J Korean Med Sci.
2022 Jun;37(22):e78. 10.3346/jkms.2022.37.e78.
Impact of Mediastinal Lymphadenopathy on the Severity of COVID-19 Pneumonia: A Nationwide Multicenter Cohort Study
- Affiliations
-
- 1Department of Radiology, Chonnam National University Medical School, Chonnam National University Hospital, Gwangju, Korea
- 2Department of Radiology, Chonnam National University Medical School, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 3Department of Radiology, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 4Department of Radiology, Seoul National University Hospital, Seoul National College of Medicine, Seoul, Korea
- 5Department of Radiology and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 6Department of Radiology, Chungbuk National University College of Medicine, Chungbuk National University Hospital, Cheongju, Korea
- KMID: 2530425
- DOI: http://doi.org/10.3346/jkms.2022.37.e78
Abstract
- Background
We analyzed the differences between clinical characteristics and computed tomography (CT) findings in patients with coronavirus disease 2019 (COVID-19) to establish potential relationships with mediastinal lymphadenopathy and clinical outcomes.
Methods
We compared the clinical characteristics and CT findings of COVID-19 patients from a nationwide multicenter cohort who were grouped based on the presence or absence of mediastinal lymphadenopathy. Differences between clinical characteristics and CT findings in these groups were analyzed. Univariate and multivariate analyses were performed to determine the impact of mediastinal lymphadenopathy on clinical outcomes.
Results
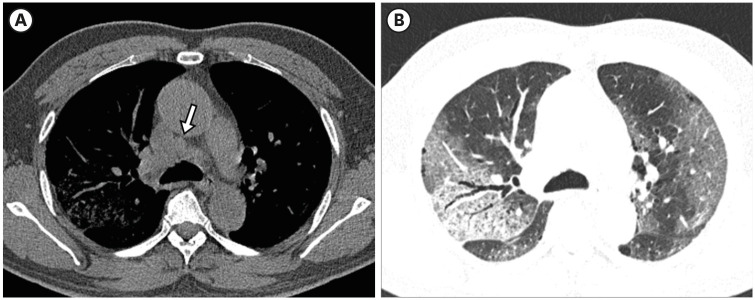
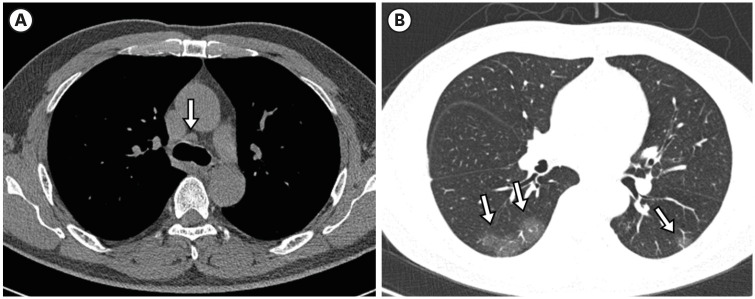
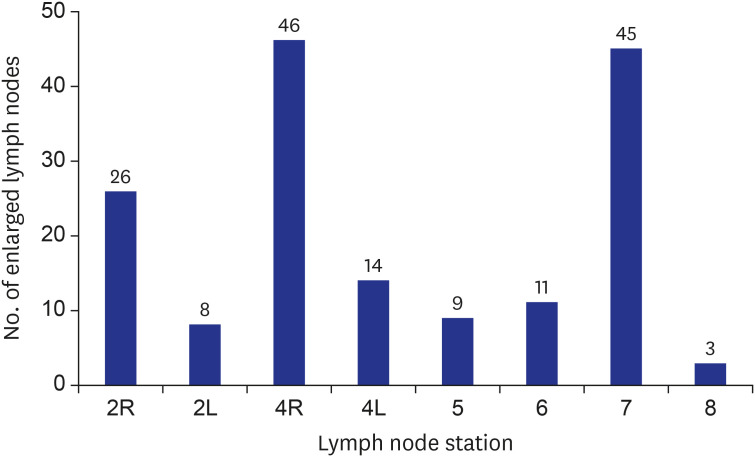
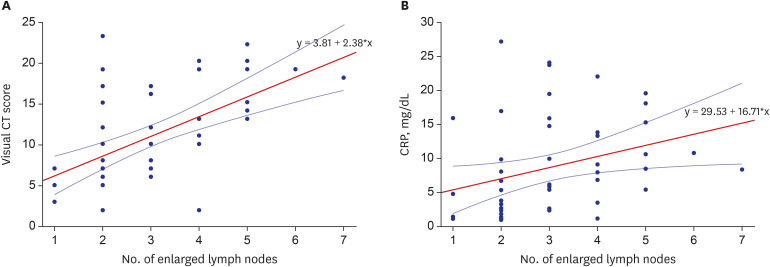
Of the 344 patients included in this study, 53 (15.4%) presented with mediastinal lymphadenopathy. The rate of diffuse alveolar damage pattern pneumonia and the visual CT scores were significantly higher in patients with mediastinal lymphadenopathy than in those without (P < 0.05). A positive correlation between the number of enlarged mediastinal lymph nodes and visual CT scores was noted in patients with mediastinal lymphadenopathy (Spearman’s ρ = 0.334, P < 0.001). Multivariate analysis showed that mediastinal lymphadenopathy was independently associated with a higher risk of intensive care unit (ICU) admission (odds ratio, 95% confidence interval; 3.25, 1.06-9.95) but was not significantly associated with an increased risk of in-hospital death in patients with COVID-19.
Conclusion
COVID-19 patients with mediastinal lymphadenopathy had a larger extent of pneumonia than those without. Multivariate analysis adjusted for clinical characteristics and CT findings revealed that the presence of mediastinal lymphadenopathy was significantly associated with ICU admission.
