Korean Circ J.
2022 Jun;52(6):429-440. 10.4070/kcj.2021.0342.
Long-term Clinical Outcomes and Prognostic Factors After Endovascular Treatment in Patients With Chronic Limb Threatening Ischemia
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea
- 2Division of Cardiology, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Health Promotion, Health Promotion Center, Severance Hospital, Yonsei University Health System, Seoul, Korea
- 4Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 5Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea
- 6Division of Cardiology, Seoul National University Bundang Hospital, Seongnam, Korea
- 7Division of Cardiology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 8Division of Cardiology, Department of Internal Medicine, Jeonbuk National University Hospital, Jeonju, Korea
- 9Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 10Division of Cardiology, Hallym University Sacred Heart Hospital, Anyang, Korea
- KMID: 2530447
- DOI: http://doi.org/10.4070/kcj.2021.0342
Abstract
- Background and Objectives
Endovascular therapy (EVT) first strategy has been widely adopted for the treatment of chronic limb threatening ischemia (CLTI) patients in realworld practice. This study aimed to investigate long-term outcomes of CLTI patients who underwent EVT and identify prognostic factors.
Methods
From the retrospective cohorts of a Korean multicenter endovascular therapy registry, 1,036 patients with CLTI (792 men, 68.8 ± 9.5 years) were included. The primary endpoint was amputation-free survival (AFS) defined as the absence of major amputation or death. Secondary endpoints were major adverse limb events (MALE; a composite of major amputation, minor amputation, and reintervention).
Results
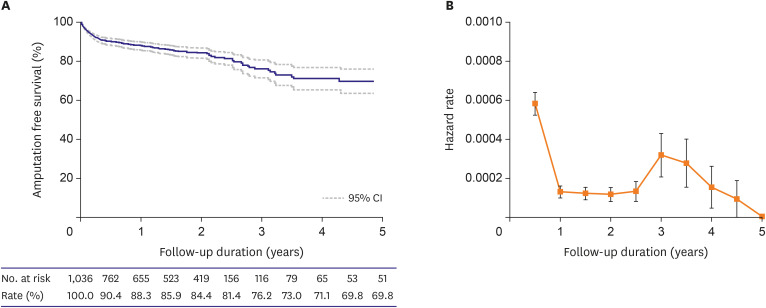
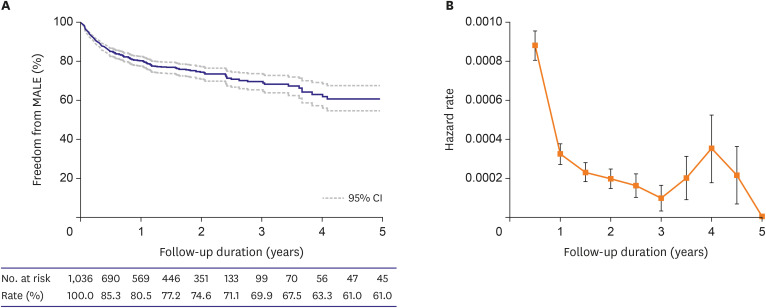
Five-year AFS and freedom from MALE were 69.8% and 61%, respectively. After multivariate analysis, age (hazard ratio [HR], 1.476; p<0.001), end-stage renal disease (ESRD; HR, 2.340; p<0.001), Rutherford category (RC) 6 (HR, 1.456; p=0.036), and suboptimal EVT (HR, 1.798; p=0.005) were identified as predictors of major amputation or death, whereas smoking (HR, 0.594; p=0.007) was protective. Low body mass index (HR, 1.505; p=0.046), ESRD (HR, 1.648; p=0.001), femoropopliteal lesion (HR, 1.877; p=0.004), RC-6 (HR, 1.471; p=0.008), and suboptimal EVT (HR, 1.847; p=0.001) were predictors of MALE. The highest hazard rates were observed during the first 6 months for both major amputation or death and MALE. After that, the hazard rate decreased and rose again after 3–4 years.
Conclusions
In CLTI patients, long-term outcomes of EVT were acceptable. ESRD, RC-6, and suboptimal EVT were common predictors for poor clinical outcomes.
