J Korean Med Sci.
2022 Apr;37(13):e99. 10.3346/jkms.2022.37.e99.
Comparisons Between Normocalcemic Primary Hyperparathyroidism and Typical Primary Hyperparathyroidism
- Affiliations
-
- 1Department of Surgery, Eulji Medical Center, Eulji University School of Medicine, Seoul, Korea
- 2Department of Family medicine, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 3Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2527832
- DOI: http://doi.org/10.3346/jkms.2022.37.e99
Abstract
- Background
Normocalcemic primary hyperparathyroidism (NPHPT) was first described in 2008. It is defined as consistently elevated serum parathyroid hormone (PTH) levels with normal serum calcium (sCa) concentration, after excluding secondary causes of PTH elevation. However, the exact definition and management strategy for NPHPT remain controversial. We retrospectively investigated the clinicopathological features and short-term outcomes of NPHPT patients.
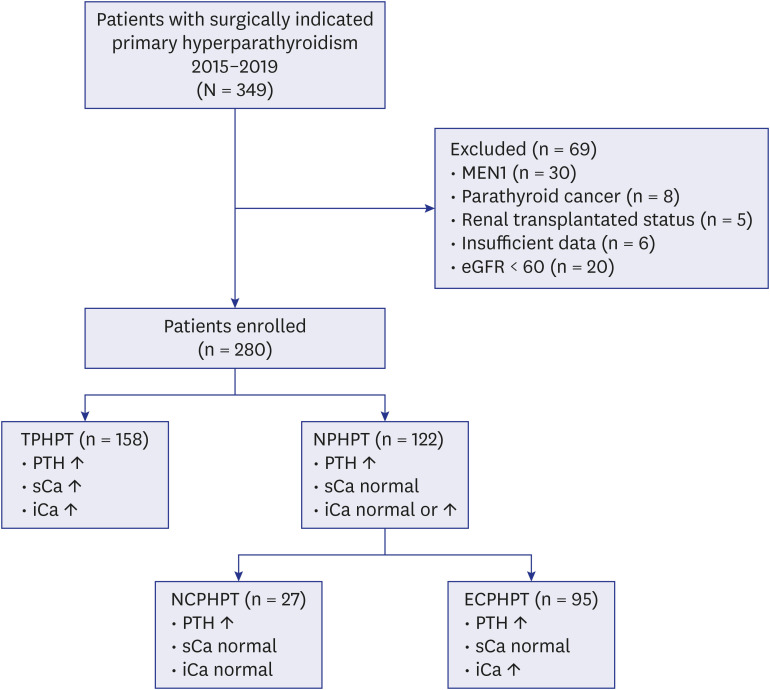
Methods
A total of 280 patients who were surgically indicated for primary hyperparathyroidism (PHPT) at the Yonsei Severance Medical Center between 2015 and 2019 were included. Patients were classified according to preoperative PTH, corrected sCa, and ionized calcium (iCa) levels as follows: typical primary hyperparathyroidism (TPHPT, elevated PTH, sCa, and iCa, n = 158) and NPHPT (elevated PTH, normal sCa, n = 122).
Results
NPHPT was commonly seen in younger individuals (aged < 50 years, P = 0.025); nephrolithiasis and bone fractures were common. Preoperative PTH level was higher in the TPHPT group (P < 0.001). The NPHPT group had higher numbers of multiple parathyroid lesions (P = 0.004) that were smaller (P = 0.011). NPHPT patients were further divided into two subgroups according to iCa levels: the elevated (n = 95) and normal iCa (n = 27) groups. There was no significant difference between the two subgroups regarding symptoms and multiplicity of lesions.
Conclusion
We found that NPHPT may be a heterogeneous disease entity of PHPT with high rates of multi-gland disease, which appears to be biochemically milder but symptomatic. Intraoperative PTH monitoring might help increase the surgery success rate. Moreover, the short-term outcomes of NPHPT after surgery did not differ from that of TPHPT.
Figure
Reference
-
1. Bilezikian JP, Khan AA, Potts JT Jr. Third International Workshop on the Management of Asymptomatic Primary Hyperthyroidism. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab. 2009; 94(2):335–339. PMID: 19193908.
Article2. Eastell R, Brandi ML, Costa AG, D’Amour P, Shoback DM, Thakker RV. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014; 99(10):3570–3579. PMID: 25162666.
Article3. Madeo B, Kara E, Cioni K, Vezzani S, Trenti T, Santi D, et al. Serum calcium to phosphorous (Ca/P) ratio is a simple, inexpensive, and accurate tool in the diagnosis of primary hyperparathyroidism. JBMR Plus. 2017; 2(2):109–117. PMID: 30283895.
