Arch Hand Microsurg.
2022 Jun;27(2):125-133. 10.12790/ahm.21.0148.
Comparative finite element analysis of an osseointegration system in transradial amputation: a proposal of a new design for osseointegration
- Affiliations
-
- 1Department of Orthopedic Surgery, Hanyang University Guri Hospital, Guri, Korea
- 2Machine Dynamics Laboratory, Department of Mechanical Engineering, Hanyang University, Ansan, Korea
- 3Department of Orthopedic Surgery, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2531918
- DOI: http://doi.org/10.12790/ahm.21.0148
Abstract
- Purpose
Conventional osseointegration systems have been applied in patients requiring transhumeral or transfemoral amputation. However, the application of these systems to transradial amputation is limited by the small diameter of the radius and ulna. Our study compared the biomechanical stability of a novel osseointegration system with that of a conventional system used in transradial amputation through an analysis of finite element (FE) models.
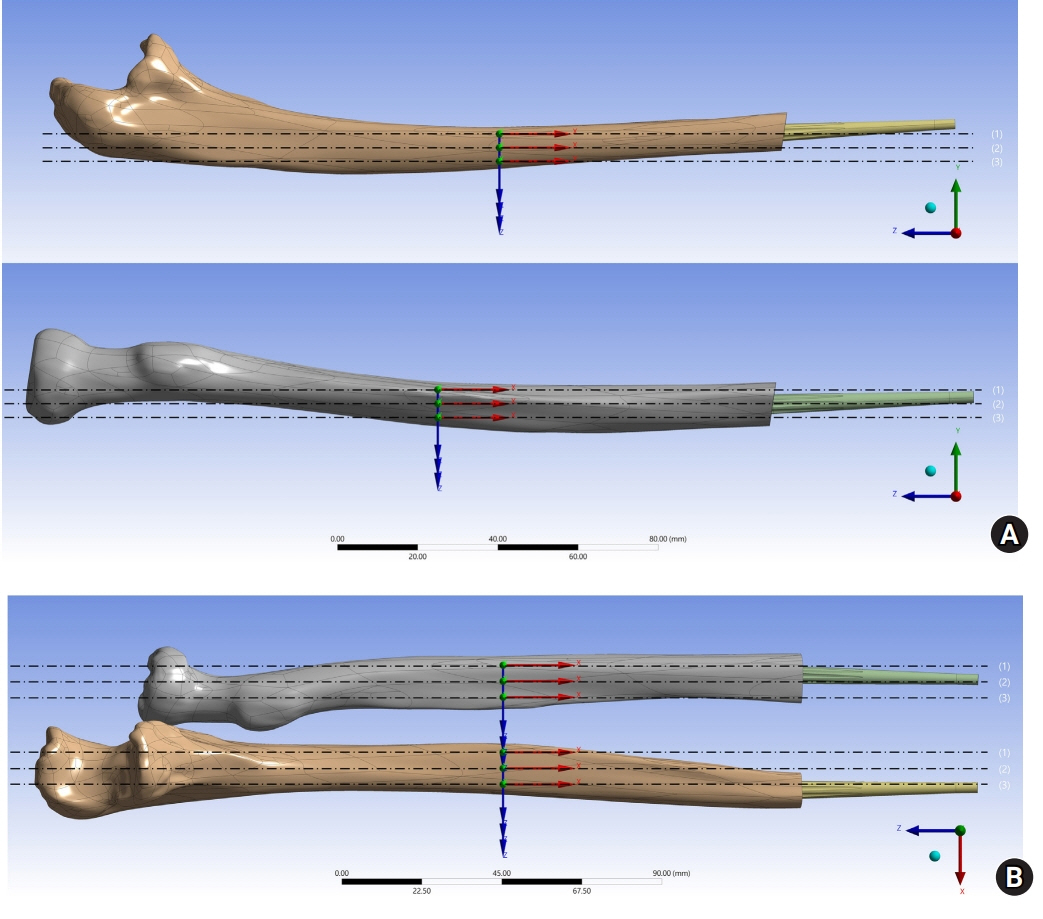
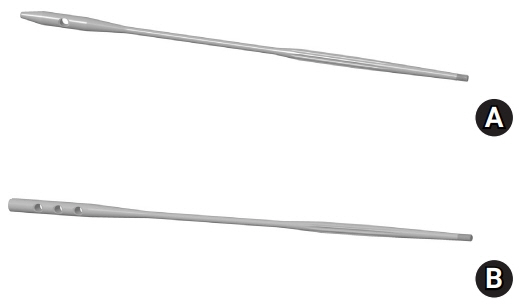
Methods
We established three-dimensional FE models of transradial amputations, which were osseointegrated with both the novel and conventional systems. External loads were applied to the FE models with compressive force and tensile force along the long axis, horizontal shear force, and vertical shear force. The maximum equivalent stress (MES) and the distribution of stress through the radius and ulna were evaluated.
