Acute Crit Care.
2022 Feb;37(1):84-93. 10.4266/acc.2021.00129.
Clinical characteristics and outcomes of critically ill COVID-19 patients in Sfax, Tunisia
- Affiliations
-
- 1Department of Intensive Care, Habib Bourguiba University Hospital, Sfax University, Sfax, Tunisia
- 2Department of Radiology, Habib Bourguiba University Hospital, Sfax University, Sfax, Tunisia
- 3Department of Anesthesiology, Habib Bourguiba University Hospital, Sfax University, Sfax, Tunisia
- 4Department of Emergency Medicine, Habib Bourguiba University Hospital, Sfax University, Sfax, Tunisia
- 5Department of Microbiology, Habib Bourguiba University Hospital, Sfax University, Sfax, Tunisia
- KMID: 2527910
- DOI: http://doi.org/10.4266/acc.2021.00129
Abstract
- Background
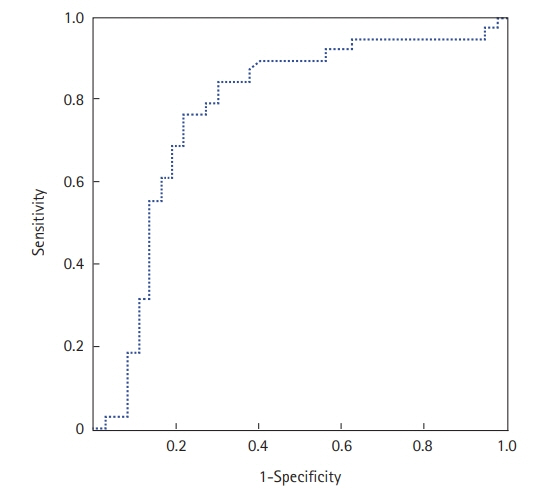
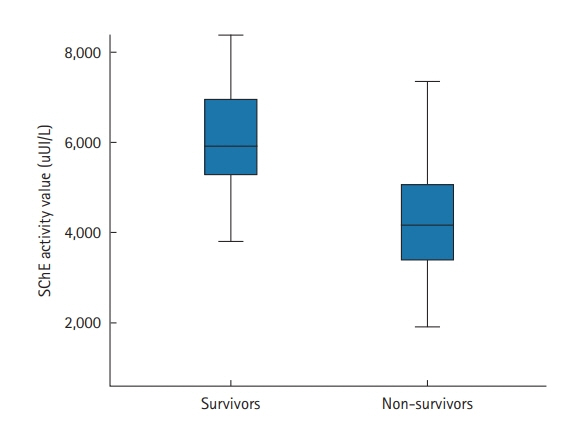
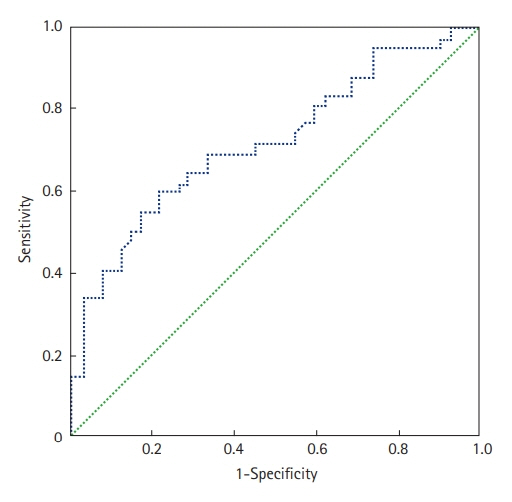
Africa, like the rest of the world, has been impacted by the coronavirus disease 2019 (COVID-19) pandemic. However, only a few studies covering this subject in Africa have been published. Methods: We conducted a retrospective study of critically ill adult COVID-19 patients—all of whom had a confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection— admitted to the intensive care unit (ICU) of Habib Bourguiba University Hospital (Sfax, Tunisia). Results: A total of 96 patients were admitted into our ICU for respiratory distress due to COVID-19 infection. Mean age was 62.4±12.8 years and median age was 64 years. Mean arterial oxygen tension (PaO2)/fractional inspired oxygen (FiO2) ratio was 105±60 and ≤300 in all cases but one. Oxygen support was required for all patients (100%) and invasive mechanical ventilation for 38 (40%). Prone positioning was applied in 67 patients (70%). Within the study period, 47 of the 96 patients died (49%). Multivariate analysis showed that the factors associated with poor outcome were the development of acute renal failure (odds ratio [OR], 6.7; 95% confidence interval [CI], 1.75–25.9), the use of mechanical ventilation (OR, 5.8; 95% CI, 1.54–22.0), and serum cholinesterase (SChE) activity lower than 5,000 UI/L (OR, 5.0; 95% CI, 1.34–19). Conclusions: In this retrospective cohort study of critically ill patients admitted to the ICU in Sfax, Tunisia, for acute respiratory failure following COVID-19 infection, the mortality rate was high. The development of acute renal failure, the use of mechanical ventilation, and SChE activity lower than 5,000 UI/L were associated with a poor outcome.
