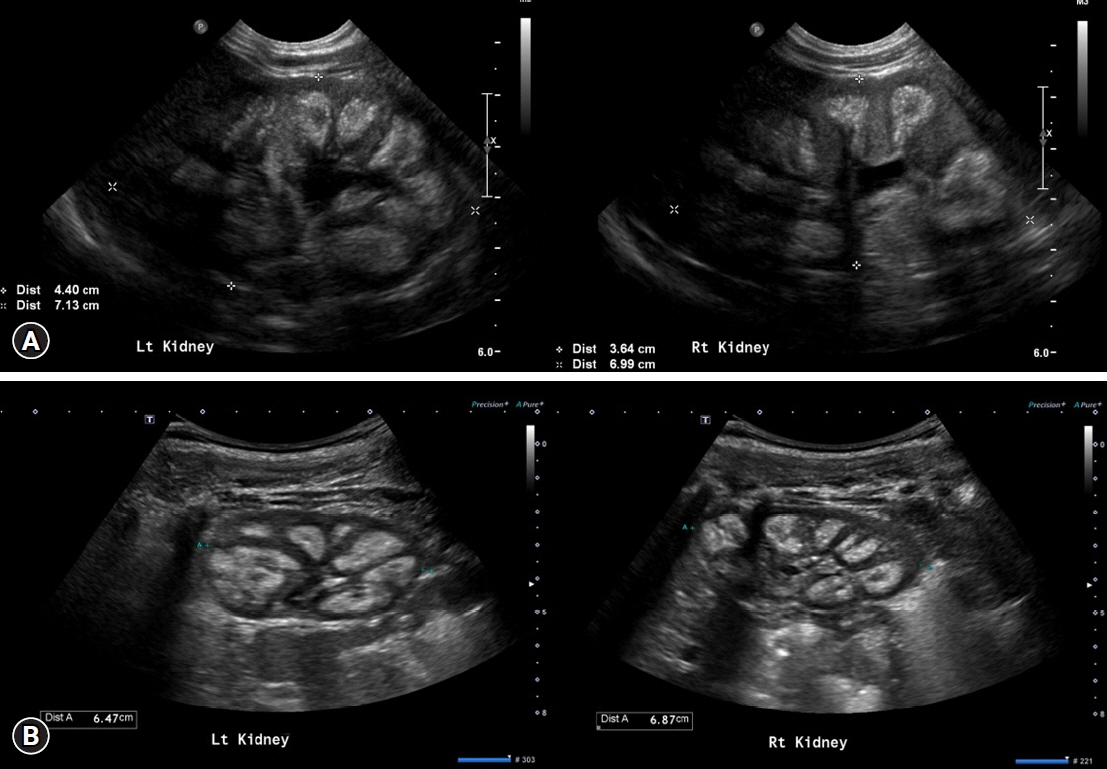
- Nephrocalcinosis often occurs in infants and is caused by excessive calcium or vitamin D supplementation, neonatal primary hyperparathyroidism, and genetic disorders. Idiopathic infantile hypercalcemia (IIH), a rare cause of nephrocalcinosis, results from genetic defects in CYP24A1 or SLC34A1. Mutations in CYP24A1, which encodes 25-hydroxyvitamin D 24-hydroxylase, disrupt active vitamin D degradation. IIH clinically manifests as failure to thrive and hypercalcemia within the first year of life and usually remits spontaneously. Herein, we present a case of IIH wih CYP24A1 mutations. An 11-month-old girl visited our hospital with incidental hypercalcemia. She showed failure to thrive, and her oral intake had decreased over time since the age of 6 months. Her initial serum parathyroid hormone level was low, 25-OH vitamin D and 1,25-OH vitamin D levels were normal, and renal ultrasonography showed bilateral nephrocalcinosis. Whole-exome sequencing revealed compound heterozygous variants in CYP24A1 (NM_000782.4:c.376C>T [p.Pro126Ser] and c.1310C>A [p.Pro437His]). Although her hypercalcemia and poor oral intake spontaneously resolved in approximately 8 months, we suggested that her nephrocalcinosis and renal function be regularly checked in consideration of potential asymptomatic renal damage. Hypercalcemia caused by IIH should be suspected in infants with severe nephrocalcinosis, especially when presenting with failure to thrive.