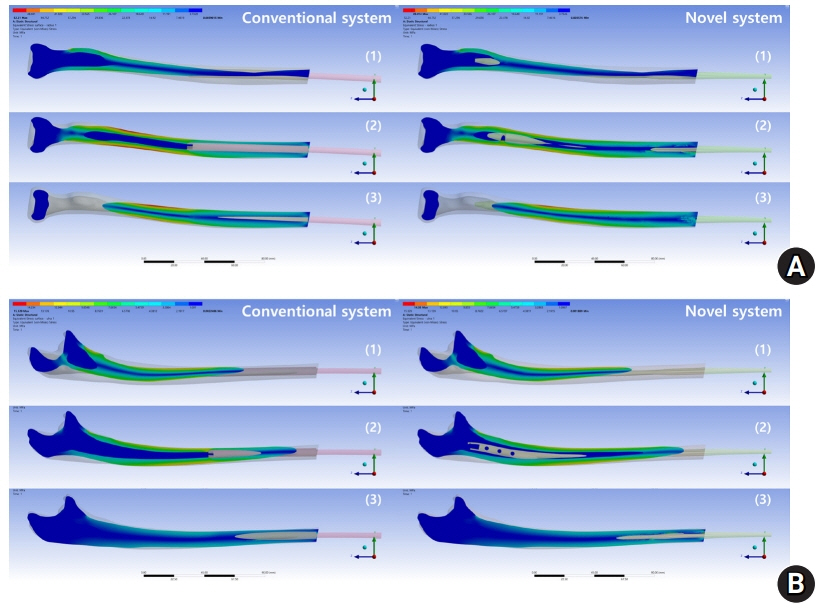
Results
The MES of the radius and ulna was higher in the conventional system when compressive, tensile, and vertical shear forces were applied. However, when a horizontal shear force was applied, the opposite result was found. The distribution of stress was more effective in the novel system.
Conclusion
Three-dimensional FE modeling showed that the novel system enabled a lower stress level and a more even distribution of stress for osseointegration in transradial amputation.
Figure
Reference
-
References
1. Amornvit P, Rokaya D, Keawcharoen K, Thongpulsawasdi N. Stress distribution in implant retained finger prosthesis: a finite element study. J Clin Diagn Res. 2013; 7:2851–4.
Article2. Maduri P, Akhondi H. Upper limb amputation [updated 2021 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2022. [cited 2021 Dec 3]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540962/.3. Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008; 89:422–9.
Article4. Atroshi I, Rosberg HE. Epidemiology of amputations and severe injuries of the hand. Hand Clin. 2001; 17:343–50.
Article5. Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002; 95:875–83.
Article6. Lee G, Kim SJ, Ha JH, Lee CH, Choi YJ, Lee KH. Residual rotation of forearm amputation: cadaveric study. BMC Musculoskelet Disord. 2020; 21:40.
Article7. Grisez BT, Hanselman AE, Boukhemis KW, Lalli TA, Lindsey BA. Osseointegrated transcutaneous device for amputees: a pilot large animal model. Adv Orthop. 2018; 2018:4625967.
Article8. Tomaszewski PK, van Diest M, Bulstra SK, Verdonschot N, Verkerke GJ. Numerical analysis of an osseointegrated prosthesis fixation with reduced bone failure risk and periprosthetic bone loss. J Biomech. 2012; 45:1875–80.
Article9. Barth J, Garret J, Boutsiadis A, et al. Is global humeral head offset related to intramedullary canal width?: a computer tomography morphometric study. J Exp Orthop. 2018; 5:35.
