Ann Rehabil Med.
2022 Apr;46(2):97-107. 10.5535/arm.22010.
Early Return to Play After Anterior Cruciate Ligament Reconstruction: Is It Worth the Risk?
- Affiliations
-
- 1Department of Sports Medicine, University of Szeged, Szeged, Hungary
- 2Department of Traumatology, University of Szeged, Szeged, Hungary
- 3Department of Kinesiology, University of Physical Education, Budapest, Hungary
- 4Department of Medical Physics and Informatics, University of Szeged, Szeged, Hungary
- KMID: 2529510
- DOI: http://doi.org/10.5535/arm.22010
Abstract
Objective
To compare the outcomes of a 6-month-long accelerated rehabilitation with a 12-month-long rehabilitation. There is no consensus on the optimal duration of rehabilitation after anterior cruciate ligament reconstruction (ACLR). Trends in the past decades have shifted towards accelerated programs, often resulting in a return to play (RTP) at 4–6 months, postoperatively. However, longer rehabilitation cycles have recently experienced renaissance due to a greater understanding of graft remodeling.
Methods
Adult athletes who underwent ACLR between 2015 and 2018 by the same surgeon were included and followed-up prospectively for 24 months. Participants were allocated into two groups based on their RTP (6 months vs. 12 months) and compared with graft elongation, reoperation rate, and sports career (quit or continue) outcomes.
Results
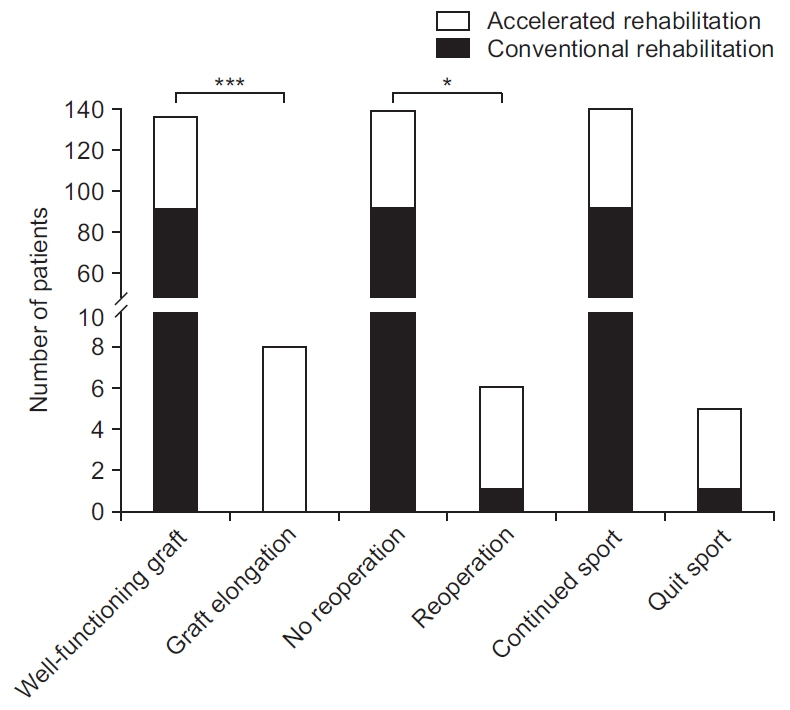
Fifty-four patients underwent accelerated rehabilitation and 92 completed conventional rehabilitation. The accelerated rehabilitation was significantly associated with graft elongation—the accelerated rehabilitation group (n=9) and the conventional rehabilitation group (n=0), p<0.001—and need for reoperation—the accelerated rehabilitation group (n=5) and the conventional rehabilitation group (n=1), p=0.026. Although the relationship between rehabilitation time and quitting competitive sports did not reach significance at 0.05 level (p=0.063), it was significant when p<0.1, thereby showing a clear trend.
