Obstet Gynecol Sci.
2022 May;65(3):244-255. 10.5468/ogs.22037.
Evaluation of mobile health applications for cervical cancer in the digital marketplace
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
- KMID: 2529827
- DOI: http://doi.org/10.5468/ogs.22037
Abstract
Objective
To assess the quality of mobile health (mHealth) applications (apps) for cervical cancer using the mobile app rating scale (MARS), APPLICATIONS scoring system, and app rating using specific statements.
Methods
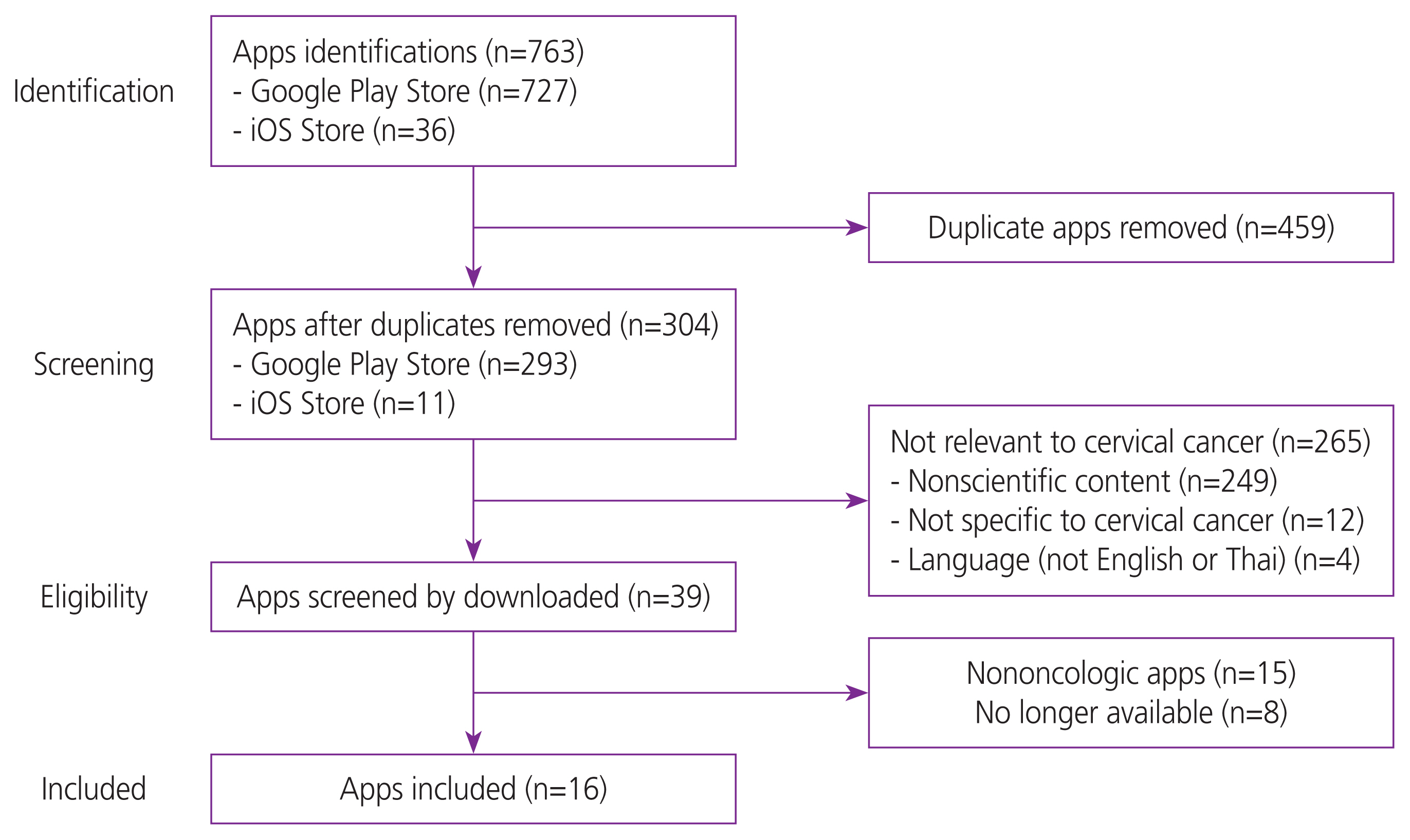
We searched for cervical cancer apps on two major mobile operating systems (Google Play Store and Apple iTunes Store) in March 2021. Eligible apps were downloaded and assessed for quality by two independent reviewers using multimodal assessment tools.
