Child Kidney Dis.
2022 Jun;26(1):18-24. 10.3339/ckd.22.028.
Renal involvement in pediatric rheumatologic diseases
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea
- KMID: 2531930
- DOI: http://doi.org/10.3339/ckd.22.028
Abstract
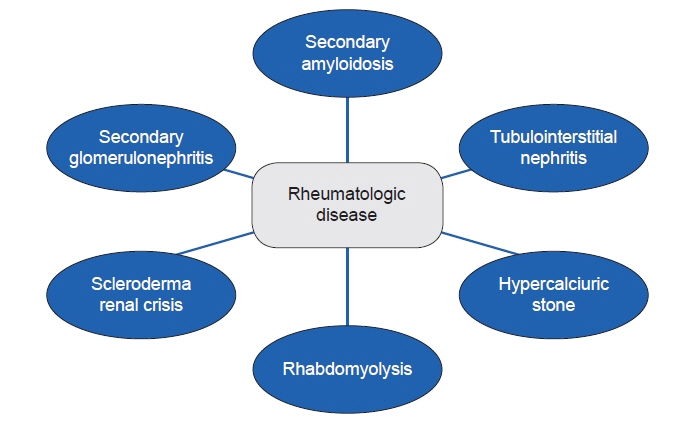
- Pediatric rheumatologic diseases are rare systemic diseases that can involve various organs, including the kidneys. Each rheumatologic disease can exhibit characteristic renal involvement, which requires proper treatment and diagnosis. In this review, we discuss renal involvement in classic rheumatologic diseases, including juvenile idiopathic arthritis, Sjogren's syndrome, systemic sclerosis, and juvenile dermatomyositis. Reviews addressing lupus nephritis and antineutrophil cytoplasmic antibody-associated renal disease are complex and tend to cover a wide array of topics, and thus were excluded from this review.
Keyword
Figure
Reference
-
References
1. Schaller JG. The history of pediatric rheumatology. Pediatr Res. 2005; 58:997–1007.
Article2. Srinivasalu H, Riebschleger M. Medical education in pediatric rheumatology: unique challenges and opportunities. Clin Rheumatol. 2020; 39:643–50.
Article3. Husserl FE, Shuler SE. Gold nephropathy in juvenile rheumatoid arthritis. Am J Dis Child. 1979; 133:50–2.
Article4. Rovenska E, Kapeller K, Rossmann P. Gold nephropathy in rheumatoid arthritis and in juvenile chronic arthritis. Czech Med. 1979; 2:125–33.5. Koseki Y, Terai C, Moriguchi M, Uesato M, Kamatani N. A prospective study of renal disease in patients with early rheumatoid arthritis. Ann Rheum Dis. 2001; 60:327–31.
Article6. Deschenes G, Prieur AM, Hayem F, Broyer M, Gubler MC. Renal amyloidosis in juvenile chronic arthritis: evolution after chlorambucil treatment. Pediatr Nephrol. 1990; 4:463–9.
Article7. Bilginer Y, Akpolat T, Ozen S. Renal amyloidosis in children. Pediatr Nephrol. 2011; 26:1215–27.
Article8. Immonen K, Savolainen A, Kautiainen H, Hakala M. Longterm outcome of amyloidosis associated with juvenile idiopathic arthritis. J Rheumatol. 2008; 35:907–12.9. David J, Vouyiouka O, Ansell BM, Hall A, Woo P. Amyloidosis in juvenile chronic arthritis: a morbidity and mortality study. Clin Exp Rheumatol. 1993; 11:85–90.10. Schneider R, Passo MH. Juvenile rheumatoid arthritis. Rheum Dis Clin North Am. 2002; 28:503–30.
Article11. Dhillon V, Woo P, Isenberg D. Amyloidosis in the rheumatic diseases. Ann Rheum Dis. 1989; 48:696–701.
Article12. Chantarogh S, Vilaiyuk S, Tim-Aroon T, Worawichawong S. Clinical improvement of renal amyloidosis in a patient with systemic-onset juvenile idiopathic arthritis who received tocilizumab treatment: a case report and literature review. BMC Nephrol. 2017; 18:159.
Article13. Gupta A, Bagri NK, Tripathy SK, Barwad A, Phulware RH, Hari P. Successful use of tocilizumab in amyloidosis secondary to systemic juvenile idiopathic arthritis. Rheumatol Int. 2020; 40:153–9.
Article14. Okuda Y, Takasugi K. Successful use of a humanized anti-interleukin-6 receptor antibody, tocilizumab, to treat amyloid A amyloidosis complicating juvenile idiopathic arthritis. Arthritis Rheum. 2006; 54:2997–3000.
Article15. Mielants H, Van den Bosch F. Extra-articular manifestations. Clin Exp Rheumatol. 2009; 27(4 Suppl 55):S56–61.16. Adu D, Berisa F, Howie AJ, Emery P, Bacon PA, McConkey B, et al. Glomerulonephritis in rheumatoid arthritis. Br J Rheumatol. 1993; 32:1008–11.
