J Korean Med Sci.
2022 May;37(18):e145. 10.3346/jkms.2022.37.e145.
Prognostic Value of Estimated Plasma Volume Status in Patients With Sepsis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2529711
- DOI: http://doi.org/10.3346/jkms.2022.37.e145
Abstract
- Background
In patients with sepsis, timely risk stratification is important to improve prognosis. Although several clinical scoring systems are currently being used to predict the outcome of sepsis, but they all have certain limitations. The objective of this study was to evaluate the prognostic value of estimated plasma volume status (ePVS) in patients admitted to the intensive care unit (ICU) with sepsis or septic shock.
Methods
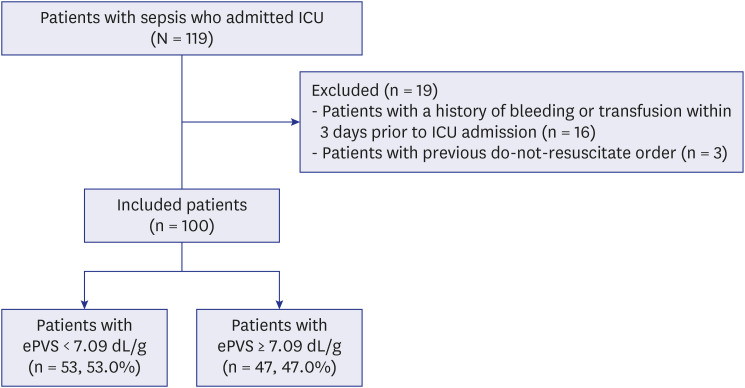
This single-center, prospective observational study, included 100 patients admitted to the ICU with sepsis or septic shock. Informed consent, blood samples, and co-morbidity data were obtained from the patients on admission, and the severity of sepsis was recorded. The primary outcome was in-hospital mortality and multivariable logistic regression analysis was used to adjust for confounding factors to determine the significant prognostic factor.
Results
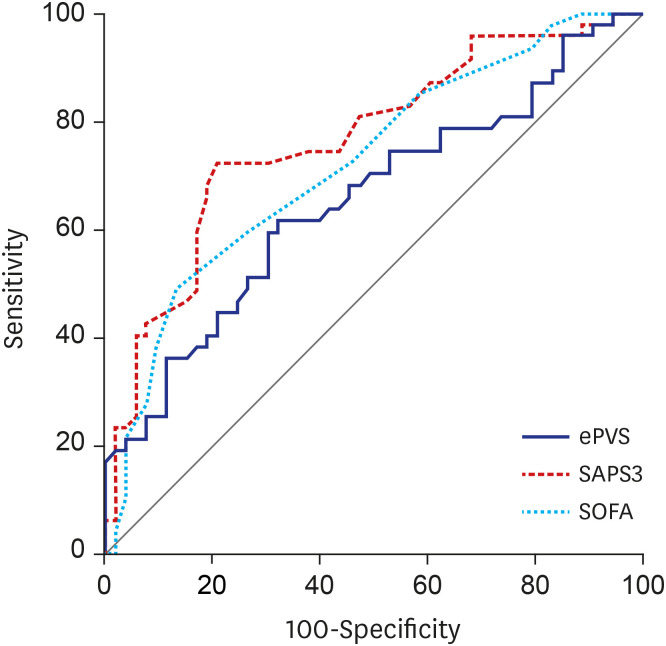
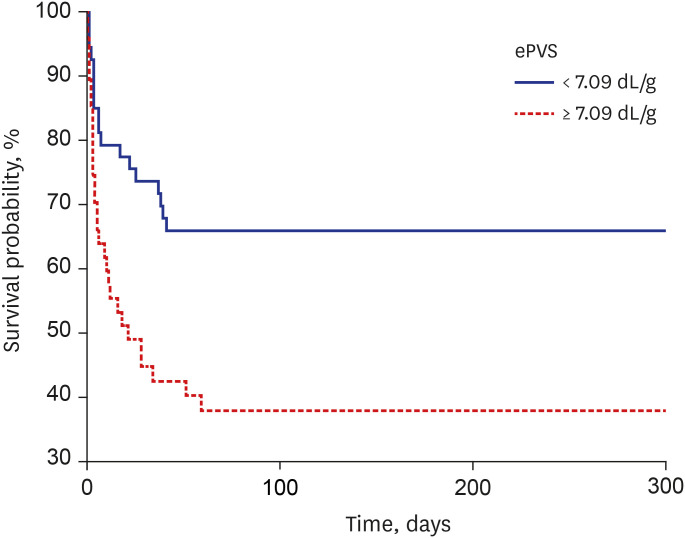
The in-hospital mortality was 47%. The ePVS was correlated with the amount of total fluids administered 24 hours before the ICU admission. The mean ePVS in patients who died was higher than in those who survived (7.7 ± 2.1 dL/g vs. 6.6 ± 1.6 dL/g, P = 0.003). To evaluate the utility of ePVS in predicting in-hospital mortality, a receiver operating characteristic curve was produced. Sensitivity and specificity were optimal at a cut-off point of 7.09 dL/g, with an area under the curve of 0.655. In the multivariate analysis, higher ePVS was significantly associated with higher in-hospital mortality adjusted odds ratio, 1.39; 95% confidence interval, 1.04–1.85, P = 0.028). The Kaplan-Meier curve showed that an ePVS value above 7.09 was associated with an increased risk of in-hospital mortality compared with the rest of the population (P = 0.004).