Article10. Hopf JC, Jähnig A, Jorg T, Westphal RS, Wagner D, Rommens PM. Computer tomographic analysis of anatomic characteristics of the ulna: essential parameters for preshaped implants. PLoS One. 2020; 15:e0232988.11. Pierrie SN, Gaston RG, Loeffler BJ. Current concepts in upper-extremity amputation. J Hand Surg Am. 2018; 43:657–67.
Article12. Kaku N, Tanaka A, Tagomori H, Tsumura H. Finite element analysis of stress distribution in flat and elevated-rim polyethylene acetabular liners. Clin Orthop Surg. 2020; 12:291–7.
Article13. Liu HC, Jiang JS, Lin CL. Biomechanical investigation of a novel hybrid dorsal double plating for distal radius fractures by integrating topology optimization and finite element analysis. Injury. 2020; 51:1271–80.
Article14. Engelke K, Libanati C, Fuerst T, Zysset P, Genant HK. Advanced CT based in vivo methods for the assessment of bone density, structure, and strength. Curr Osteoporos Rep. 2013; 11:246–55.
Article15. Santoni BG, Aira JR, Diaz MA, Kyle Stoops T, Simon P. Radiographic evaluation of acute distal radius fracture stability: a comparative cadaveric study between a thermo-formable bracing system and traditional fiberglass casting. Clin Biomech (Bristol, Avon). 2017; 47:20–6.
Article16. Jönsson S, Caine-Winterberger K, Brånemark R. Osseointegration amputation prostheses on the upper limbs: methods, prosthetics and rehabilitation. Prosthet Orthot Int. 2011; 35:190–200.17. Dudek NL, Marks MB, Marshall SC, Chardon JP. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005; 86:659–63.
Article18. Meulenbelt HE, Geertzen JH, Jonkman MF, Dijkstra PU. Skin problems of the stump in lower limb amputees: 1. A clinical study. Acta Derm Venereol. 2011; 91:173–7.
Article19. Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999; 9:207–31.
Article20. Nebergall A, Bragdon C, Antonellis A, Kärrholm J, Brånemark R, Malchau H. Stable fixation of an osseointegated implant system for above-the-knee amputees: titel RSA and radiographic evaluation of migration and bone remodeling in 55 cases. Acta Orthop. 2012; 83:121–8.21. Tillander J, Hagberg K, Hagberg L, Brånemark R. Osseointegrated titanium implants for limb prostheses attachments: infectious complications. Clin Orthop Relat Res. 2010; 468:2781–8.
Article22. Ding X, Liao SH, Zhu XH, Zhang XH, Zhang L. Effect of diameter and length on stress distribution of the alveolar crest around immediate loading implants. Clin Implant Dent Relat Res. 2009; 11:279–87.
Article23. Baggi L, Cappelloni I, Di Girolamo M, Maceri F, Vairo G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: a three-dimensional finite element analysis. J Prosthet Dent. 2008; 100:422–31.
Article24. Firl M, Wünsch L. Measurement of bowing of the radius. J Bone Joint Surg Br. 2004; 86:1047–9.
Article25. Xiaobin LP, Zelong L. Stress concentration factors due to typical geometric discontinuities for shaft design by numerical simulation. In : Paper presented at 2013 ASEE Annual Conference & Exposition; 2013 Jun 23-26; Atlanta, GA. Atlanta, GA. ASEE. 2013.
Article26. Stenlund P, Trobos M, Lausmaa J, Brånemark R, Thomsen P, Palmquist A. Effect of load on the bone around bone-anchored amputation prostheses. J Orthop Res. 2017; 35:1113–22.
Article27. Al Muderis M, Khemka A, Lord SJ, Van de Meent H, Frölke JP. Safety of osseointegrated implants for transfemoral amputees: a two-center prospective cohort study. J Bone Joint Surg Am. 2016; 98:900–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stress dissipation characteristics of four implant thread designs evaluated by 3D finite element modeling
- Finite element approach to investigate the influence of the design configuration of the ITI solid implant on the bone stresses during the osseointegration process
- Effect of bone-implant contact pattern on bone strain distribution: finite element method study
- A study on the finite element analysis and bone formation of the apically expandable implant
- Three-dimensional finite element analysis according to the insertion depth of an immediately loaded implant in the anterior maxilla