Cancer Res Treat.
2022 Jul;54(3):651-660. 10.4143/crt.2022.116.
Psychological Aspects of Care in Cancer Patients in the Last Weeks/Days of Life
- Affiliations
-
- 1Department of Palliative Care, Rehabilitation, and Integrative Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX, USA
- KMID: 2531312
- DOI: http://doi.org/10.4143/crt.2022.116
Abstract
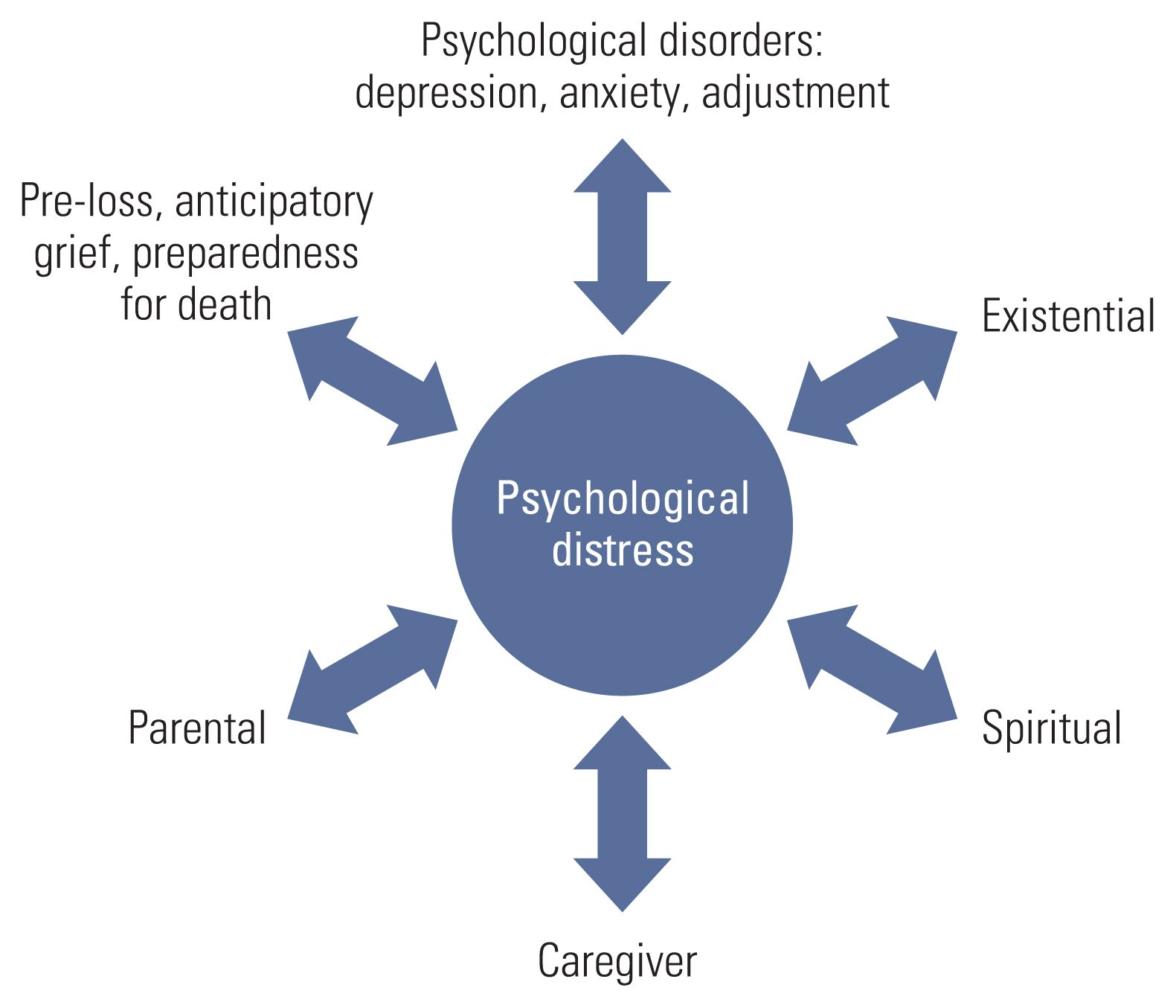
- Palliative care is comprised of an interdisciplinary team (IDT) approach with members from different disciplines who collaboratively work together to reduce multidimensional components of pain and suffering and improve quality of life for patients coping with a terminal illness. Psychosocial team members are integral to the palliative care IDT and provide expertise in assessment and empirically validated interventions to address psychological distress. The following paper will provide a review of different facets of psychological distress experienced by advanced cancer patients such as psychological disorders, existential distress, spiritual distress, caregiver distress, parental distress, and grief. Finally, an overview of commonly used screening and assessment tools as well as psychological interventions relevant for the palliative care population is presented.
