Diabetes Metab J.
2022 May;46(3):427-438. 10.4093/dmj.2021.0105.
Association of Metabolic Syndrome with COVID-19 in the Republic of Korea
- Affiliations
-
- 1Department of Preventive Medicine, College of Medicine, Kyung Hee University, Seoul, Korea
- 2Department of Medical Education and Humanities, College of Medicine, Kyung Hee University, Seoul, Korea
- KMID: 2530182
- DOI: http://doi.org/10.4093/dmj.2021.0105
Abstract
- Background
Metabolic syndrome (MetS) is reportedly a crucial risk factor for coronavirus disease 2019 (COVID-19). Since the epidemiological studies that examine this association are few and include small samples, we investigated the relationship between MetS and COVID-19 severity and death using a larger sample in the Republic of Korea.
Methods
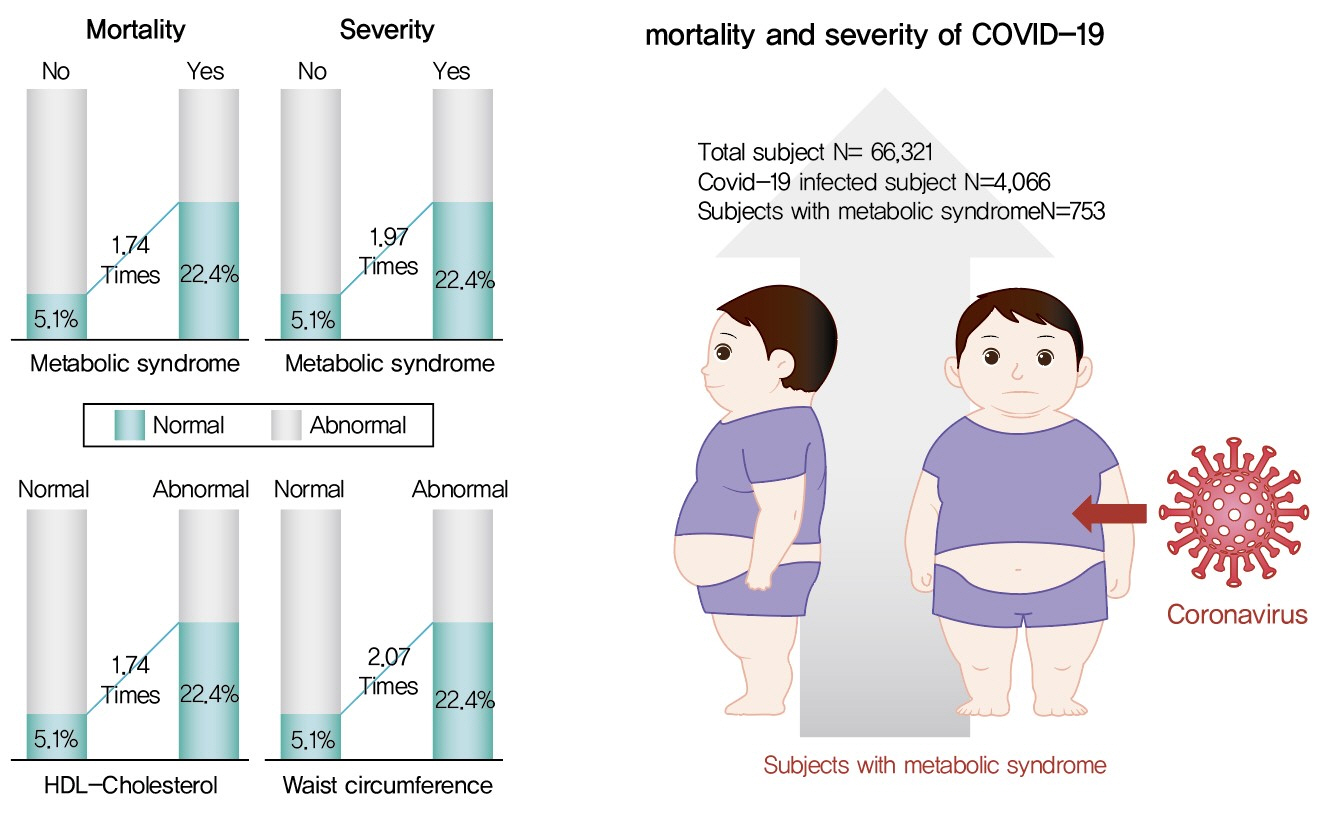
We analyzed 66,321 patients, 4,066 of whom had COVID-19. We used chi-square tests to examine patients’ characteristics. We performed logistic regression analysis to analyze differences in COVID-19 infection and clinical outcomes according to the presence of MetS.