Article17. Bandin F, Merhenberger M, Modesto A, Brochard K, Decramer S. Steroid-responsive nephrotic syndrome in a child with juvenile idiopathic arthritis. Pediatr Nephrol. 2008; 23:651–4.
Article18. Breedveld FC, Valentijn RM, Westedt ML, Weening JJ. Rapidly progressive glomerulonephritis with glomerular crescent formation in rheumatoid arthritis. Clin Rheumatol. 1985; 4:353–9.
Article19. Helin HJ, Korpela MM, Mustonen JT, Pasternack AI. Renal biopsy findings and clinicopathologic correlations in rheumatoid arthritis. Arthritis Rheum. 1995; 38:242–7.
Article20. Gedalia A, Mendez EA, Craver R, Vehaskari M, Espinoza LR. Renal involvement in juvenile rheumatoid arthritis: report of two cases. Clin Rheumatol. 2001; 20:153–6.
Article21. Varma S. Juvenile rheumatoid arthritis with focal segmental glomerulosclerosis: a rare association. Pediatr Nephrol. 2010; 25:2189–90.
Article22. Kari JA, Bamashmous H, Mahan JD. Steroid-sensitive nephrotic syndrome and juvenile idiopathic arthritis. Pediatr Nephrol. 2002; 17:975–6.
Article23. Lipnick RN, Tsokos GC, Magilavy DB. Immune abnormalities in the pathogenesis of juvenile rheumatoid arthritis. Rheum Dis Clin North Am. 1991; 17:843–57.
Article24. Foster BJ, Duffy CM, Sharma AK. Systemic juvenile rheumatoid arthritis complicated by two different renal lesions. Pediatr Nephrol. 1998; 12:113–6.
Article25. Francois H, Mariette X. Renal involvement in primary Sjogren syndrome. Nat Rev Nephrol. 2016; 12:82–93.26. Pessler F, Emery H, Dai L, Wu YM, Monash B, Cron RQ, et al. The spectrum of renal tubular acidosis in paediatric Sjogren syndrome. Rheumatology (Oxford). 2006; 45:85–91.
Article27. Brito-Zeron P, Baldini C, Bootsma H, Bowman SJ, Jonsson R, Mariette X, et al. Sjogren syndrome. Nat Rev Dis Primers. 2016; 2:16047.28. Tucker L, Ciurtin C. Sjogren syndrome and immunoglobulin-G4 disease. In : Petty RE, Laxer RM, Lindsley CB, Wedderburn LR, Mellins ED, Fuhlbrigge RC, editors. Textbook of pediatric rheumatology. 8th ed. Philadelphia: Elsevier;2021. p. 417–26.29. Zhao J, Chen Q, Zhu Y, Zhao M, Liu J, Zhang Z, et al. Nephrological disorders and neurological involvement in pediatric primary Sjogren syndrome: a case report and review of literature. Pediatr Rheumatol Online J. 2020; 18:39.
Article30. Aiyegbusi O, McGregor L, McGeoch L, Kipgen D, Geddes CC, Stevens KI. Renal disease in primary Sjogren’s syndrome. Rheumatol Ther. 2021; 8:63–80.31. Katsifis GE, Rekka S, Moutsopoulos NM, Pillemer S, Wahl SM. Systemic and local interleukin-17 and linked cytokines associated with Sjogren’s syndrome immunopathogenesis. Am J Pathol. 2009; 175:1167–77.32. Goules A, Geetha D, Arend LJ, Baer AN. Renal involvement in primary Sjogren’s syndrome: natural history and treatment outcome. Clin Exp Rheumatol. 2019; 37 Suppl 118:123–32.33. Gu X, Su Z, Chen M, Xu Y, Wang Y. Acquired Gitelman syndrome in a primary Sjogren syndrome patient with a SLC12A3 heterozygous mutation: a case report and literature review. Nephrology (Carlton). 2017; 22:652–5.34. Ren H, Wang WM, Chen XN, Zhang W, Pan XX, Wang XL, et al. Renal involvement and followup of 130 patients with primary Sjogren’s syndrome. J Rheumatol. 2008; 35:278–84.35. Cohen EP, Bastani B, Cohen MR, Kolner S, Hemken P, Gluck SL. Absence of H(+)-ATPase in cortical collecting tubules of a patient with Sjogren’s syndrome and distal renal tubular acidosis. J Am Soc Nephrol. 1992; 3:264–71.
Article36. Pedro-Botet J, Tomas S, Soriano JC, Coll J. Primary Sjogren’s syndrome associated with Bartter’s syndrome. Clin Exp Rheumatol. 1991; 9:210–2.37. Oliva-Damaso N, Oliva-Damaso E, Payan J. Acute and chronic tubulointerstitial nephritis of rheumatic causes. Rheum Dis Clin North Am. 2018; 44:619–33.