Article4. Guo Y, Wang Q, Lu C, Fan P, Li J, Luo X, et al. New parathyroid function index for the differentiation of primary and secondary hyperparathyroidism: a case-control study. BMC Endocr Disord. 2020; 20(1):5. PMID: 31914999.
Article5. Lavryk OA, Siperstein AE. Use of calcium and parathyroid hormone nomogram to distinguish between atypical primary hyperparathyroidism and normal patients. World J Surg. 2017; 41(1):122–128. PMID: 27734082.
Article6. Palermo A, Jacques R, Gossiel F, Reid DM, Roux C, Felsenberg D, et al. Normocalcaemic hypoparathyroidism: prevalence and effect on bone status in older women. The OPUS study. Clin Endocrinol (Oxf). 2015; 82(6):816–823. PMID: 25640980.
Article7. García-Martín A, Reyes-García R, Muñoz-Torres M. Normocalcemic primary hyperparathyroidism: one-year follow-up in one hundred postmenopausal women. Endocrine. 2012; 42(3):764–766. PMID: 22573047.
Article8. Berger C, Almohareb O, Langsetmo L, Hanley DA, Kovacs CS, Josse RG, et al. Characteristics of hyperparathyroid states in the Canadian multicentre osteoporosis study (CaMos) and relationship to skeletal markers. Clin Endocrinol (Oxf). 2015; 82(3):359–368. PMID: 25059283.
Article9. Kontogeorgos G, Trimpou P, Laine CM, Oleröd G, Lindahl A, Landin-Wilhelmsen K. Normocalcaemic, vitamin D-sufficient hyperparathyroidism - high prevalence and low morbidity in the general population: A long-term follow-up study, the WHO MONICA project, Gothenburg, Sweden. Clin Endocrinol (Oxf). 2015; 83(2):277–284. PMID: 25988687.
Article10. Cusano NE, Maalouf NM, Wang PY, Zhang C, Cremers SC, Haney EM, et al. Normocalcemic hyperparathyroidism and hypoparathyroidism in two community-based nonreferral populations. J Clin Endocrinol Metab. 2013; 98(7):2734–2741. PMID: 23690312.
Article11. Tordjman KM, Greenman Y, Osher E, Shenkerman G, Stern N. Characterization of normocalcemic primary hyperparathyroidism. Am J Med. 2004; 117(11):861–863. PMID: 15589491.
Article12. Silverberg SJ, Bilezikian JP. “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J Clin Endocrinol Metab. 2003; 88(11):5348–5352. PMID: 14602772.
Article13. Šiprová H, Fryšák Z, Souček M. Primary hyperparathyroidism, with a focus on management of the normocalcemic form: to treat or not to treat? Endocr Pract. 2016; 22(3):294–301. PMID: 26523628.
Article14. Cusano NE, Cipriani C, Bilezikian JP. Management of normocalcemic primary hyperparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018; 32(6):837–845. PMID: 30665550.
Article15. Lowe H, McMahon DJ, Rubin MR, Bilezikian JP, Silverberg SJ. Normocalcemic primary hyperparathyroidism: further characterization of a new clinical phenotype. J Clin Endocrinol Metab. 2007; 92(8):3001–3005. PMID: 17536001.
Article16. Ledger GA, Burritt MF, Kao PC, O’Fallon WM, Riggs BL, Khosla S. Abnormalities of parathyroid hormone secretion in elderly women that are reversible by short term therapy with 1,25-dihydroxyvitamin D3. J Clin Endocrinol Metab. 1994; 79(1):211–216. PMID: 8027229.
Article17. Cosman F, Nieves J, Horton J, Shen V, Lindsay R. Effects of estrogen on response to edetic acid infusion in postmenopausal osteoporotic women. J Clin Endocrinol Metab. 1994; 78(4):939–943. PMID: 8157725.
Article18. Vincent A, Riggs BL, Atkinson EJ, Oberg AL, Khosla S. Effect of estrogen replacement therapy on parathyroid hormone secretion in elderly postmenopausal women. Menopause. 2003; 10(2):165–171. PMID: 12627043.
Article19. Invernizzi M, Carda S, Righini V, Baricich A, Cisari C, Bevilacqua M. Different PTH response to oral peptone load and oral calcium load in patients with normocalcemic primary hyperparathyroidism, primary hyperparathyroidism, and healthy subjects. Eur J Endocrinol. 2012; 167(4):491–497. PMID: 22872468.