Conclusion
The ePVS was correlated with the amount of intravenous fluid resuscitation and may be used as a simple and novel prognostic factor in patients with sepsis or septic shock who are admitted to the ICU.
Figure
Reference
-
1. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016; 315(8):801–810. PMID: 26903338.2. Quartin AA, Calonge RO, Schein RM, Crandall LA. Influence of critical illness on physicians’ prognoses for underlying disease: a randomized study using simulated cases. Crit Care Med. 2008; 36(2):462–470. PMID: 18176316.3. Ince C, Mayeux PR, Nguyen T, Gomez H, Kellum JA, Ospina-Tascón GA, et al. The endothelium in sepsis. Shock. 2016; 45(3):259–270. PMID: 26871664.4. Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. 2015; 19(1):251. PMID: 26073560.5. Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021; 49(11):e1063–e1143. PMID: 34605781.6. Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011; 39(2):259–265. PMID: 20975548.7. Miller WL. Fluid volume overload and congestion in heart failure: time to reconsider pathophysiology and how volume is assessed. Circ Heart Fail. 2016; 9(8):e002922. PMID: 27436837.8. Duarte K, Monnez JM, Albuisson E, Pitt B, Zannad F, Rossignol P. Prognostic value of estimated plasma volume in heart failure. JACC Heart Fail. 2015; 3(11):886–893. PMID: 26541787.9. Kobayashi M, Rossignol P, Ferreira JP, Aragão I, Paku Y, Iwasaki Y, et al. Prognostic value of estimated plasma volume in acute heart failure in three cohort studies. Clin Res Cardiol. 2019; 108(5):549–561. PMID: 30341579.10. Huang CY, Lin TT, Wu YF, Chiang FT, Wu CK. Long-term prognostic value of estimated plasma volume in heart failure with preserved ejection fraction. Sci Rep. 2019; 9(1):14369. PMID: 31591412.11. Turcato G, Zaboli A, Ciccariello L, Pfeifer N. Estimated plasma volume status (ePVS) could be an easy-to-use clinical tool to determine the risk of sepsis or death in patients with fever. J Crit Care. 2020; 58:106–112. PMID: 32422322.12. Chouihed T, Rossignol P, Bassand A, Duarte K, Kobayashi M, Jaeger D, et al. Diagnostic and prognostic value of plasma volume status at emergency department admission in dyspneic patients: results from the PARADISE cohort. Clin Res Cardiol. 2019; 108(5):563–573. PMID: 30370469.13. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.14. Pittard MG, Huang SJ, McLean AS, Orde SR. Association of positive fluid balance and mortality in sepsis and septic shock in an Australian cohort. Anaesth Intensive Care. 2017; 45(6):737–743. PMID: 29137585.15. Hippensteel JA, Uchimido R, Tyler PD, Burke RC, Han X, Zhang F, et al. Intravenous fluid resuscitation is associated with septic endothelial glycocalyx degradation. Crit Care. 2019; 23(1):259. PMID: 31337421.16. Bateman RM, Sharpe MD, Jagger JE, Ellis CG. Sepsis impairs microvascular autoregulation and delays capillary response within hypoxic capillaries. Crit Care. 2015; 19(1):389. PMID: 26537126.17. Ince C. The microcirculation is the motor of sepsis. Crit Care. 2005; 9(Suppl 4):S13–S19. PMID: 16168069.18. Strauss MB, Davis RK, Rosenbaum JD, Rossmeisl EC. Water diuresis produced during recumbency by the intravenous infusion of isotonic saline solution. J Clin Invest. 1951; 30(8):862–868. PMID: 14861307.19. Fudim M, Miller WL. Calculated estimates of plasma volume in patients with chronic heart failure-comparison with measured volumes. J Card Fail. 2018; 24(9):553–560. PMID: 30098381.20. Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009; 76(4):422–427. PMID: 19436332.21. Koch T, Geiger S, Ragaller MJ. Monitoring of organ dysfunction in sepsis/systemic inflammatory response syndrome: novel strategies. J Am Soc Nephrol. 2001; 12(Suppl 17):S53–S59. PMID: 11251033.22. Miranda M, Balarini M, Caixeta D, Bouskela E. Microcirculatory dysfunction in sepsis: pathophysiology, clinical monitoring, and potential therapies. Am J Physiol Heart Circ Physiol. 2016; 311(1):H24–H35. PMID: 27106039.23. Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, et al. SAPS3--From evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005; 31(10):1345–1355. PMID: 16132892.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Amino Acid Derangements in Plasma and Erythrocytes of Patients with Sepsis
- Changes in Plasma Levels of Natural Anticoagulants in Disseminated Intravascular Coagulation: High Prognostic Value of Antithrombin and Protein C in Patients with Underlying Sepsis or Severe Infection
- Blood Volume of Rabbit Eye
- Assessment of Dry Body Weight in Maintenance Hemodialysis Patients by Plasma Levels of ANP and cGMP
- Correlation of Nitric Oxide and Corticosteroids Along the Course of Sepsis