Figure
Cited by 2 articles
-
Critical Determinants of Chronic Limb Threatening Ischemia After Endovascular Treatment
Wonho Kim
Korean Circ J. 2022;52(6):441-443. doi: 10.4070/kcj.2022.0064.Endovascular Therapy for Complex Iliac Lesions: There Is Much More to Be Defined
Yahya Alansari, Pil Hyung Lee
Korean Circ J. 2022;52(7):541-543. doi: 10.4070/kcj.2022.0145.
Reference
-
1. Farber A, Eberhardt RT. The current state of critical limb ischemia: a systematic review. JAMA Surg. 2016; 151:1070–1077. PMID: 27551978.2. Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017; 135:e726–e779. PMID: 27840333.3. Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018; 39:763–816. PMID: 28886620.4. Adam DJ, Beard JD, Cleveland T, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005; 366:1925–1934. PMID: 16325694.
Article5. Mustapha JA, Katzen BT, Neville RF, et al. Propensity score-adjusted comparison of long-term outcomes among revascularization strategies for critical limb ischemia. Circ Cardiovasc Interv. 2019; 12:e008097. PMID: 31495219.
Article6. Lin JH, Brunson A, Romano PS, Mell MW, Humphries MD. Endovascular-first treatment is associated with improved amputation-free survival in patients with critical limb ischemia. Circ Cardiovasc Qual Outcomes. 2019; 12:e005273. PMID: 31357888.
Article7. Dalal PK, Prasad A. Contemporary outcomes of endovascular intervention for critical limb ischemia. Interv Cardiol Clin. 2017; 6:251–259. PMID: 28257772.
Article8. Schmidt A, Bausback Y, Piorkowski M, et al. Retrograde tibioperoneal access for complex infrainguinal occlusions: short- and long-term outcomes of 554 endovascular interventions. JACC Cardiovasc Interv. 2019; 12:1714–1726. PMID: 31488299.9. Ko YG, Ahn CM, Min PK, et al. Baseline characteristics of a retrospective patient cohort in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) registry. Korean Circ J. 2017; 47:469–476. PMID: 28765738.
Article10. Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997; 26:517–538. PMID: 9308598.
Article11. Stella J, Engelbertz C, Gebauer K, et al. Outcome of patients with chronic limb-threatening ischemia with and without revascularization. Vasa. 2020; 49:121–127. PMID: 31808379.
Article12. Mustapha JA, Katzen BT, Neville RF, et al. Determinants of Long-term outcomes and costs in the management of critical limb ischemia: a population-based cohort study. J Am Heart Assoc. 2018; 7:e009724. PMID: 30369325.
Article13. Almasri J, Adusumalli J, Asi N, et al. A systematic review and meta-analysis of revascularization outcomes of infrainguinal chronic limb-threatening ischemia. J Vasc Surg. 2018; 68:624–633. PMID: 29804736.
Article14. Iida O, Nakamura M, Yamauchi Y, et al. 3-Year outcomes of the OLIVE registry, a prospective multicenter study of patients with critical limb ischemia: a prospective, multi-center, three-year follow-up study on endovascular treatment for infra-inguinal vessel in patients with critical limb ischemia. JACC Cardiovasc Interv. 2015; 8:1493–1502. PMID: 26404203.
Article15. Bradbury AW, Adam DJ, Bell J, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: an intention-to-treat analysis of amputation-free and overall survival in patients randomized to a bypass surgery-first or a balloon angioplasty-first revascularization strategy. J Vasc Surg. 2010; 51:5S–17S. PMID: 20435258.
Article16. Soga Y, Iida O, Takahara M, et al. Two-year life expectancy in patients with critical limb ischemia. JACC Cardiovasc Interv. 2014; 7:1444–1449. PMID: 25523536.17. Vierthaler L, Callas PW, Goodney PP, et al. Determinants of survival and major amputation after peripheral endovascular intervention for critical limb ischemia. J Vasc Surg. 2015; 62:655–664.e8. PMID: 26215708.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Comprehension and Application of Angiosome Concept in Critical Limb Ischemia
- Critical Determinants of Chronic Limb Threatening Ischemia After Endovascular Treatment
- Endovascular treatment of acute limb ischemia due to thrombotic occlusion of the suprainguinal artery
- The Early Outcome of the Endovascular Subintimal Angioplasty for Chronic Critical Limb Ischemia in Infrainguinal Vascular Disease
- Endovascular Revascularization for Patients with Critical Limb Ischemia: Impact on Wound Healing and Long Term Clinical Results in 189 Limbs