Korean Circ J.
2022 Jul;52(7):529-540. 10.4070/kcj.2021.0390.
Long-Term Clinical Outcomes of Iliac Artery Endovascular Therapy in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yonsei University College of Medicine and Cardiovascular Center, Yongin Severance Hospital, Yongin, Korea
- 2Department of Cardiology, Ewha Womans University Medical Center, Ewha Womans University, Seoul, Korea
- 3Department of Cardiology and Cardiovascular Research Institute, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 4Division of Biostatistics, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 5Division of Cardiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 6Division of Cardiology, Chungnam National University Sejong Hospital, Sejong, Korea
- 7Division of Cardiology, Seoul National University Bundang Hospital, Seoungnam, Korea
- 8Division of Cardiology, Korea University Anam Hospital, Seoul, Korea
- 9Division of Cardiology, Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea
- 10Division of Cardiology, Jeonbuk National University Hospital, Jeonju, Korea
- 11Division of Cardiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2530734
- DOI: http://doi.org/10.4070/kcj.2021.0390
Abstract
- Background and Objectives
Limited data are available regarding long-term clinical outcomes of iliac artery endovascular therapy (EVT) in real-world practice. This study investigated long-term outcomes according to Trans-Atlantic Inter-Society Consensus (TASC) classifications.
Methods
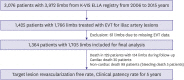
We analyzed data from 1,705 limbs of 1,364 patients from the retrospective cohort of the multicenter Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Disease registry. The primary endpoint was target lesion revascularization (TLR)-free survival.
Results
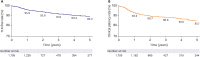
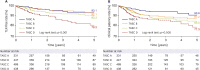
TASC A, B, C, and D lesions were present in 19.4%, 26.2%, 28.7%, and 25.7% of the treated limbs, respectively. The technical success rate was 96.2% and did not differ between TASC lesion types. Complications occurred in 6.8% of cases and more occurred in TASC D (11.8%). Iliac artery EVT showed a 5-year TLR-free survival of 89.2%. The TASC D group had the lowest TLR-free rate of 79.3%. TASC D (hazard ratio [HR], 1.75; 95% confidence interval [CI], 1.12–2.73; p=0.014), plain old balloon angioplasty (HR, 4.25; 95% CI, 2.03–8.88; p<0.001), current smoker (HR, 1.89; 95% CI, 1.26–2.83; p=0.002), previous bypass surgery (HR, 3.04;95% CI, 1.28–7.19; p=0.011), combined femoropopliteal treatment (HR, 4.89; 95% CI, 3.19–7.50; p<0.001), combined below the knee treatment (HR, 2.20; 95% CI, 1.25–3.89; p=0.007), and complications (HR, 1.86; 95% CI, 1.07–3.24; p=0.028) were predictors for TLR.
Conclusions
Iliac artery EVT achieved excellent technical success and 5-year TLR-free survival. TASC D showed a favorable but lower 5-year TLR-free survival rate and higher complication rate compared with other TASC groups.
Figure
Cited by 1 articles
-
Endovascular Therapy for Complex Iliac Lesions: There Is Much More to Be Defined
Yahya Alansari, Pil Hyung Lee
Korean Circ J. 2022;52(7):541-543. doi: 10.4070/kcj.2022.0145.
Reference
-
1. Criqui MH, Matsushita K, Aboyans V, et al. Lower extremity peripheral artery disease: contemporary epidemiology, management gaps, and future directions: a scientific statement from the American Heart Association. Circulation. 2021; 144:e171–e191. PMID: 34315230.
Article2. Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2017; 69:e71–126. PMID: 27851992.3. Aboyans V, Ricco JB, Bartelink ME, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. Endorsed by: the European Stroke Organization (ESO). The task force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018; 39:763–816. PMID: 28886620.4. Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007; 45(Suppl S):S5–67. PMID: 17223489.
Article5. Indes JE, Pfaff MJ, Farrokhyar F, et al. Clinical outcomes of 5358 patients undergoing direct open bypass or endovascular treatment for aortoiliac occlusive disease: a systematic review and meta-analysis. J Endovasc Ther. 2013; 20:443–455. PMID: 23914850.
Article6. Premaratne S, Newman J, Hobbs S, Garnham A, Wall M. Meta-analysis of direct surgical versus endovascular revascularization for aortoiliac occlusive disease. J Vasc Surg. 2020; 72:726–737. PMID: 32171442.
Article7. Rossi M, Iezzi R. Cardiovascular and Interventional Radiological Society of Europe guidelines on endovascular treatment in aortoiliac arterial disease. Cardiovasc Intervent Radiol. 2014; 37:13–25. PMID: 24196266.
Article8. Ko YG, Ahn CM, Min PK, et al. Baseline characteristics of a retrospective patient cohort in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry. Korean Circ J. 2017; 47:469–476. PMID: 28765738.
Article9. Society for Vascular Surgery Lower Extremity Guidelines Writing Group. Conte MS, Pomposelli FB, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 2015; 61:2S–41S. PMID: 25638515.
Article10. European Stroke Organisation. Tendera M, Aboyans V, et al. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the task force on the diagnosis and treatment of peripheral artery diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2851–2906. PMID: 21873417.11. de Donato G, Bosiers M, Setacci F, et al. 24-month data from the BRAVISSIMO: a large-scale prospective registry on iliac stenting for TASC A & B and TASC C & D lesions. Ann Vasc Surg. 2015; 29:738–750. PMID: 25733220.
Article12. Piffaretti G, Fargion AT, Dorigo W, et al. Outcomes from the multicenter italian registry on primary endovascular treatment of aortoiliac occlusive disease. J Endovasc Ther. 2019; 26:623–632. PMID: 31331235.
Article13. Jongkind V, Akkersdijk GJ, Yeung KK, Wisselink W. A systematic review of endovascular treatment of extensive aortoiliac occlusive disease. J Vasc Surg. 2010; 52:1376–1383. PMID: 20598474.
Article14. Suzuki K, Mizutani Y, Soga Y, et al. Efficacy and safety of endovascular therapy for aortoiliac TASC D lesions. Angiology. 2017; 68:67–73. PMID: 26980775.
Article15. Çakmak EÖ, Bayam E, Yilmaz F, et al. Midterm outcomes on primary endovascular treatment of 395 aortoiliac occlusive disease patients: a single-center experience. Angiology. 2021; 72:640–650. PMID: 33541091.
Article16. Bechter-Hugl B, Falkensammer J, Gorny O, Greiner A, Chemelli A, Fraedrich G. The influence of gender on patency rates after iliac artery stenting. J Vasc Surg. 2014; 59:1588–1596. PMID: 24548520.
Article17. Psacharopulo D, Ferrero E, Ferri M, et al. Increasing efficacy of endovascular recanalization with covered stent graft for TransAtlantic Inter-Society Consensus II D aortoiliac complex occlusion. J Vasc Surg. 2015; 62:1219–1226. PMID: 26391459.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Management for Chronic Steno-occlusion of Iliac and Femoral Arteries
- Endovascular Treatment of Iliac & Femoral Artery Occlusive Disease
- Novel Strategies for the Hostile Iliac Artery during Endovascular Aortic Aneurysm Repair
- Baseline Characteristics of a Retrospective Patient Cohort in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry
- Adjunctive Procedures for Challenging Endovascular Abdominal Aortic Repair: When Needed and How Effective?