Conclusion
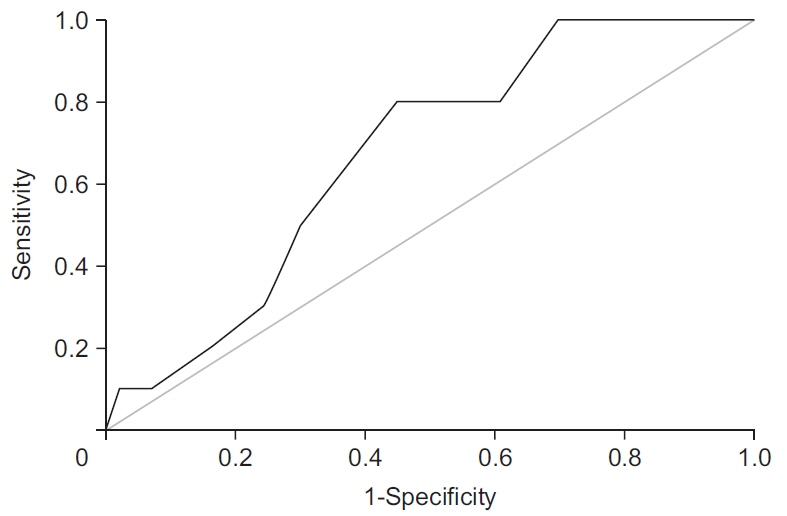
Accelerated rehabilitation increased graft elongation risk. Knee laxity ≥3 mm measured at 6 months after ACLR should be accompanied by RTP time frame re-evaluation. Arthrometry checkups or routine magnetic resonance imaging shortly after RTP may be considered in cases of accelerated rehabilitation.
Figure
Reference
-
1. Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev. 2017; 1:398–408.
Article2. Brandl G, Ostermann RC, Pauzenberger L, Lobo C, Feichtinger X. Bone-on-bone anatomic patellar tendon graft anterior cruciate ligament reconstruction: a reproducible technique combining press-fit and extracortical fixation. Arthrosc Tech. 2020; 9:e205–12.
Article3. Iio K, Tsuda E, Tsukada H, Yamamoto Y, Maeda S, Naraoka T, et al. Characteristics of elongated and ruptured anterior cruciate ligament grafts: an analysis of 21 consecutive revision cases. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2017; 8:1–7.
Article4. Sanders TL, Pareek A, Hewett TE, Levy BA, Dahm DL, Stuart MJ, et al. Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2017; 25:222–8.
Article5. Raines BT, Naclerio E, Sherman SL. Management of anterior cruciate ligament injury: what’s in and what’s out? Indian J Orthop. 2017; 51:563–75.6. Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015; 3:220–40.7. Ellman MB, Sherman SL, Forsythe B, LaPrade RF, Cole BJ, Bach BR Jr. Return to play following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015; 23:283–96.
Article8. Flagg KY, Karavatas SG, Thompson S Jr, Bennett C. Current criteria for return to play after anterior cruciate ligament reconstruction: an evidence-based literature review. Ann Transl Med. 2019; 7(Suppl 7):S252.
Article9. Menetrey J, Duthon VB, Laumonier T, Fritschy D. “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc. 2008; 16:224–31.
Article10. Mayr HO, Stoehr A, Herberger KT, Haasters F, Bernstein A, Schmal H, et al. Histomorphological alterations of human anterior cruciate ligament grafts during mid-term and long-term remodeling. Orthop Surg. 2021; 13:314–20.
Article11. American College of Surgeons; Committee on Trauma. Descriptions of trauma center levels and their roles in a trauma system. Resources for optimal care of the injured. Chicago, IL: American College of Surgeons;2014. p. 16–23.12. Soto JM, Zhang Y, Huang JH, Feng DX. An overview of the American trauma system. Chin J Traumatol. 2018; 21:77–9.
Article13. van Melick N, van Cingel RE, Brooijmans F, Neeter C, van Tienen T, Hullegie W, et al. Evidence-based clini cal practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016; 50:1506–15.
Article14. Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017; 175:8–26.15. Grassi A, Bailey JR, Signorelli C, Carbone G, Tchonang Wakam A, Lucidi GA, et al. Magnetic resonance imaging after anterior cruciate ligament reconstruction: a practical guide. World J Orthop. 2016; 7:638–49.