Keyword
Figure
Reference
-
References
1. National Comprehensive Cancer Network. Distress management, version 2.2018 [Internet]. Plymouth Meeting, PA: National Comprehensive Cancer Network;2018. [cited 2022 Jan 10]. Available from: https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf .2. Bernard M, Strasser F, Gamondi C, Braunschweig G, Forster M, Kaspers-Elekes K, et al. Relationship between spirituality, meaning in life, psychological distress, wish for hastened death, and their influence on quality of life in palliative care patients. J Pain Symptom Manage. 2017; 54:514–22.
Article3. Meier DE, Beresford L. The palliative care team. J Palliat Med. 2008; 11:677–81.
Article4. Edmonds PM, Stuttaford JM, Penny J, Lynch AM, Chamberlain J. Do hospital palliative care teams improve symptom control? Use of a modified STAS as an evaluation tool. Palliat Med. 1998; 12:345–51.
Article5. Hearn J, Higginson IJ. Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliat Med. 1998; 12:317–32.
Article6. Phongtankuel V, Meador L, Adelman RD, Roberts J, Henderson CR Jr, Mehta SS, et al. Multicomponent palliative care interventions in advanced chronic diseases: a systematic review. Am J Hosp Palliat Care. 2018; 35:173–83.
Article7. Junger S, Payne S. Guidance on postgraudate education for psychologists involved in palliative care. Eur J Palliat Care. 2011; 18:238–52.8. Kasl-Godley JE, King DA, Quill TE. Opportunities for psychologists in palliative care: working with patients and families across the disease continuum. Am Psychol. 2014; 69:364–76.
Article9. Hamer M, Chida Y, Molloy GJ. Psychological distress and cancer mortality. J Psychosom Res. 2009; 66:255–8.
Article10. Krikorian A, Limonero JT, Roman JP, Vargas JJ, Palacio C. Predictors of suffering in advanced cancer. Am J Hosp Palliat Care. 2014; 31:534–42.
Article11. Seow H, Stevens T, Barbera LC, Burge F, McGrail K, Chan KK, et al. Trajectory of psychosocial symptoms among home care patients with cancer at end-of-life. Psychooncology. 2021; 30:103–10.
Article12. Lichtenthal WG, Nilsson M, Zhang B, Trice ED, Kissane DW, Breitbart W, et al. Do rates of mental disorders and existential distress among advanced stage cancer patients increase as death approaches? Psychooncology. 2009; 18:50–61.
Article13. Gao W, Bennett MI, Stark D, Murray S, Higginson IJ. Psychological distress in cancer from survivorship to end of life care: prevalence, associated factors and clinical implications. Eur J Cancer. 2010; 46:2036–44.
Article14. Hotopf M, Chidgey J, Addington-Hall J, Ly KL. Depression in advanced disease: a systematic review. Part 1. Prevalence and case finding. Palliat Med. 2002; 16:81–97.
Article15. Ryan D, Gallagher P, Wright S, Cassidy E. Methodological challenges in researching psychological distress and psychiatric morbidity among patients with advanced cancer: what does the literature (not) tell us? Palliat Med. 2012; 26:162–77.