Results
The overall quality of the MARS score was 2.61±0.795. The highest scoring app was “The American Society for Colposcopy and Cervical Pathology (ASCCP) Management Guidelines” (3.98). Overall, apps scored highest in the functionality domain, followed by information, engagement, and aesthetics domains. The mean±standard deviation of the APPLICATIONS scoring system was 8.50±1.712. The highest-rated apps were “ASCCP Management Guidelines,” “The British Society for Colposcopy and Cervical Pathology (BSCCP),” and “Cervical Cancer Guide.” Apps scored the highest in the paid subscription and price domains. By contrast, apps scored poorly in the text search, literature, and subjective presentation domains. Concerning app content, many apps infrequently provided misconceptions regarding cervical cancer. The apps’ rating using specific statements was 7.81±4.562.
Conclusion
Overall, the apps analyzed using the MARS and APPLICATIONS scoring systems demonstrated above-average quality. However, there is a need to improve the essential information conveyed by these applications. Moreover, the assessment tools have influenced different app quality rating results, confirming the lack of standardized quality assessment tools for mHealth apps.
Figure
Cited by 1 articles
-
Diagnostic accuracy of hand-held colposcope (Gynocular) in comparison with standard colposcope in patients with abnormal cervical cytology or visual inspection with acetic acid positivity: a cross over randomized controlled study
Sowmiya Jayabalan, Murali Subbaiah, Latha Chaturvedula
Obstet Gynecol Sci. 2023;66(4):300-306. doi: 10.5468/ogs.23089.
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.
Article2. Medical Record and Databased Cancer Unit. Cancer in Thailand Vol X 2016 2018 [Internet]. Bangkok: National Cancer Institute Medical Record and Databased, Medical Digital Division;c2021. [cited 2021 Aug 17]. Available from: https://www.nci.go.th/e_book/cit_x/index.html .3. Bogale AL, Teklehaymanot T, Haidar Ali J, Kassie GM. Knowledge, attitude and practice of cervical cancer screening among women infected with HIV in Africa: systematic review and meta-analysis. PLoS One. 2021; 16:e0249960.
Article4. Osei EA, Appiah S, Gaogli JE, Oti-Boadi E. Knowledge on cervical cancer screening and vaccination among females at Oyibi community. BMC Womens Health. 2021; 21:148.
Article5. Weng Q, Jiang J, Haji FM, Nondo LH, Zhou H. Women’s knowledge of and attitudes toward cervical cancer and cervical cancer screening in Zanzibar, Tanzania: a cross-sectional study. BMC Cancer. 2020; 20:63.
Article6. Likitdee N, Kietpeerakool C, Chumworathayi B, Temtanakitpaisan A, Aue-Aungkul A, Nhokaew W, et al. Knowledge and attitude toward human papillomavirus infection and vaccination among Thai women: a nationwide social media survey. Asian Pac J Cancer Prev. 2020; 21:2895–902.
Article7. Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N. Barriers to the use of mobile health in improving health outcomes in developing countries: systematic review. J Med Internet Res. 2019; 21:e13263.
Article8. Salmani H, Ahmadi M, Shahrokhi N. The impact of mobile health on cancer screening: a systematic review. Cancer Inform. 2020; 19:1176935120954191.
Article9. Charbonneau DH, Hightower S, Katz A, Zhang K, Abrams J, Senft N, et al. Smartphone apps for cancer: a content analysis of the digital health marketplace. Digit Health. 2020; 6:2055207620905413.
Article10. Ana FA, Loreto MS, José LM, Pablo SM, María Pilar MJ, Myriam SA. Mobile applications in oncology: a systematic review of health science databases. Int J Med Inform. 2019; 133:104001.
Article11. Kessel KA, Vogel MME, Schmidt-Graf F, Combs SE. Mobile apps in oncology: a survey on health care professionals’ attitude toward telemedicine, mhealth, and oncological apps. J Med Internet Res. 2016; 18:e312.
Article12. Böhme C, von Osthoff MB, Frey K, Hübner J. Qualitative evaluation of mobile cancer apps with particular attention to the target group, content, and advertising. J Cancer Res Clin Oncol. 2018; 144:173–81.
Article13. Upadhyay VA, Landman AB, Hassett MJ. Landscape analysis of oncology mobile health applications. JCO Clin Cancer Inform. 2021; 5:579–87.
Article14. DeNicola N, Marko K. Connected health and mobile apps in obstetrics and gynecology. Obstet Gynecol Clin North Am. 2020; 47:317–31.
Article15. Brouard B, Bardo P, Bonnet C, Mounier N, Vignot M, Vignot S. Mobile applications in oncology: is it possible for patients and healthcare professionals to easily identify relevant tools? Ann Med. 2016; 48:509–15.