Results
Although MetS was not significantly associated with COVID-19 risk, acquiring MetS was significantly associated with the risk of severe COVID-19 outcomes (odds ratio [OR], 1.97; 95% confidence interval [CI], 1.34 to 2.91; P=0.001). The mortality risk was significantly higher in COVID-19 patients with MetS (OR, 1.74; 95% CI, 1.17 to 2.59; P=0.006). Patients with abnormal waist circumference were approximately 2.07 times more likely to develop severe COVID-19 (P<0.001), and high-density lipoprotein cholesterol (HDL-C) levels were significantly associated with COVID-19; the mortality risk due to COVID-19 was 1.74 times higher in men with an HDL-C level of <40 mg/dL and in women with an HDL-C level of <50 mg/dL (P=0.012).
Conclusion
COVID-19 is likely associated with severity and death in patients with MetS or in patients with MetS risk factors. Therefore, patients with MetS or those with abnormal waist circumference and HDL-C levels need to be treated with caution.
Keyword
Figure
Cited by 1 articles
-
Associated Factors with Changes of Metabolic Abnormalities among General Population in COVID-19 Pandemic
Eunjoo Kwon, Eun-Hee Nah, Suyoung Kim, Seon Cho, Hyeran Park
Korean J Health Promot. 2023;23(2):55-64. doi: 10.15384/kjhp.2023.23.2.55.
Reference
-
1. World Health Organization: Coronavirus disease (COVID-19): situation report 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (cited 2021 Oct 27).2. Korea Centers for Disease Control & Prevention: The updates on COVID-19 in Korea as of 13 January. Available from: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=4620&contSeq=4620&board_id=312&gubun=ALL#/ (cited 2021 Oct 27).3. Aggarwal G, Cheruiyot I, Aggarwal S, Wong J, Lippi G, Lavie CJ, et al. Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: a meta-analysis. Curr Probl Cardiol. 2020; 45:100617.
Article4. Ssentongo P, Ssentongo AE, Heilbrunn ES, Ba DM, Chinchilli VM. Association of cardiovascular disease and 10 other preexisting comorbidities with COVID-19 mortality: a systematic review and meta-analysis. PLoS One. 2020; 15:e0238215.
Article5. GBD 2019 Viewpoint Collaborators. Five insights from the Global Burden of Disease Study 2019. Lancet. 2020; 396:1135–59.6. Kim MH, Lee SH, Shin KS, Son DY, Kim SH, Joe H, et al. The change of metabolic syndrome prevalence and its risk factors in Korean adults for decade: Korea National Health and Nutrition Examination Survey for 2008-2017. Korean J Fam Pract. 2020; 10:44–52.
Article7. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006; 119:812–9.
Article8. Malik S, Wong ND, Franklin SS, Kamath TV, L’Italien GJ, Pio JR, et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004; 110:1245–50.
Article9. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005; 28:1769–78.10. Xie J, Zu Y, Alkhatib A, Pham TT, Gill F, Jang A, et al. Metabolic syndrome and COVID-19 mortality among adult black patients in New Orleans. Diabetes Care. 2020; 44:188–93.
Article11. Yanai H. Metabolic syndrome and COVID-19. Cardiol Res. 2020; 11:360–5.
Article12. Enkhtur A, Yoon JS, Lee CW. Factors increasing the risk of mortality and morbidity due to coronavirus infection in patients with metabolic syndrome. Precis Future Med. 2020; 4:83–90.