Article16. Walker J, Holm Hansen C, Martin P, Sawhney A, Thekkumpurath P, Beale C, et al. Prevalence of depression in adults with cancer: a systematic review. Ann Oncol. 2013; 24:895–900.
Article17. Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001; 10:19–28.
Article18. Mehnert A, Brahler E, Faller H, Harter M, Keller M, Schulz H, et al. Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol. 2014; 32:3540–6.
Article19. Singer S, Das-Munshi J, Brahler E. Prevalence of mental health conditions in cancer patients in acute care: a meta-analysis. Ann Oncol. 2010; 21:925–30.20. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011; 12:160–74.
Article21. Ann-Yi S, Bruera E, Wu J, Liu DD, Agosta M, Williams JL, et al. Characteristics and outcomes of psychology referrals in a palliative care department. J Pain Symptom Manage. 2018; 56:344–51.
Article22. Pidgeon T, Johnson CE, Currow D, Yates P, Banfield M, Lester L, et al. A survey of patients’ experience of pain and other symptoms while receiving care from palliative care services. BMJ Support Palliat Care. 2016; 6:315–22.
Article23. Potash M, Breitbart W. Affective disorders in advanced cancer. Hematol Oncol Clin North Am. 2002; 16:671–700.
Article24. Fitzgerald P, Lo C, Li M, Gagliese L, Zimmermann C, Rodin G. The relationship between depression and physical symptom burden in advanced cancer. BMJ Support Palliat Care. 2015; 5:381–8.
Article25. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009; 115:5349–61.
Article26. Boston P, Bruce A, Schreiber R. Existential suffering in the palliative care setting: an integrated literature review. J Pain Symptom Manage. 2011; 41:604–18.
Article27. LeMay K, Wilson KG. Treatment of existential distress in life threatening illness: a review of manualized interventions. Clin Psychol Rev. 2008; 28:472–93.
Article28. Strang P, Strang S, Hultborn R, Arner S. Existential pain: an entity, a provocation, or a challenge? J Pain Symptom Manage. 2004; 27:241–50.29. Vehling S, Kissane DW. Existential distress in cancer: alleviating suffering from fundamental loss and change. Psychooncology. 2018; 27:2525–30.
Article30. Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002; 36:733–42.
Article31. Gabel S. Demoralization in health professional practice: development, amelioration, and implications for continuing education. J Contin Educ Health Prof. 2013; 33:118–26.
Article32. Jacobsen JC, Maytal G, Stern TA. Demoralization in medical practice. Prim Care Companion J Clin Psychiatry. 2007; 9:139–43.
Article33. Kissane DW, Wein S, Love A, Lee XQ, Kee PL, Clarke DM. The demoralization scale: a report of its development and preliminary validation. J Palliat Care. 2004; 20:269–76.
Article34. Ignatius J, De La Garza R 2nd. Frequency of demoralization and depression in cancer patients. Gen Hosp Psychiatry. 2019; 60:137–40.
Article35. Robinson S, Kissane DW, Brooker J, Burney S. A systematic review of the demoralization syndrome in individuals with progressive disease and cancer: a decade of research. J Pain Symptom Manage. 2015; 49:595–610.
Article36. Mehnert A, Vehling S, Hocker A, Lehmann C, Koch U. Demoralization and depression in patients with advanced cancer: validation of the German version of the demoralization scale. J Pain Symptom Manage. 2011; 42:768–76.
Article37. Tang PL, Wang HH, Chou FH. A systematic review and meta-analysis of demoralization and depression in patients with cancer. Psychosomatics. 2015; 56:634–43.
Article38. Best M, Leget C, Goodhead A, Paal P. An EAPC white paper on multi-disciplinary education for spiritual care in palliative care. BMC Palliat Care. 2020; 19:9.
Article39. Balboni TA, Paulk ME, Balboni MJ, Phelps AC, Loggers ET, Wright AA, et al. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010; 28:445–52.
Article40. Bovero A, Leombruni P, Miniotti M, Rocca G, Torta R. Spirituality, quality of life, psychological adjustment in terminal cancer patients in hospice. Eur J Cancer Care (Engl). 2016; 25:961–9.
