J Korean Med Sci.
2022 Jun;37(22):e175. 10.3346/jkms.2022.37.e175.
Clinical Characteristics and Risk Factors for Mortality in Critical Coronavirus Disease 2019 Patients 50 Years of Age or Younger During the Delta Wave: Comparison With Patients > 50 Years in Korea
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 2Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 3Division of Infectious Diseases, Department of Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Infectious Diseases, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 5Division of Infectious Diseases, Department of Medicine, Dankook University School of Medicine, Cheonan, Korea
- 6Department of Internal Medicine, Chungnam National University School of Medicine, Daejeon, Korea
- 7Devision of Infectious Diseases, Chungnam National University Sejong Hospital, Sejong, Korea
- 8Division of Infectious Diseases, Department of Medicine, Changwon Samsung Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 9Division of Infectious Diseases, Department of Internal Medicine, Chungnam National University School of Medicine, Daejeon, Korea
- 10Division of Infectious Diseases, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea
- 11Division of Infectious Diseases, Department of Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 12Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea
- 13Division of Infectious Diseases, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2530417
- DOI: http://doi.org/10.3346/jkms.2022.37.e175
Abstract
- Background
Numerous patients around the globe are dying from coronavirus disease 2019 (COVID-19). While age is a known risk factor, risk analysis in the young generation is lacking. The present study aimed to evaluate the clinical features and mortality risk factors in younger patients (≤ 50 years) with a critical case of COVID-19 in comparison with those among older patients (> 50 years) in Korea.
Methods
We analyzed the data of adult patients only in critical condition (requiring high flow nasal cannula oxygen therapy or higher respiratory support) hospitalized with PCR-confirmed COVID-19 at 11 hospitals in Korea from July 1, 2021 to November 30, 2021 when the delta variant was a dominant strain. Patients’ electronic medical records were reviewed to identify clinical characteristics.
Results
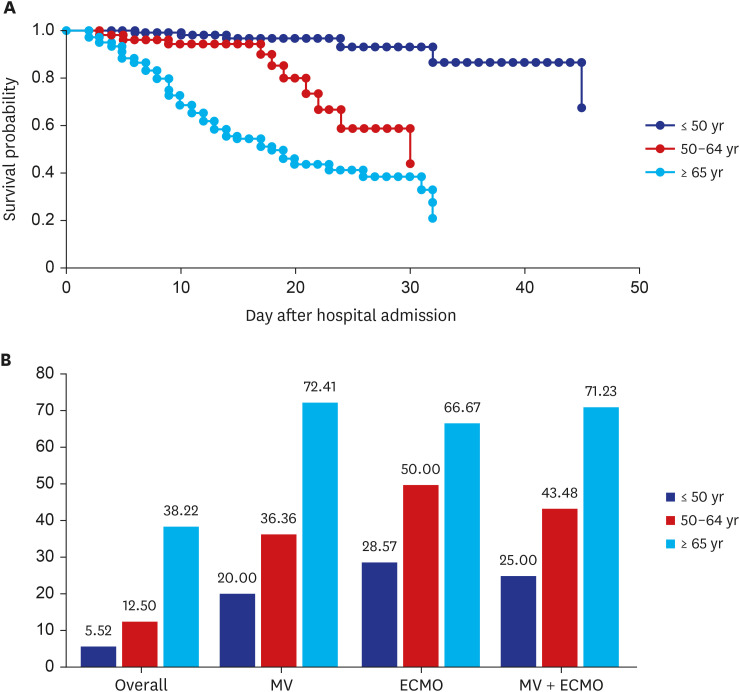
During the study period, 448 patients were enrolled. One hundred and forty-two were aged 50 years or younger (the younger group), while 306 were above 50 years of age (the older group). The most common pre-existing conditions in the younger group were diabetes mellitus and hypertension, and 69.7% of the patients had a body mass index (BMI) > 25 kg/m 2 . Of 142 younger patients, 31 of 142 patients (21.8%, 19 women) did not have these pre-existing conditions. The overall case fatality rate among severity cases was 21.0%, and it differed according to age: 5.6% (n = 8/142) in the younger group, 28.1% in the older group, and 38% in the ≥ 65 years group. Age (odds ratio [OR], 7.902; 95% confidence interval [CI], 2.754–18.181), mechanical ventilation therapy (OR, 17.233; 95% CI, 8.439–35.192), highest creatinine > 1.5 mg/dL (OR, 17.631; 95% CI, 8.321–37.357), and combined blood stream infection (OR, 7.092; 95% CI, 1.061–18.181) were identified as independent predictors of mortality in total patients. Similar patterns were observed in age-specific analyses, but most results were statistically insignificant in multivariate analysis due to the low number of deaths in the younger group.The full vaccination rate was very low among study population (13.6%), and only three patients were fully vaccinated, with none of the patients who died having been fully vaccinated in the younger group. Seven of eight patients who died had a pre-existing condition or were obese (BMI > 25 kg/m 2 ), and the one remaining patient died from a secondary infection.
Conclusion
About 22% of the patients in the young critical group did not have an underlying disease or obesity, but the rate of obesity (BMI > 25 kg/m2 ) was high, with a fatality rate of 5.6%. The full vaccination rate was extremely low compared to the general population of the same age group, showing that non-vaccination has a grave impact on the progression of COVID-19 to a critical condition. The findings of this study highlight the need for measures to prevent critical progression of COVID-19, such as vaccinations and targeting young adults especially having risk factors.