Article16. Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013; 41:1808–12.
Article17. Kaeding CC, Aros B, Pedroza A, Pifel E, Amendola A, Andrish JT, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011; 3:73–81.
Article18. Noailles T, Chalopin A, Boissard M, Lopes R, Bouguennec N, Hardy A. Incidence and risk factors for cyclops syndrome after anterior cruciate ligament reconstruction: a systematic literature review. Orthop Traumatol Surg Res. 2019; 105:1401–5.
Article19. Decarlo MS, Shelbourne KD, McCarroll JR, Rettig AC. Traditional versus accelerated rehabilitation following ACL reconstruction: a one-year follow-up. J Orthop Sports Phys Ther. 1992; 15:309–16.
Article20. Zaffagnini S, Grassi A, Serra M, Marcacci M. Return to sport after ACL reconstruction: how, when and why? A narrative review of current evidence. Joints. 2015; 3:25–30.
Article21. Risberg MA, Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009; 37:1958–66.
Article22. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016; 44:1861–76.
Article23. Beynnon BD, Uh BS, Johnson RJ, Abate JA, Nichols CE, Fleming BC, et al. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005; 33:347–59.
Article24. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012; 28:526–31.
Article25. Beynnon BD, Johnson RJ, Fleming BC. The science of anterior cruciate ligament rehabilitation. Clin Orthop Relat Res. 2002; (402):9–20.
Article26. Arnoczky SP. Biology of ACL reconstructions: what happens to the graft? Instr Course Lect. 1996; 45:229–33.27. Raoul T, Klouche S, Guerrier B, El-Hariri B, Herman S, Gerometta A, et al. Are athletes able to resume sport at six-month mean follow-up after anterior cruciate ligament reconstruction? Prospective functional and psychological assessment from the French Anterior Cruciate Ligament Study (FAST) cohort. Knee. 2019; 26:155–64.
Article28. Marumo K, Saito M, Yamagishi T, Fujii K. The “ligamentization” process in human anterior cruciate ligament reconstruction with autogenous patellar and hamstring tendons: a biochemical study. Am J Sports Med. 2005; 33:1166–73.
Article29. Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry. Am J Sports Med. 2016; 44:331–6.
Article30. Sutherland K, Clatworthy M, Chang K, Rahardja R, Young SW. Risk factors for revision anterior cruciate ligament reconstruction and frequency with which patients change surgeons. Orthop J Sports Med. 2019; 7:2325967119880487.
Article31. Snaebjornsson T, Svantesson E, Sundemo D, Westin O, Sansone M, Engebretsen L, et al. Young age and high BMI are predictors of early revision surgery after primary anterior cruciate ligament reconstruction: a cohort study from the Swedish and Norwegian knee ligament registries based on 30,747 patients. Knee Surg Sports Traumatol Arthrosc. 2019; 27:3583–91.
Article32. Parkinson B, Robb C, Thomas M, Thompson P, Spald ing T. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2017; 45:1529–36.
Article33. Inderhaug E, Drogset JO, Lygre S, Gifstad T. No effect of graft size or body mass index on risk of revision after ACL reconstruction using hamstrings autograft. Knee Surg Sports Traumatol Arthrosc. 2020; 28:707–13.
Article34. Hsu WH, Fan CH, Yu PA, Chen CL, Kuo LT, Hsu RW. Effect of high body mass index on knee muscle strength and function after anterior cruciate ligament reconstruction using hamstring tendon autografts. BMC Musculoskelet Disord. 2018; 19:363.
Article35. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013; 29:1566–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ligament Reconstruction in Congenital Absence of the Anterior Cruciate Ligament: A Case Report
- Anterior Cruciate Ligament Reconstruction with Achilles Tendon Allograft
- The Effect of Cyclic Tensile Load on Various Tibial Fixation Techniques in Anterior Cruciate Ligament Reconstruction
- Open anterior cruciate ligament reconstruction using inside-out femoral drilling
- Anterior Cruciate Ligament Reconstruction: The Long Road from Science to Clinical Relevance