Article41. McCoubrie RC, Davies AN. Is there a correlation between spirituality and anxiety and depression in patients with advanced cancer? Support Care Cancer. 2006; 14:379–85.
Article42. Nelson CJ, Rosenfeld B, Breitbart W, Galietta M. Spirituality, religion, and depression in the terminally ill. Psychosomatics. 2002; 43:213–20.
Article43. Schultz M, Meged-Book T, Mashiach T, Bar-Sela G. Distinguishing between spiritual distress, general distress, spiritual well-being, and spiritual pain among cancer patients during oncology treatment. J Pain Symptom Manage. 2017; 54:66–73.
Article44. Rego F, Nunes R. The interface between psychology and spirituality in palliative care. J Health Psychol. 2019; 24:279–87.
Article45. El Nawawi NM, Balboni MJ, Balboni TA. Palliative care and spiritual care: the crucial role of spiritual care in the care of patients with advanced illness. Curr Opin Support Palliat Care. 2012; 6:269–74.46. Rodin G, An E, Shnall J, Malfitano C. Psychological interventions for patients with advanced disease: implications for oncology and palliative care. J Clin Oncol. 2020; 38:885–904.
Article47. Hodges LJ, Humphris GM, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005; 60:1–12.
Article48. Ullrich A, Ascherfeld L, Marx G, Bokemeyer C, Bergelt C, Oechsle K. Quality of life, psychological burden, needs, and satisfaction during specialized inpatient palliative care in family caregivers of advanced cancer patients. BMC Palliat Care. 2017; 16:31.
Article49. Costa-Requena G, Cristofol R, Canete J. Caregivers’ morbidity in palliative care unit: predicting by gender, age, burden and self-esteem. Support Care Cancer. 2012; 20:1465–70.
Article50. Martin JM, Olano-Lizarraga M, Saracibar-Razquin M. The experience of family caregivers caring for a terminal patient at home: a research review. Int J Nurs Stud. 2016; 64:1–12.
Article51. Siegel K, Raveis VH, Houts P, Mor V. Caregiver burden and unmet patient needs. Cancer. 1991; 68:1131–40.
Article52. Park EM, Deal AM, Check DK, Hanson LC, Reeder-Hayes KE, Mayer DK, et al. Parenting concerns, quality of life, and psychological distress in patients with advanced cancer. Psychooncology. 2016; 25:942–8.
Article53. Park EM, Deal AM, Yopp JM, Edwards TP, Wilson DJ, Hanson LC, et al. End-of-life experiences of mothers with advanced cancer: perspectives of widowed fathers. BMJ Support Palliat Care. 2016; 6:437–44.
Article54. Schmitt F, Santalahti P, Saarelainen S, Savonlahti E, Romer G, Piha J. Cancer families with children: factors associated with family functioning: a comparative study in Finland. Psychooncology. 2008; 17:363–72.55. Park EM, Stephenson EM, Moore CW, Deal AM, Muriel AC. Parental psychological distress and cancer stage: a comparison of adults with metastatic and non-metastatic cancer. Support Care Cancer. 2019; 27:2443–51.
Article56. Moore CW, Rauch PK, Baer L, Pirl WF, Muriel AC. Parenting changes in adults with cancer. Cancer. 2015; 121:3551–7.
Article57. Muriel AC, Moore CW, Baer L, Park ER, Kornblith AB, Pirl W, et al. Measuring psychosocial distress and parenting concerns among adults with cancer: the Parenting Concerns Questionnaire. Cancer. 2012; 118:5671–8.
Article58. Northouse LL, Walker J, Schafenacker A, Mood D, Mellon S, Galvin E, et al. A family-based program of care for women with recurrent breast cancer and their family members. Oncol Nurs Forum. 2002; 29:1411–9.
Article59. Semple CJ, McCance T. Experience of parents with head and neck cancer who are caring for young children. J Adv Nurs. 2010; 66:1280–90.