Article38. Jung SK, Park KH, Yim HE, Yoo KH, Hong YS, Lee JW, et al. Primary Sjogren’s syndrome with mesangial proliferative glomerulonephritis and IgA deposits in a child. Pediatr Nephrol. 2010; 25:567–8.
Article39. Yoshida K, Suzuki J, Kume K, Suzuki S, Isome M, Kato K, et al. Sjogren’s syndrome with membranous glomerulonephritis detected by urine screening of schoolchildren. Acta Paediatr Jpn. 1996; 38:533–6.40. Kagan M, Bervina N, Vorobyeva O, Wouters C, Levtchenko E. Pauci-immune crescentic glomerulonephritis complicating Sjogren’s syndrome in a 12-year-old girl. Pediatr Nephrol. 2011; 26:991–2.
Article41. Dorfman RF, Berry GJ. Kikuchi’s histiocytic necrotizing lymphadenitis: an analysis of 108 cases with emphasis on differential diagnosis. Semin Diagn Pathol. 1988; 5:329–45.42. Lin CY, Wu CH, Chen HA, Hsu CY, Wang LH, Su YJ. Long-term renal prognosis among patients with primary Sjogren’s syndrome and renal involvement: a nationwide matched cohort study. J Autoimmun. 2020; 113:102483.43. Fragoulis GE, Zampeli E, Moutsopoulos HM. IgG4-related sialadenitis and Sjogren’s syndrome. Oral Dis. 2017; 23:152–6.44. Boffa JJ, Esteve E, Buob D. Renal involvement in IgG4-related disease. Presse Med. 2020; 49:104017.
Article45. Johnson JS, Saltzman AF, Treece AL, Cost NG. A case of IgG4-related renal pseudotumor in a child with history of Wilms tumor. Urol Case Rep. 2018; 21:107–9.
Article46. Karim F, Loeffen J, Bramer W, Westenberg L, Verdijk R, van Hagen M, et al. IgG4-related disease: a systematic review of this unrecognized disease in pediatrics. Pediatr Rheumatol Online J. 2016; 14:18.
Article47. Torok KS, Stevens AM. Juvenile systemic sclerosis. In : Petty RE, Laxer RM, Lindsley CB, Wedderburn LR, Mellins ED, Fuhlbrigge RC, editors. Textbook of pediatric rheumatology. 8th ed. Philadelphia: Elsevier;2021. p. 377–401.48. Chrabaszcz M, Malyszko J, Sikora M, Alda-Malicka R, Stochmal A, Matuszkiewicz-Rowinska J, et al. Renal involvement in systemic sclerosis: an update. Kidney Blood Press Res. 2020; 45:532–48.
Article49. Denton CP, Khanna D. Systemic sclerosis. Lancet. 2017; 390:1685–99.
Article50. Herrick AL. Vascular function in systemic sclerosis. Curr Opin Rheumatol. 2000; 12:527–33.
Article51. Steen VD. Scleroderma renal crisis. Rheum Dis Clin North Am. 2003; 29:315–33.
Article52. Pamuk GE, Pamuk ON, Altiparmak MR, Tanverdi M, Uygun N, Yurdakul S. Secondary amyloidosis in progressive systemic sclerosis. Clin Rheumatol. 2001; 20:285–7.
Article53. Papadopoulou C, McCann LJ. The vasculopathy of juvenile dermatomyositis. Front Pediatr. 2018; 6:284.
Article54. Sangeetha G, Dhanabal D, Mouttou Prebagarane S, Janarthanan M. Juvenile dermatomyositis: a case of delayed recognition with unusual complication of nephrocalcinosis. BMJ Case Rep. 2021; 14:e241152.
Article55. Couvrat-Desvergnes G, Masseau A, Benveniste O, Bruel A, Hervier B, Mussini JM, et al. The spectrum of renal involvement in patients with inflammatory myopathies. Medicine (Baltimore). 2014; 93:33–41.
Article56. Mantoo MR, Tripathy SK, Phulware RH, Bagri NK, Hari P, Barwad A. Juvenile dermatomyositis with IgA nephropathy: case-based review. Rheumatol Int. 2019; 39:577–81.
Article57. Wyatt RJ, Julian BA. IgA nephropathy. N Engl J Med. 2013; 368:2402–14.
Article58. Stahl JL, Rutledge JC, Gordillo R. The unusual suspects: a curious case of acute kidney injury: answers. Pediatr Nephrol. 2019; 34:1213–5.
Article59. Minoia F, Tibaldi J, Muratore V, Gallizzi R, Bracaglia C, Arduini A, et al. Thrombotic microangiopathy associated with macrophage activation syndrome: a multinational study of 23 patients. J Pediatr. 2021; 235:196–202.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Renal Involvement in Rheumatic Diseases
- Behcet's disease: a rheumatologic perspective
- The Systemic Rheumatologic Disease and Neuromyelitis Optica
- Impact of Rheumatologic Consultations on Detecting Interstitial Lung Disease Associated with Connective Tissue Disease
- The Effect of Steroid on Renal Involvement in Henoch-Schonlein Purpura