J Cerebrovasc Endovasc Neurosurg.
2022 Jun;24(2):113-120. 10.7461/jcen.2021.E2021.08.003.
Adrenocorticotropic hormone and β-endorphin concentration as a prognostic factor in patients with subarachnoid hemorrhage due to aneurysmal rupture
- Affiliations
-
- 1Department of neurosurgery Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2531653
- DOI: http://doi.org/10.7461/jcen.2021.E2021.08.003
Abstract
Objective
Adrenocorticotropic hormone (ACTH) and β-endorphin are pituitary neuro-peptides released by acute stress. We determined why the prognosis of patients with subarachnoid hemorrhages (SAH) due to aneurysmal rupture is not always dependent on the Hunt–Hess grading system (HHS) and delta-National Institutes of Health Stroke Scale (NIHSS), while studying endogenous neuropeptides, including ACTH and β-endorphin.
Methods
We analyzed blood samples collected from patients with SAH (SAH group; n=37) and those with unruptured intracranial aneurysms (control group; n=37). Blood sampling was performed before any procedure or chemical agents administration. The results of ACTH and β-endorphin measurements were compared using the delta-NIHSS and HHS. The data were analyzed using descriptive statistics, independent samples t-tests, and Pearson’s correlations.
Results
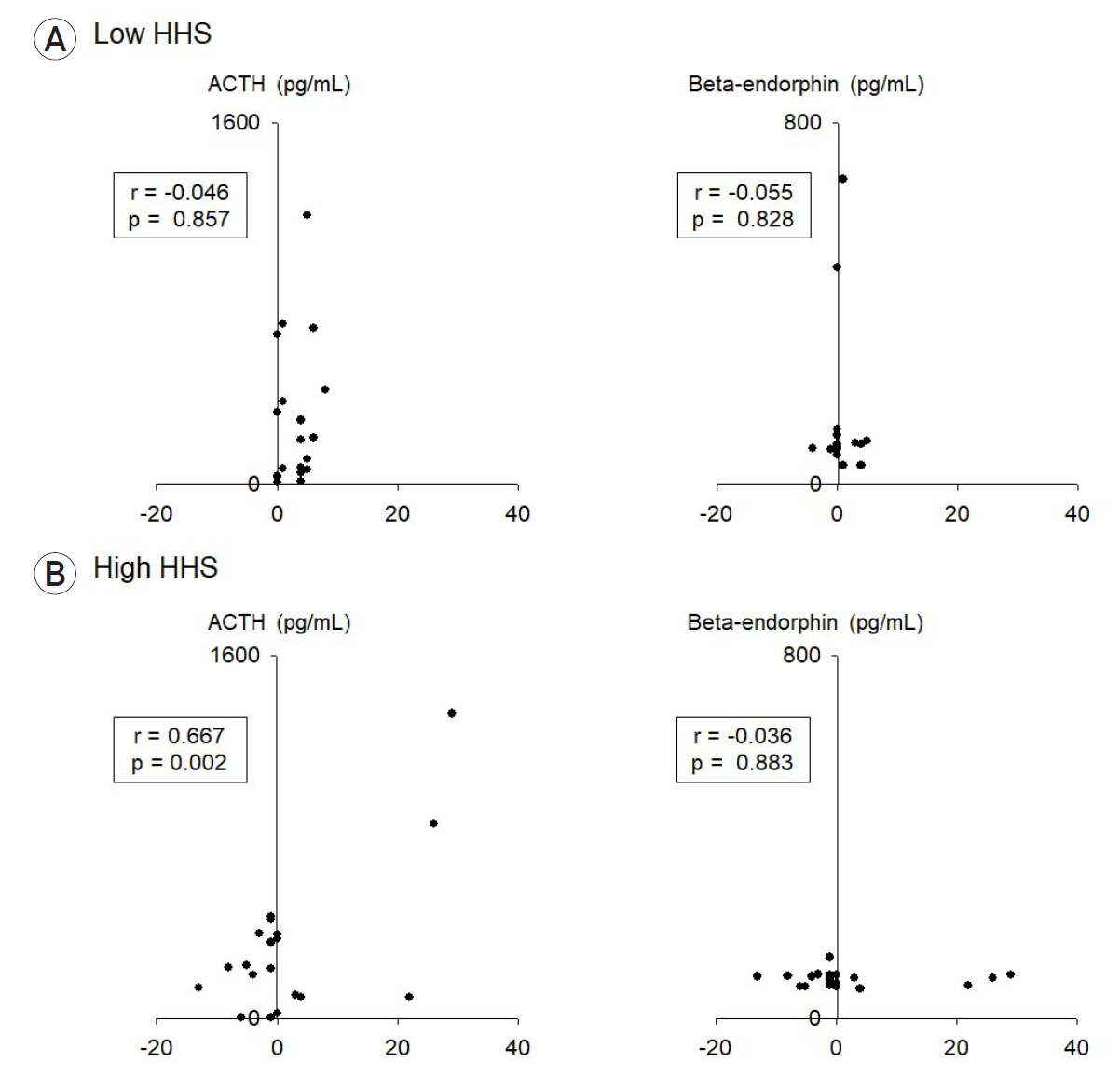
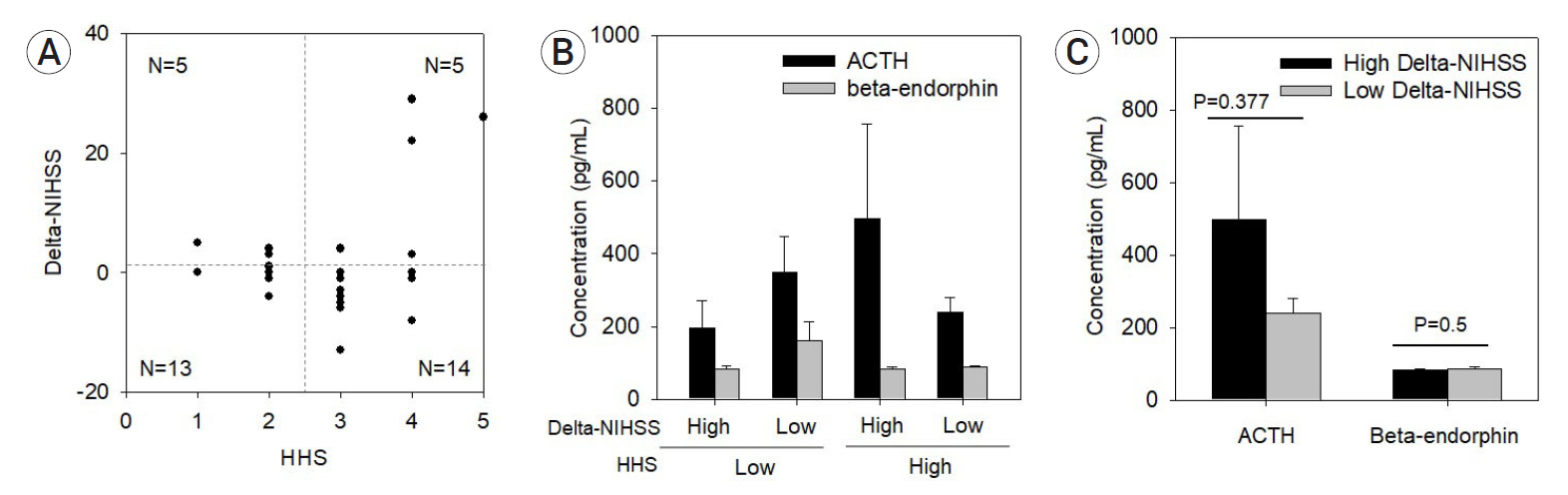
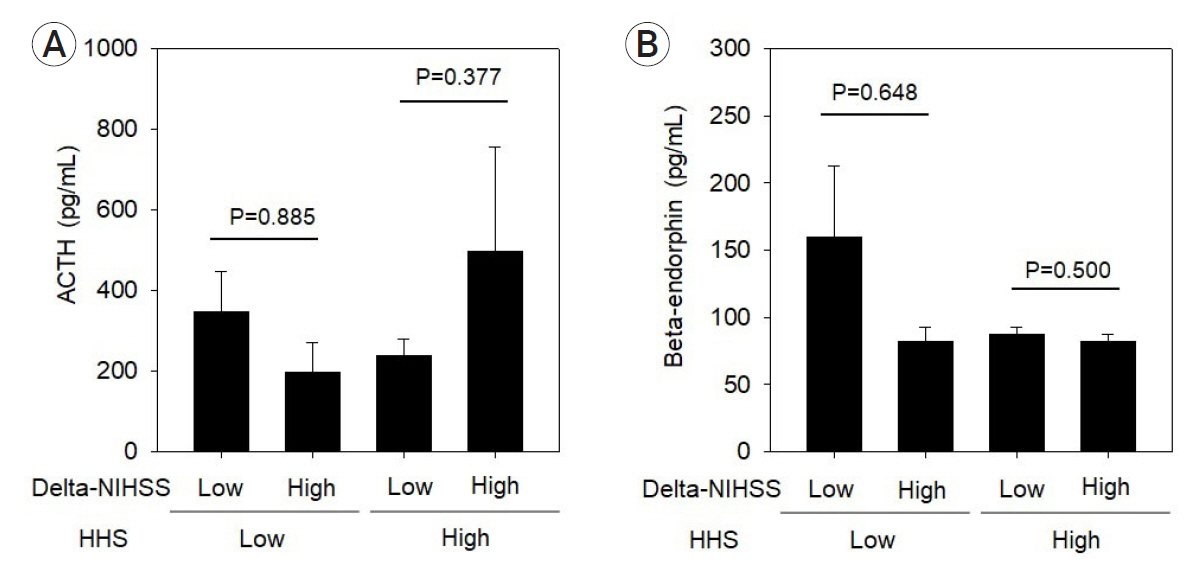
Of the 18 patients with low-grade HHS, 13 had low delta-NIHSS and five showed high delta-NIHSS. Of the 19 patients with high-grade HHS, the delta-NIHSS was ≥14 in the other five patients. ACTH concentration was high (497.3 pg/mL) in five patients with high-grade HHS and high delta-NIHSS. β-endorphin concentration was high (159.7 pg/mL) in 13 patients with low-grade HHS and low delta-NIHSS.