Article60. Semple CJ, McCance T. Parents’ experience of cancer who have young children: a literature review. Cancer Nurs. 2010; 33:110–8.61. Nilsson ME, Maciejewski PK, Zhang B, Wright AA, Trice ED, Muriel AC, et al. Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer. 2009; 115:399–409.
Article62. Yellen SB, Cella DF. Someone to live for: social well-being, parenthood status, and decision-making in oncology. J Clin Oncol. 1995; 13:1255–64.
Article63. Fasse L, Sultan S, Flahault C, Mackinnon CJ, Dolbeault S, Bredart A. How do researchers conceive of spousal grief after cancer? A systematic review of models used by researchers to study spousal grief in the cancer context. Psychooncology. 2014; 23:131–42.
Article64. Kim Y, Lucette A, Loscalzo M. Bereavement needs of adults, children, and families after cancer. Cancer J. 2013; 19:444–57.
Article65. Nielsen MK, Neergaard MA, Jensen AB, Bro F, Guldin MB. Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin Psychol Rev. 2016; 44:75–93.
Article66. Nielsen MK, Neergaard MA, Jensen AB, Vedsted P, Bro F, Guldin MB. Preloss grief in family caregivers during end-of-life cancer care: a nationwide population-based cohort study. Psychooncology. 2017; 26:2048–56.
Article67. Treml J, Schmidt V, Nagl M, Kersting A. Pre-loss grief and preparedness for death among caregivers of terminally ill cancer patients: a systematic review. Soc Sci Med. 2021; 284:114240.
Article68. Hebert RS, Dang Q, Schulz R. Preparedness for the death of a loved one and mental health in bereaved caregivers of patients with dementia: findings from the REACH study. J Palliat Med. 2006; 9:683–93.
Article69. Institute of Medicine Committee on the Future Health Care. Workforce for Older Americans Retooling for an aging America: building the Health Care Workforce. Washington, DC: National Academies Press;2008.70. Hui D, Bruera E. The Edmonton symptom assessment system 25 years later: past, present, and future developments. J Pain Symptom Manage. 2017; 53:630–43.71. Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, et al. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994; 30A:1326–36.
Article72. Ewing G, Todd C, Rogers M, Barclay S, McCabe J, Martin A. Validation of a symptom measure suitable for use among palliative care patients in the community: CAMPAS-R. J Pain Symptom Manage. 2004; 27:287–99.
Article73. Murtagh FE, Ramsenthaler C, Firth A, Groeneveld EI, Lovell N, Simon ST, et al. A brief, patient- and proxy-reported outcome measure in advanced illness: validity, reliability and responsiveness of the Integrated Palliative care Outcome Scale (IPOS). Palliat Med. 2019; 33:1045–57.
Article74. Breitbart W, Rosenfeld B, Roth A, Smith MJ, Cohen K, Passik S. The Memorial Delirium Assessment Scale. J Pain Symptom Manage. 1997; 13:128–37.
Article75. Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995; 94:135–40.76. Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984; 252:1905–7.
Article77. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–70.
Article78. Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. 2021; 279:473–83.
Article79. Kroenke K. PHQ-9: global uptake of a depression scale. World Psychiatry. 2021; 20:135–6.80. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011; 168:1266–77.
Article81. Robinson S, Kissane DW, Brooker J, Michael N, Fischer J, Franco M, et al. Refinement and revalidation of the demoralization scale: The DS-II-internal validity. Cancer. 2016; 122:2251–9.
Article82. Sands MB, Wee I, Agar M, Vardy JL. The detection of delirium in admitted oncology patients: a scoping review. Eur Geriatr Med. 2022; 13:33–51.
Article83. Yusufov M, Braun IM, Pirl WF. A systematic review of substance use and substance use disorders in patients with cancer. Gen Hosp Psychiatry. 2019; 60:128–36.
Article84. Fulton JJ, Newins AR, Porter LS, Ramos K. Psychotherapy targeting depression and anxiety for use in palliative care: a meta-analysis. J Palliat Med. 2018; 21:1024–37.