Keyword
Figure
Reference
-
1. Worldometer. Coronavirus update [Internet]. Worldometer;2020. [cited 2020 Jul 24]. Available from: https://www.worldometers.info/coronavirus/.2. Vetter P, Vu DL, L'Huillier AG, Schibler M, Kaiser L, Jacquerioz F. Clinical features of covid-19. BMJ. 2020; 369:m1470.
Article3. Chaddha U, Kaul V, Agrawal A. What is the true mortality in the critically ill patients with COVID-19? Indian J Crit Care Med. 2020; 24:383–4.
Article4. Olumade TJ, Uzairue LI. Clinical characteristics of 4499 COVID-19 patients in Africa: a meta-analysis. J Med Virol. 2021; 93:3055–61.
Article5. Abayomi A, Odukoya O, Osibogun A, Wright O, Adebayo B, Balogun M, et al. Presenting symptoms and predictors of poor outcomes among 2,184 patients with COVID-19 in Lagos State, Nigeria. Int J Infect Dis. 2021; 102:226–32.
Article6. El Vally A, Bollahi MA, Ould Ahmedou Salem MS, Deida J, Parola P, Basco L, et al. Retrospective overview of a COVID-19 outbreak in Mauritania. New Microbes New Infect. 2020; 38:100788.
Article7. Ibrahim OR, Suleiman BM, Abdullahi SB, Oloyede T, Sanda A, Gbadamosi MS, et al. Epidemiology of COVID-19 and predictors of outcome in Nigeria: a single-center study. Am J Trop Med Hyg. 2020; 103:2376–81.
Article8. Matangila JR, Nyembu RK, Telo GM, Ngoy CD, Sakobo TM, Massolo JM, et al. Clinical characteristics of COVID-19 patients hospitalized at Clinique Ngaliema, a public hospital in Kinshasa, in the Democratic Republic of Congo: a retrospective cohort study. PLoS One. 2020; 15:e0244272.
Article9. Bahloul M, Ketata W, Lahyeni D, Mayoufi H, Kotti A, Smaoui F, et al. Pulmonary capillary leak syndrome following COVID-19 virus infection. J Med Virol. 2021; 93:94–6.
Article10. Saida IB, Ennouri E, Nachi R, Meddeb K, Mahmoud J, Thabet N, et al. Very severe COVID-19 in the critically ill in Tunisia. Pan Afr Med J. 2020; 35(Suppl 2):136.
Article11. Hare SS, Rodrigues JCL, Nair A, Jacob J, Upile S, Johnstone A, et al. The continuing evolution of COVID-19 imaging pathways in the UK: a British Society of Thoracic Imaging expert reference group update. Clin Radiol. 2020; 75:399–404.
Article12. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993; 270:2957–63.
Article13. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001; 286:1754–8.
Article14. World Health Organization. Obesity [Internet]. Geneva: World Health Organization;2020. [cited 2020 Jul 24]. Available from: https://www.who.int/topics/obesity/en/.15. Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019; 9:69.
Article16. RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021; 384:693–704.
Article17. Makkar P, Pastores SM. Respiratory management of adult patients with acute respiratory distress syndrome due to COVID-19. Respirology. 2020; 25:1133–5.