Article16. Farag S, Fields J, Pereira E, Chyjek K, Chen KT. Identification and rating of gynecologic oncology applications using the APPLICATIONS scoring system. Telemed J E Health. 2016; 22:1001–7.
Article17. US Food and Drug Administration. Policy for device software functions and mobile medical applications: guidance for industry and food and drug administration staff [Internet]. Washington, D.C: U.S. Food and Drug Administration;c2019. [cited 2021 Aug 17]. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/policy-device-software-functions-and-mobile-medical-applications .18. Shin MB, Liu G, Mugo N, Garcia PJ, Rao DW, Bayer CJ, et al. A framework for cervical cancer elimination in low-and-middle-income countries: a scoping review and roadmap for interventions and research priorities. Front Public Health. 2021; 9:670032.
Article19. Bhochhibhoya S, Dobbs PD, Maness SB. Interventions using mHealth strategies to improve screening rates of cervical cancer: a scoping review. Prev Med. 2021; 143:106387.
Article20. Lee YH, Huang LH, Chen SH, Shao JH, Lai CH, Yang NP. Effects of mobile application program (App)-assisted health education on preventive behaviors and cancer literacy among women with cervical intraepithelial neoplasia. Int J Environ Res Public Health. 2021; 18:11603.
Article21. Munoz-Zuluaga CA, Gallo-Pérez JD, Pérez-Bustos A, Orozco-Urdaneta M, Druffel K, Cordoba-Astudillo LP, et al. Mobile applications: breaking barriers to early breast and cervical cancer detection in underserved communities. JCO Oncol Pract. 2021; 17:e323–35.
Article22. Amor-García MÁ, Collado-Borrell R, Escudero-Vilaplana V, Melgarejo-Ortuño A, Herranz-Alonso A, Arranz Arija JÁ, et al. Assessing apps for patients with genitourinary tumors using the mobile application rating scale (MARS): systematic search in app stores and content analysis. JMIR Mhealth Uhealth. 2020; 8:e17609.
Article23. Jupp JCY, Sultani H, Cooper CA, Peterson KA, Truong TH. Evaluation of mobile phone applications to support medication adherence and symptom management in oncology patients. Pediatr Blood Cancer. 2018; 65:e27278.
Article24. Stoyanov SR, Hides L, Kavanagh DJ, Zelenko O, Tjondronegoro D, Mani M. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015; 3:e27.
Article25. Farag S, Chyjek K, Chen KT. Identification of iPhone and iPad applications for obstetrics and gynecology providers. Obstet Gynecol. 2014; 124:941–5.
Article26. Sedhom R, McShea MJ, Cohen AB, Webster JA, Mathews SC. Mobile app validation: a digital health scorecard approach. NPJ Digit Med. 2021; 4:111.
Article27. Hongsanun W, Insuk S. Quality assessment criteria for mobile health apps: a systematic review. Walailak J Sci & Tech. 2020; 17:745–59.
Article28. StatCounter Global Stats. Mobile operating system market share worldwide–August 2021 [Internet]. Dublin: Statcounter;c2021. [cited 2021 Aug 17]. Available from: http://gs.ststcounter.com/os-market-share/mobile/world-wide .29. Stoyanov SR. MARS training video [Internet]. Stoyan Stoyanov. c2016. [cited 2021 Aug 17]. Available from: https://www.youtube.com/watch?v=25vBwJQIOcE .30. Kietpeerakool C, Phianmongkhol Y, Jitvatcharanun K, Siriratwatakul U, Srisomboon J. Knowledge, awareness, and attitudes of female sex workers toward HPV infection, cervical cancer, and cervical smears in Thailand. Int J Gynaecol Obstet. 2009; 107:216–9.
Article31. Lu DJ, Girgis M, David JM, Chung EM, Atkins KM, Kamrava M. Evaluation of mobile health applications to track patient-reported outcomes for oncology patients: a systematic review. Adv Radiat Oncol. 2020; 6:100576.
Article32. Ghalavandi S, Heidarnia A, Zarei F, Beiranvand R. Knowledge, attitude, practice, and self-efficacy of women regarding cervical cancer screening. Obstet Gynecol Sci. 2021; 64:216–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current status and future direction of digital health in Korea
- Qualitative assessment of atopic dermatitis-related mobile applications in Korea
- The Perception of Laymen and Experts Toward Mobile Applications for Self-monitoring of Diet Based on in-depth Interviews and Focus Group Interviews
- Construction and Performance Evaluation of Digital Radiographic System
- Quality Evaluation of Online Health Information Related to Young Child