Article85. Okuyama T, Akechi T, Mackenzie L, Furukawa TA. Psychotherapy for depression among advanced, incurable cancer patients: a systematic review and meta-analysis. Cancer Treat Rev. 2017; 56:16–27.
Article86. von Blanckenburg P, Leppin N. Psychological interventions in palliative care. Curr Opin Psychiatry. 2018; 31:389–95.
Article87. Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005; 23:5520–5.
Article88. Chochinov HM, Kristjanson LJ, Breitbart W, McClement S, Hack TF, Hassard T, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011; 12:753–62.
Article89. Breitbart W, Poppito S, Rosenfeld B, Vickers AJ, Li Y, Abbey J, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012; 30:1304–9.
Article90. Breitbart W, Rosenfeld B, Pessin H, Applebaum A, Kuli-kowski J, Lichtenthal WG. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol. 2015; 33:749–54.
Article91. Applebaum AJ, Kulikowski JR, Breitbart W. Meaning-centered Psychotherapy for Cancer Caregivers (MCP-C): rationale and overview. Palliat Support Care. 2015; 13:1631–41.
Article92. Rosenfeld B, Saracino R, Tobias K, Masterson M, Pessin H, Applebaum A, et al. Adapting meaning-centered psychotherapy for the palliative care setting: results of a pilot study. Palliat Med. 2017; 31:140–6.
Article93. Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008; 300:1665–73.
Article94. Leichsenring F, Leibing E. Supportive-expressive (SE) psychotherapy: an update. Curr Psychiatr Rev. 2007; 3:57–64.
Article95. Classen C, Butler LD, Koopman C, Miller E, DiMiceli S, Giese-Davis J, et al. Supportive-expressive group therapy and distress in patients with metastatic breast cancer: a randomized clinical intervention trial. Arch Gen Psychiatry. 2001; 58:494–501.
Article96. Lai J, Song H, Ren Y, Li S, Xiao F. Effectiveness of supportive-expressive group therapy in women with breast cancer: a systematic review and meta-analysis. Oncol Res Treat. 2021; 44:252–60.
Article97. Oberoi D, Martopullo C, Bultz BD, Carlson LE. The effectiveness of a men-only supportive expressive group therapy intervention for psychosocial health outcomes in gastrointestinal cancer patients: a 6-month longitudinal study. Health Qual Life Outcomes. 2021; 19:47.98. Beck AT. The current state of cognitive therapy: a 40-year retrospective. Arch Gen Psychiatry. 2005; 62:953–9.99. Getu MA, Chen C, Panpan W, Mboineki JF, Dhakal K, Du R. The effect of cognitive behavioral therapy on the quality of life of breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual Life Res. 2021; 30:367–84.
Article100. Gonzalez-Fernandez S, Fernandez-Rodriguez C. Acceptance and commitment therapy in cancer: review of applications and findings. Behav Med. 2019; 45:255–69.
Article101. Li H, Wong CL, Jin X, Chen J, Chong YY, Bai Y. Effects of acceptance and commitment therapy on health-related outcomes for patients with advanced cancer: a systematic review. Int J Nurs Stud. 2021; 115:103876.
Article102. Lo C, Hales S, Chiu A, Panday T, Malfitano C, Jung J, et al. Managing Cancer And Living Meaningfully (CALM): randomised feasibility trial in patients with advanced cancer. BMJ Support Palliat Care. 2019; 9:209–18.
Article103. Rodin G, Lo C, Rydall A, Shnall J, Malfitano C, Chiu A, et al. Managing Cancer and Living Meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol. 2018; 36:2422–32.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Psychosocial Aspects and Mental Health in Cancer Patients
- Management of Physical Symptoms in Patients with Advanced Cancer during the Last Weeks and Days of Life
- Psychosocial aspects of childhood cancer survivors
- Update on distress management for cancer patients
- Factors Affecting Psychological Burnout in Nurses Caring for Terminal Cancer Patients