Figure
Reference
-
1. Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020; 30(8):4381–4389. PMID: 32193638.2. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from 2019 coronavirus disease 2019 (COVID-19). Radiology. 2020; 295(3):715–721. PMID: 32053470.3. Wei J, Xu H, Xiong J, Shen Q, Fan B, Ye C, et al. 2019 novel coronavirus (COVID-19) pneumonia: serial computed tomography findings. Korean J Radiol. 2020; 21(4):501–504. PMID: 32100486.4. Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, et al. Radiological Society of North America expert consensus document on reporting chest CT findings related to COVID-19: endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothorac Imaging. 2020; 2(2):e200152. PMID: 33778571.5. Kwee TC, Kwee RM. Chest CT in COVID-19: what the radiologist needs to know. Radiographics. 2020; 40(7):1848–1865. PMID: 33095680.6. Li Y, Yang Z, Ai T, Wu S, Xia L. Association of “initial CT” findings with mortality in older patients with coronavirus disease 2019 (COVID-19). Eur Radiol. 2020; 30(11):6186–6193. PMID: 32524220.7. Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020; 55(6):327–331. PMID: 32118615.8. Bao C, Liu X, Zhang H, Li Y, Liu J. Coronavirus disease 2019 (COVID-19) CT findings: a systematic review and meta-analysis. J Am Coll Radiol. 2020; 17(6):701–709. PMID: 32283052.9. Zhu J, Zhong Z, Li H, Ji P, Pang J, Li B, et al. CT imaging features of 4121 patients with COVID-19: A meta-analysis. J Med Virol. 2020; 92(7):891–902. PMID: 32314805.10. Valette X, du Cheyron D, Goursaud S. Mediastinal lymphadenopathy in patients with severe COVID-19. Lancet Infect Dis. 2020; 20(11):1230.11. Sardanelli F, Cozzi A, Monfardini L, Bnà C, Foà RA, Spinazzola A, et al. Association of mediastinal lymphadenopathy with COVID-19 prognosis. Lancet Infect Dis. 2020; 20(11):1230–1231.12. Satici C, Cengel F, Gurkan O, Demirkol MA, Altunok ES, Esatoglu SN. Mediastinal lymphadenopathy may predict 30-day mortality in patients with COVID-19. Clin Imaging. 2021; 75:119–124. PMID: 33545439.13. Yoon SH, Ham SY, Nam BD, Chae KJ, Lee D, Yoo JY, et al. Establishment of a nationwide Korean imaging cohort of coronavirus disease 2019. J Korean Med Sci. 2020; 35(46):e413. PMID: 33258333.14. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307(23):2526–2533. PMID: 22797452.15. World Health Organization. Medical certification, ICD mortality coding, and reporting mortality associated with COVID-19: technical note, 7 June 2020. Updated 2020. Accessed April 15, 2017. https://apps.who.int/iris/handle/10665/332297 .16. Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, et al. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005; 236(3):1011–1019. PMID: 16014441.17. Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol. 2009; 4(5):568. 77. PMID: 19357537.18. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008; 246(3):697–722. PMID: 18195376.19. Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, et al. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol. 2020; 30(12):6808–6817. PMID: 32623505.20. Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003; 228(2):303–308. PMID: 12819342.21. Chon Y, Kim JY, Suh YJ, Lee JY, Park JS, Moon SM, et al. Adverse initial CT findings associated with poor prognosis of coronavirus disease. J Korean Med Sci. 2020; 35(34):e316. PMID: 32864912.22. Grodecki K, Lin A, Cadet S, McElhinney PA, Razipour A, Chan C, et al. Quantitative burden of COVID-19 pneumonia on chest CT predicts adverse outcomes: a post-hoc analysis of a prospective international registry. Radiol Cardiothorac Imaging. 2020; 2(5):e200389. PMID: 33778629.23. Li X, Fang X, Bian Y, Lu J. Comparison of chest CT findings between COVID-19 pneumonia and other types of viral pneumonia: a two-center retrospective study. Eur Radiol. 2020; 30(10):5470–5478. PMID: 32394279.24. Li Y, Wu J, Wang S, Li X, Zhou J, Huang B, et al. Progression to fibrosing diffuse alveolar damage in a series of 30 minimally invasive autopsies with COVID-19 pneumonia in Wuhan, China. Histopathology. 2021; 78(4):542–555. PMID: 32926596.25. Jeong YJ, Nam BD, Yoo JY, Kim KI, Kang H, Hwang JH, et al. Prognostic implications of CT feature analysis in patients with COVID-19: a nationwide cohort study. J Korean Med Sci. 2021; 36(8):e51. PMID: 33650333.26. Jin C, Tian C, Wang Y, Wu CC, Zhao H, Liang T, et al. A pattern categorization of CT findings to predict outcome of COVID-19 pneumonia. Front Public Health. 2020; 8:567672. PMID: 33072703.27. Gandhi RT, Lynch JB, Del Rio C. Mild or moderate Covid-19. N Engl J Med. 2020; 383(18):1757–1766. PMID: 32329974.28. Jang SY, Seon JY, Eun BL, Koh SB, Yoo JH, Lee WY, et al. Risk factors of outcomes of COVID-19 patients in Korea: focus on early symptoms. J Korean Med Sci. 2021; 36(18):e132. PMID: 33975399.29. Lee JY, Kim HA, Huh K, Hyun M, Rhee JY, Jang S, et al. Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID-19 in Korea. J Korean Med Sci. 2020; 35(23):e223. PMID: 32537957.30. Suh HJ, Lee E, Park SW. Clinical characteristics of COVID-19: risk factors for early oxygen requirement after hospitalization. J Korean Med Sci. 2021; 36(19):e139. PMID: 34002553.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mediastinal Emphysema, Giant Bulla, and PneumothoraxDeveloped during the Course of COVID-19 Pneumonia
- Outcomes of COVID-19 in Thai kidney transplant recipients in the vaccination era
- The Comparison of Dysphagia between COVID-19 Pneumonia and Aspiration Pneumonia
- Clinical and Radiologic Findings of COVID-19 Pneumonia: South Korean Experience from Three Cases
- The coronavirus disease 2019 pandemic and chronic diseases