Article18. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–43.
Article19. Lo Bianco G, Di Pietro S, Mazzuca E, et al. Multidisciplinary approach to the diagnosis and in-hospital management of COVID-19 infection: a narrative review. Front Pharmacol. 2020; 11:572168.
Article20. Agarwal N, Biswas B, Lohani P. Epidemiological determinants of COVID-19 infection and mortality: a study among patients presenting with severe acute respiratory illness during the pandemic in Bihar, India. Niger Postgrad Med J. 2020; 27:293–301.
Article21. Brown WA, Moore EM, Watters DA. Mortality of patients with COVID-19 who undergo an elective or emergency surgical procedure: a systematic review and meta-analysis. ANZ J Surg. 2021; 91:33–41.
Article22. Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020; 180:1345–55.23. Verma AA, Hora T, Jung HY, Fralick M, Malecki SL, Lapointe-Shaw L, et al. Characteristics and outcomes of hospital admissions for COVID-19 and influenza in the Toronto area. CMAJ. 2021; 193:E410–8.
Article24. Roedl K, Jarczak D, Thasler L, Bachmann M, Schulte F, Bein B, et al. Mechanical ventilation and mortality among 223 critically ill patients with coronavirus disease 2019: a multicentric study in Germany. Aust Crit Care. 2021; 34:167–75.
Article25. Name JJ, Souza AC, Vasconcelos AR, Prado PS, Pereira CP. Zinc, vitamin D and vitamin C: perspectives for COVID-19 with a focus on physical tissue barrier integrity. Front Nutr. 2020; 7:606398.
Article26. Kim MS, An MH, Kim WJ, Hwang TH. Comparative efficacy and safety of pharmacological interventions for the treatment of COVID-19: a systematic review and network meta-analysis. PLoS Med. 2020; 17:e1003501.
Article27. Zang X, Wang Q, Zhou H, Liu S, Xue X; COVID-19 Early Prone Position Study Group. Efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med. 2020; 46:1927–9.
Article28. Kang SH, Kim SW, Kim AY, Cho KH, Park JW, Do JY. Association between chronic kidney disease or acute kidney injury and clinical outcomes in COVID-19 patients. J Korean Med Sci. 2020; 35:e434.
Article29. Fabrizi F, Alfieri CM, Cerutti R, Lunghi G, Messa P. COVID-19 and acute kidney injury: a systematic review and meta-analysis. Pathogens. 2020; 9:1052.
Article30. Kolhe NV, Fluck RJ, Selby NM, Taal MW. Acute kidney injury associated with COVID-19: a retrospective cohort study. PLoS Med. 2020; 17:e1003406.
Article31. Nakajima K, Abe T, Saji R, Ogawa F, Taniguchi H, Yamaguchi K, et al. Serum cholinesterase associated with COVID-19 pneumonia severity and mortality. J Infect. 2021; 82:282–327.
Article32. Bahloul M, Baccouch N, Chtara K, Turki M, Turki O, Hamida CB, et al. Value of serum cholinesterase activity in the diagnosis of septic shock due to bacterial infections. J Intensive Care Med. 2017; 32:346–52.
Article33. Bardi T, Pintado V, Gomez-Rojo M, Escudero-Sanchez R, Azzam Lopez A, Diez-Remesal Y, et al. Nosocomial infections associated to COVID-19 in the intensive care unit: clinical characteristics and outcome. Eur J Clin Microbiol Infect Dis. 2021; 40:495–502.
Article34. Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS One. 2021; 16:e0251170.
Article35. Bassetti M, Kollef MH, Timsit JF. Bacterial and fungal superinfections in critically ill patients with COVID-19. Intensive Care Med. 2020; 46:2071–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of prone position on outcomes of COVID-19 patients with spontaneous breathing
- Gravity-induced ischemia in the brain and prone positioning for COVID-19 patients breathing spontaneously: still far from the truth!
- Characteristics of Critically Ill COVID-19 Patients in Busan, Republic of Korea
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea
- How We Have Treated Severe to Critically Ill Patients With Coronavirus Disease 2019 in Korea