Conclusions
High ACTH levels in patients with massive bleeding and poor neurological status suggests increasing ACTH secretion in response to bleeding stress, which may aggravate neurological status. Contrary to ACTH, high β-endorphin levels in patients with low-grade HHS implied the involvement of additional factors in predicting fair outcomes related to low delta-NIHSS. These results may provide insight into the varying prognostic potential of HHS in SAH patients.
Figure
Reference
-
1. Bendel S, Koivisto T, Ruokonen E, Rinne J, Romppanen J, Vauhkonen I, et al. Pituitary-adrenal function in patients with acute subarachnoid haemorrhage: a prospective cohort study. 2008; Oct. 12(5):R126.
Article2. Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980; Jan. 6(1):1–9.
Article3. Henryk S, Jośko J, Jedrzejowska-Szypułka H, Jarzab B, Döhler KD. Corticotropin releasing hormone (CRH) increases beta-endorphin (beta-end like) concentration in cerebrospinal fluid of rats with vasospasm following subarachnoid hemorrhage. J Physiol Pharmacol. 1999; Sep. 50(3):419–28.4. Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968; Jan. 28(1):14–20.
Article5. Kim YD, Song D, Kim EH, Lee KJ, Lee HS, Nam CM, et al. Long-term mortality according to the characteristics of early neurological deterioration in ischemic stroke patients. Yonsei Med J. 2014; May. 55(3):669–75.
Article6. Lawton MT, Vates GE. Subarachnoid Hemorrhage. N Engl J Med. 2017; Jul. 377(3):257–66.
Article7. Makino S, Shibasaki T, Yamauchi N, Nishioka T, Mimoto T, Wakabayashi I, et al. Psychological stress increased corticotropin-releasing hormone mRNA and content in the central nucleus of the amygdala but not in the hypothalamic paraventricular nucleus in the rat. Brain Res. 1999; Dec. 850(1-2):136–43.
Article8. Marschall K, Schlesinger MD, Turndorf H, Puig MM. Beta-endorphin and ACTH levels in the perioperative period. Gen Pharmacol. 1989; 20(4):399–402.
Article9. McCann SM, Antunes-Rodrigues J, Franci CR, Anselmo-Franci JA, Karanth S, Rettori V. Role of the hypothalamic pituitary adrenal axis in the control of the response to stress and infection. Braz J Med Biol Res. 2000; Oct. 33(10):1121–31.
Article10. Pilozzi A, Carro C, Huang X. Roles of beta-Endorphin in Stress, Behavior, Neuroinflammation, and Brain Energy Metabolism. Int J Mol Sci. 2020; Dec. 22(1):11. Schedlowski M, Flüge T, Richter S, Tewes U, Schmidt RE, Wagner TO. Beta-endorphin, but not substance-P, is increased by acute stress in humans. Psychoneuroendocrinology. 1995; 20(1):103–10.
Article12. Sprouse-Blum AS, Smith G, Sugai D, Parsa FD. Understanding endorphins and their importance in pain management. Hawaii Med J. 2010; Mar. 69(3):70–1.13. Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009; Jun. 10(6):397–409.
Article14. Winklewski PJ, Radkowski M, Wszedybyl-Winklewska M, Demkow U. Stress Response, Brain noradrenergic system and cognition. Adv Exp Med Biol. 2017; Jan. 980:67–74.
Article15. Zhang F, Li P, Zhang C, Wang L, Jing SQ. The prognosis factors for endovascular coiling of aneurysm in patients with ruptured intracranial aneurysm. J Craniofac Surg. 2017; Sep. 28(6):e535–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simultaneous Occurrence of Aneurysmal Subarachnoid Hemorrhage and Hypertensive Intracerebral Hemorrhage
- Evaluation of Subarachnoid Hemorrhage due to Aneurysmal Rupture and Cerebral Vasospasm by CT
- Frequency of Aneurysmal Subarachnoid Hemorrhage in Perimesencephalic Subarachnoid Hemorrhage and Need of 4-vessel Angiography
- Clinical Analysis of Subarachnoid Hemorrhage with Intraventricular Hemorrhage due to Aneurysmal Rupture
- A Case of Turner Syndrome Presenting as Aneurysmal Subarachnoid Hemorrhage