Article13. Huh JH, Kang DR, Jang JY, Shin JH, Kim JY, Choi S, et al. Metabolic syndrome epidemic among Korean adults: Korean survey of cardiometabolic syndrome (2018). Atherosclerosis. 2018; 277:47–52.
Article14. National Health Insurance: National Health Insurance Sharing Service 2020. Available from: https://nhiss.nhis.or.kr/bd/ay/bdaya001iv.do (cited 2021 Oct 27).15. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; 173:676–82.
Article16. Ghoneim S, Butt MU, Hamid O, Shah A, Asaad I. The incidence of COVID-19 in patients with metabolic syndrome and non-alcoholic steatohepatitis: a population-based study. Metabol Open. 2020; 8:100057.
Article17. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020; 323:1775–6.
Article18. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. COVID-19 in critically ill patients in the Seattle region: case series. N Engl J Med. 2020; 382:2012–22.
Article19. Lee JS, Park S, Jeong HW, Ahn JY, Choi SJ, Lee H, et al. Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19. Sci Immunol. 2020; 5:e. abd1554.
Article20. Ridker PM. High-sensitivity C-reactive protein: potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation. 2001; 103:1813–8.
Article21. An YB. Association between serum adiponectin concentration and the onset of metabolic syndrome (Korean Endocrine Society 19: 492–500, 2004, Park SS and 12 others). Endocrinol Metab. 2005; 20:103–4.22. Alamdari NM, Rahimi FS, Afaghi S, Zarghi A, Qaderi S, Tarki FE, et al. The impact of metabolic syndrome on morbidity and mortality among intensive care unit admitted COVID-19 patients. Diabetes Metab Syndr. 2020; 14:1979–86.
Article23. Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002; 75:683–8.
Article24. Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from Shaping America’s Health. Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am J Clin Nutr. 2007; 85:1197–202.
Article25. Peters SAE, MacMahon S, Woodward M. Obesity as a risk factor for COVID-19 mortality in women and men in the UK biobank: comparisons with influenza/pneumonia and coronary heart disease. Diabetes Obes Metab. 2021; 23:258–62.
Article26. Zhu Z, Hasegawa K, Ma B, Fujiogi M, Camargo CA Jr, Liang L. Association of obesity and its genetic predisposition with the risk of severe COVID-19: analysis of population-based cohort data. Metabolism. 2020; 112:154345.
Article27. Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, et al. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020; 21:e13128.
Article28. Wadman M. Why obesity worsens COVID-19. Science. 2020; 369:1280–1.
Article29. Wang G, Zhang Q, Zhao X, Dong H, Wu C, Wu F, et al. Low high-density lipoprotein level is correlated with the severity of COVID-19 patients: an observational study. Lipids Health Dis. 2020; 19:204.
Article30. Ding X, Zhang J, Liu L, Yuan X, Zang X, Lu F, et al. High-density lipoprotein cholesterol as a factor affecting virus clearance in covid-19 patients. Respir Med. 2020; 175:106218.
Article31. Sun JT, Chen Z, Nie P, Ge H, Shen L, Yang F, et al. Lipid profile features and their associations with disease severity and mortality in patients with COVID-19. Front Cardiovasc Med. 2020; 7:584987.
Article32. Kaji H. High-density lipoproteins and the immune system. J Lipids. 2013; 2013:684903.
Article33. McKechnie JL, Blish CA. The innate immune system: fighting on the front lines or fanning the flames of COVID-19? Cell Host Microbe. 2020; 27:863–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associated Factors with Changes of Metabolic Abnormalities among General Population in COVID-19 Pandemic
- Impact of COVID-19 on the clinical course of nephrotic syndrome in children: a single-center study
- Changes in Body Mass Index and Prevalence of Metabolic Syndrome during COVID-19 Lockdown Period
- Post-COVID-19 Syndrome
- Changes in the prevalence of metabolic syndrome in Korean adults after the COVID-19 outbreak