Figure
Reference
-
References
1. Vaidya SR, Yarrarapu SNS, Aeddula NR. Nephrocalcinosis [Internet]. Treasure Island: StatPearls Publishing;2021. Aug. [cited 2022 Apr 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537205/.2. Ronnefarth G, Misselwitz J; Members of the Arbeitsgemeinschaft für pädiatrische Nephrologie. Nephrocalcinosis in children: a retrospective survey. Pediatr Nephrol. 2000; 14:1016–21.
Article3. Habbig S, Beck BB, Hoppe B. Nephrocalcinosis and urolithiasis in children. Kidney Int. 2011; 80:1278–91.
Article4. Hoppe B, Kemper MJ. Diagnostic examination of the child with urolithiasis or nephrocalcinosis. Pediatr Nephrol. 2010; 25:403–13.
Article5. Lietman SA, Germain-Lee EL, Levine MA. Hypercalcemia in children and adolescents. Curr Opin Pediatr. 2010; 22:508–15.
Article6. De Paolis E, Scaglione GL, De Bonis M, Minucci A, Capoluongo E. CYP24A1 and SLC34A1 genetic defects associated with idiopathic infantile hypercalcemia: from genotype to phenotype. Clin Chem Lab Med. 2019; 57:1650–67.7. Schlingmann KP, Kaufmann M, Weber S, Irwin A, Goos C, John U, et al. Mutations in CYP24A1 and idiopathic infantile hypercalcemia. N Engl J Med. 2011; 365:410–21.
Article8. Gil A, Plaza-Diaz J, Mesa MD. Vitamin D: classic and novel actions. Ann Nutr Metab. 2018; 72:87–95.
Article9. Marks BE, Doyle DA. Idiopathic infantile hypercalcemia: case report and review of the literature. J Pediatr Endocrinol Metab. 2016; 29:127–32.
Article10. Janiec A, Halat-Wolska P, Obrycki L, Ciara E, Wojcik M, Pludowski P, et al. Long-term outcome of the survivors of infantile hypercalcaemia with CYP24A1 and SLC34A1 mutations. Nephrol Dial Transplant. 2021; 36:1484–92.11. Vogiatzi MG, Jacobson-Dickman E, DeBoer MD; Drugs, and Therapeutics Committee of The Pediatric Endocrine Society. Vitamin D supplementation and risk of toxicity in pediatrics: a review of current literature. J Clin Endocrinol Metab. 2014; 99:1132–41.
Article12. Kang SJ, Lee R, Kim HS. Infantile hypercalcemia with novel compound heterozygous mutation in SLC34A1 encoding renal sodium-phosphate cotransporter 2a: a case report. Ann Pediatr Endocrinol Metab. 2019; 24:64–7.
Article13. Lee GM, Moon JE, Kim HA, Lee SJ, Ko CW. A novel variant of SLC34A1 gene in an infant with idiopathic infantile hypercalcemia. ESPE Abstr. 2018; 89:P2-047.14. Barnett ML. Hypercalcemia. Semin Oncol Nurs. 1999; 15:190–201.
Article15. Moza D, Dasgupta K, Daskalopoulou S. Hypercalcemia and upper GI symptoms. Can J Gen Int Med. 2018; 13:51–2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Infantile hypercalcemia with novel compound heterozygous mutation in SLC34A1 encoding renal sodium-phosphate cotransporter 2a: a case report
- A Case of Idiopathic Infantile Hypercalcemia Treated with Intravenous Pamidronate Infusion
- Subcutaneous Fat Necrosis of the Newborn: A Case Report
- A case of parathyroid carcinoma with acute renal failure and microscopic nephrocalcinosis
- A Case of Severe Hypercalcemia Causing Acute Kidney Injury: An Unusual Presentation of Acute Lymphoblastic Leukemia