Article20. Maruani G, Hertig A, Paillard M, Houillier P. Normocalcemic primary hyperparathyroidism: evidence for a generalized target-tissue resistance to parathyroid hormone. J Clin Endocrinol Metab. 2003; 88(10):4641–4648. PMID: 14557434.
Article21. Wang X, Meng L, Su C, Shapses SA. Low free (but not total) 25-hydroxyvitamin D levels in subjects with normocalcemic hyperparathyroidism. Endocr Pract. 2020; 26(2):174–178. PMID: 31557077.
Article22. Díaz-Soto G, Romero E, Castrillón JL, Jauregui OI, de Luis Román D. Clinical Expression of Calcium Sensing Receptor Polymorphism (A986S) in Normocalcemic and Asymptomatic Hyperparathyroidism. Clinical expression of calcium sensing receptor polymorphism (A986S) in normocalcemic and asymptomatic hyperparathyroidism. Horm Metab Res. 2016; 48(3):163–168. PMID: 26332755.
Article23. Callender GG, Udelsman R. Surgery for primary hyperparathyroidism. Cancer. 2014; 120(23):3602–3616. PMID: 25042934.
Article25. Trinh G, Rettig E, Noureldine SI, Russell JO, Agrawal N, Mathur A, et al. Surgical management of normocalcemic primary hyperparathyroidism and the impact of intraoperative parathyroid hormone testing on outcome. Otolaryngol Head Neck Surg. 2018; 159(4):630–637. PMID: 30105919.
Article26. Brown EM. Clinical lessons from the calcium-sensing receptor. Nat Clin Pract Endocrinol Metab. 2007; 3(2):122–133. PMID: 17237839.
Article27. McLeod MK, Monchik JM, Martin HF. The role of ionized calcium in the diagnosis of subtle hypercalcemia in symptomatic primary hyperparathyroidism. Surgery. 1984; 95(6):667–673. PMID: 6729704.28. Zavatta G, Clarke BL. Normocalcemic hyperparathyroidism: a heterogeneous disorder often misdiagnosed? JBMR Plus. 2020; 4(8):e10391. PMID: 32803112.
Article29. Koumakis E, Souberbielle JC, Sarfati E, Meunier M, Maury E, Gallimard E, et al. Bone mineral density evolution after successful parathyroidectomy in patients with normocalcemic primary hyperparathyroidism. J Clin Endocrinol Metab. 2013; 98(8):3213–3220. PMID: 23783096.
Article30. Palermo A, Naciu AM, Tabacco G, Falcone S, Santonati A, Maggi D, et al. Clinical, biochemical, and radiological profile of normocalcemic primary hyperparathyroidism. J Clin Endocrinol Metab. 2020; 105(7):dgaa174. PMID: 32271382.
Article31. Lim JY, Herman MC, Bubis L, Epelboym I, Allendorf JD, Chabot JA, et al. Differences in single gland and multigland disease are seen in low biochemical profile primary hyperparathyroidism. Surgery. 2017; 161(1):70–77. PMID: 27847113.
Article32. Wade TJ, Yen TW, Amin AL, Wang TS. Surgical management of normocalcemic primary hyperparathyroidism. World J Surg. 2012; 36(4):761–766. PMID: 22286968.
Article33. Kim JK, Chai YJ, Chung JK, Hwang KT, Heo SC, Kim SJ, et al. The prevalence of primary hyperparathyroidism in Korea: a population-based analysis from patient medical records. Ann Surg Treat Res. 2018; 94(5):235–239. PMID: 29732354.
Article34. Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, et al. American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 Update. Endocr Pract. 2020; 26(Suppl 1):1–46.
Article35. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96(7):1911–1930. PMID: 21646368.
Article36. Park HY, Lim YH, Park JB, Rhie J, Lee SJ. Environmental and occupation factors associated with vitamin D deficiency in Korean adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2010–2014. Int J Environ Res Public Health. 2020; 17(24):E9166. PMID: 33302471.
Article37. Schini M, Jacques RM, Oakes E, Peel NF, Walsh JS, Eastell R. Normocalcemic hyperparathyroidism: study of its prevalence and natural history. J Clin Endocrinol Metab. 2020; 105(4):e1171–e1186.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary hyperparathyroidism erosion of the sternal ends of the clavicles, a new sign of hyperparathyroidism: a case report
- Multiple brown tumors in a patient with primary hyperparathyroidism
- Primary Hyperparathyroidism Assosiated with Pathologic Fracture: A Case Report
- Primary Hyperparathyroidism with Typical Bone Changes: A Case Report
- Primary Hyperparathyroidism in a Child with Urolithiasis: 1 Case