Keyword
Figure
Reference
-
1. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020; 579(7798):270–273. PMID: 32015507.2. World Health Organization. WHO announces COVID-19 outbreak a pandemic. Updated 2020. Accessed 12 March, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200509covid-19-sitrep-110.pdf?sfvrsn=3b92992c_6 .3. World Health Organization. WHO Coronavirus (COVID-19) dashboard. Updated 2022. Accessed January 29, 2022. https://covid19.who.int/ .4. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180(7):934–943. PMID: 32167524.5. Jang JG, Hur J, Choi EY, Hong KS, Lee W, Ahn JH. Prognostic factors for severe coronavirus disease 2019 in Daegu, Korea. J Korean Med Sci. 2020; 35(23):e209. PMID: 32537954.6. Kang SJ, Jung SI. Age-related morbidity and mortality among patients with COVID-19. Infect Chemother. 2020; 52(2):154–164. PMID: 32537961.7. Heald-Sargent T, Muller WJ, Zheng X, Rippe J, Patel AB, Kociolek LK. Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr. 2020; 174(9):902–903. PMID: 32745201.8. Murillo-Zamora E, Aguilar-Sollano F, Delgado-Enciso I, Hernandez-Suarez CM. Predictors of laboratory-positive COVID-19 in children and teenagers. Public Health. 2020; 189:153–157. PMID: 33246302.9. Steinberg E, Wright E, Kushner B. In young adults with COVID-19, obesity is associated with adverse outcomes. West J Emerg Med. 2020; 21(4):752–755. PMID: 32726235.10. Lu Y, Huang Z, Wang M, Tang K, Wang S, Gao P, et al. Clinical characteristics and predictors of mortality in young adults with severe COVID-19: a retrospective observational study. Ann Clin Microbiol Antimicrob. 2021; 20(1):3. PMID: 33407543.11. Muschitz C, Trummert A, Berent T, Laimer N, Knoblich L, Bodlaj G, et al. Attenuation of COVID-19-induced cytokine storm in a young male patient with severe respiratory and neurological symptoms. Wien Klin Wochenschr. 2021; 133(17-18):973–978. PMID: 33905029.12. Singanayagam A, Hakki S, Dunning J, Madon KJ, Crone MA, Koycheva A, et al. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. Lancet Infect Dis. 2022; 22(2):183–195. PMID: 34756186.13. Korea Disease Control and Prevention Agency. COVID-19 domestic outbreaks. Updated 2022. Accessed February 3, 2022. http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=5641&contSeq=5641&board_id=312&gubun=ALL .14. Lee JY, Kim HA, Huh K, Hyun M, Rhee JY, Jang S, et al. Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID-19 in Korea. J Korean Med Sci. 2020; 35(23):e223. PMID: 32537957.15. Liu Z, Liu J, Ye L, Yu K, Luo Z, Liang C, et al. Predictors of mortality for hospitalized young adults aged less than 60 years old with severe COVID-19: a retrospective study. J Thorac Dis. 2021; 13(6):3628–3642. PMID: 34277055.16. Mohamed MS, Moulin TC, Schiöth HB. Sex differences in COVID-19: the role of androgens in disease severity and progression. Endocrine. 2021; 71(1):3–8. PMID: 33179220.17. Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res. 2020; 116(14):2197–2206. PMID: 33063089.18. Capuzzo M, Amaral AC, Liu VX. Assess COVID-19 prognosis … but be aware of your instrument’s accuracy! Intensive Care Med. 2021; 47(12):1472–1474. PMID: 34608529.19. He F, Page JH, Weinberg KR, Mishra A. The development and validation of simplified machine learning algorithms to predict prognosis of hospitalized patients with COVID-19: multicenter, retrospective study. J Med Internet Res. 2022; 24(1):e31549. PMID: 34951865.20. Korea Disease Control and Prevention Agency. Vaccination situation dashboard, Korea. Accessed January 31, 2022. https://www.korea.kr/news/pressReleaseView.do?newsId=156483536 .21. Korea Disease Control and Prevention Agency. July vaccination plan. Updated 2022. Accessed February 5, 2022. http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=5626&contSeq=5626&board_id=312&gubun=ALL .22. Newsis. "The person who got third dose vaccination is 92% risk reduction to severe COVID-19 than those who haven't been vaccinated," the authorities said. Updated 2022. Accessed February 04, 2022. https://news.nate.com/view/20220203n22126?mid=n0412 .23. Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021; 397(10287):1819–1829. PMID: 33964222.24. Self WH, Tenforde MW, Rhoads JP, Gaglani M, Ginde AA, Douin DJ, et al. Comparative effectiveness of Moderna, Pfizer-BioNTech, and Janssen (Johnson & Johnson) vaccines in preventing COVID-19 hospitalizations among adults without immunocompromising conditions - United States, March-August 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(38):1337–1343. PMID: 34555004.25. Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022; 114:252–260. PMID: 34800687.26. Liu Q, Qin C, Liu M, Liu J. Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: a systematic review and meta-analysis. Infect Dis Poverty. 2021; 10(1):132. PMID: 34776011.27. If you don’t get vaccinated, your daily life will be tied up. “Actually forced to get vaccinated.” Anti-vaccinators, “Resistance.”. Updated 2021. Accessed February 3, 2022. https://blog.naver.com/fascina1103/222585969631 .28. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363(9403):157–163. PMID: 14726171.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics and Risk Factors for Mortality in Critical COVID-19 Patients Aged 50 Years or Younger During Omicron Wave in Korea: Comparison With Patients Older Than 50 Years of Age
- Characteristics of Critically Ill COVID-19 Patients in Busan, Republic of Korea
- Herpes Zoster Ophthalmicus in Patients Younger than 50 Years Versus 50 Years and Older
- Clinical Characteristics and Risk Factors in Severely Injured Elderly Trauma Presenting to Emergency Department
- Vaccination Status and In-hospital Mortality Among Adults With COVID-19 in Jakarta, Indonesia: A Retrospective Hospital-based Cohort Study