J Cerebrovasc Endovasc Neurosurg.
2022 Mar;24(1):51-57. 10.7461/jcen.2022.E2021.06.003.
Endovascular occlusion of giant serpentine aneurysm: A case report and literature review
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Pamukkale University, Denizli, Turkey
- 2Department of Neurosurgery, Tohoku Medical and Pharmaceutical University, Sendai, Japan
- KMID: 2527595
- DOI: http://doi.org/10.7461/jcen.2022.E2021.06.003
Abstract
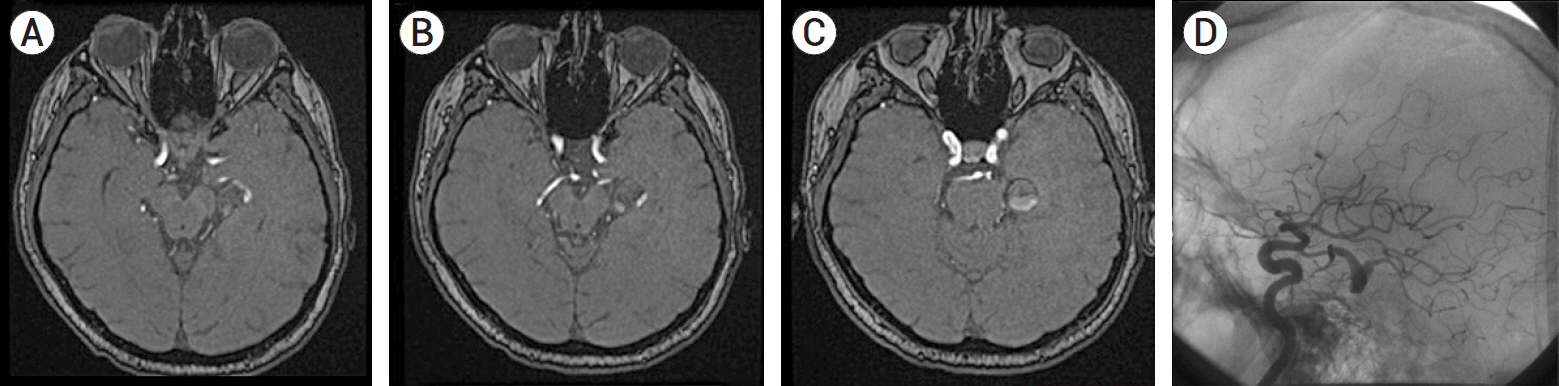
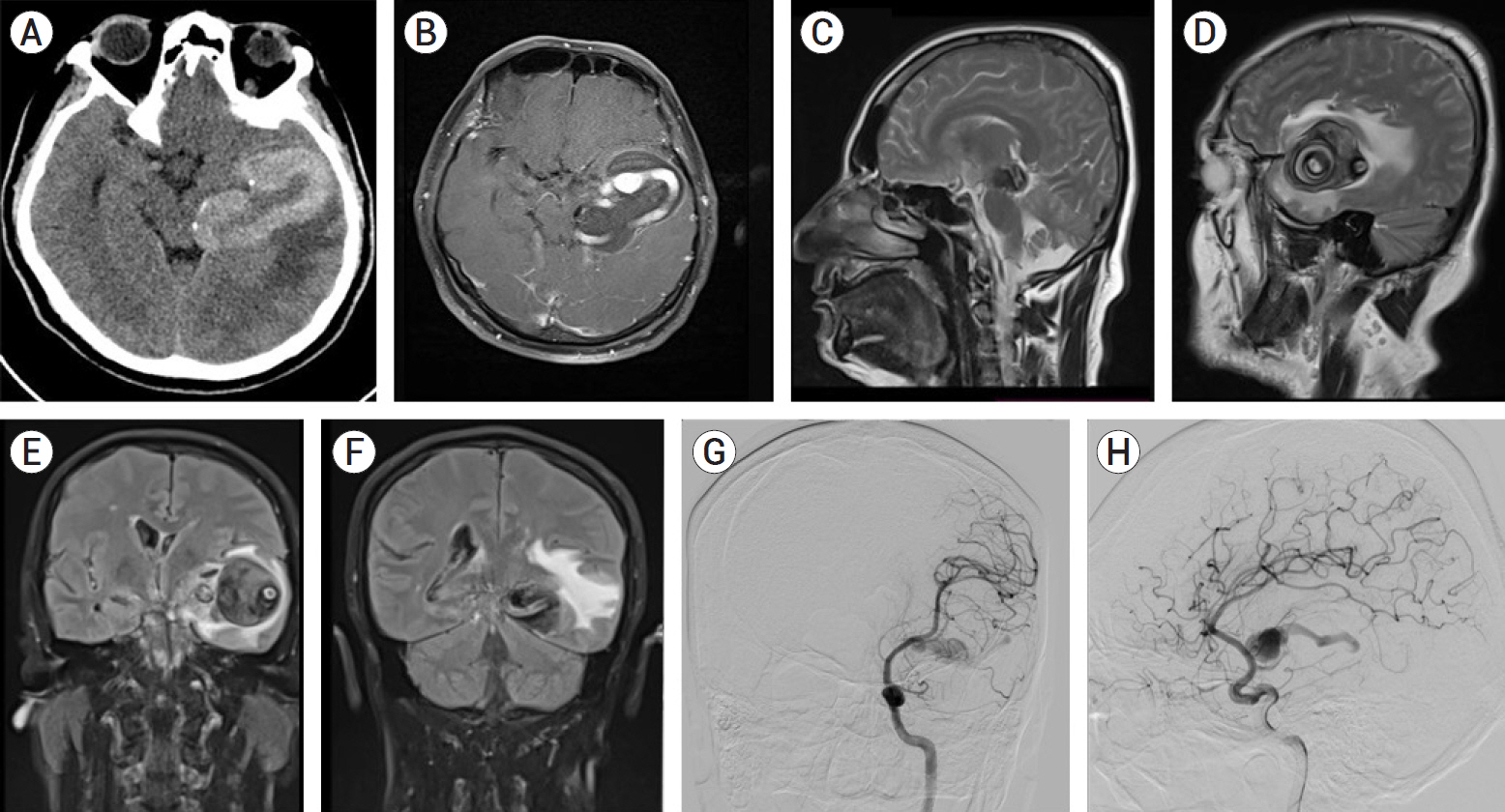
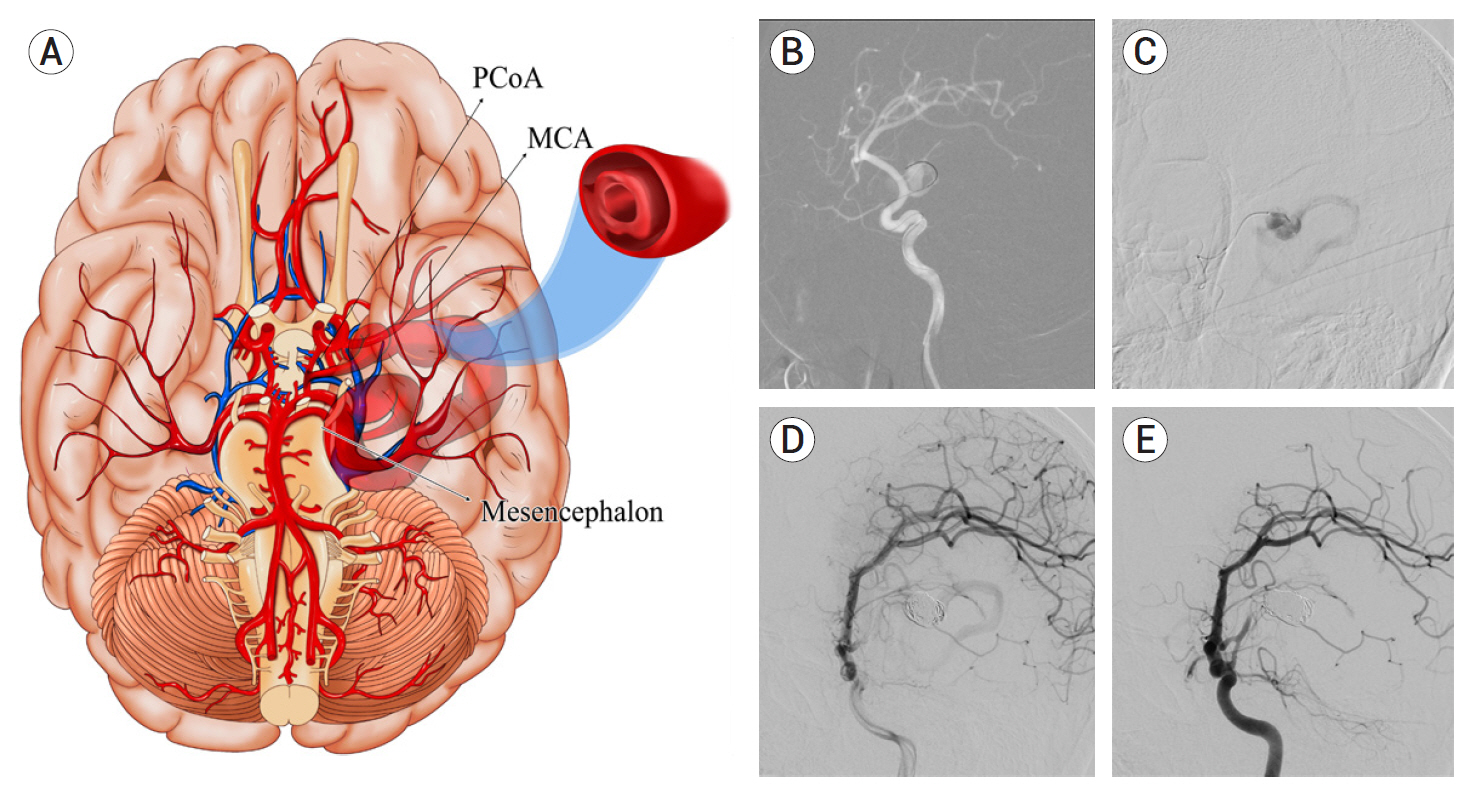
- Giant serpentine aneurysms (GSAs) are a rare subgroup of intracranial aneurysms. Separate inflow and outflow flow due to intraluminal thrombosis is the most distinguishing feature of GSAs. In treating these lesions, surgical clipping and ligation were the main treatments in the past, but bypass for revascularisation and endovascular therapies (EVTs) for deconstructive purposes are more prominent today. A 51-years-old male patient presented with headache and mild right hemiparesis. He had a GSA arising from the left fetal type posterior cerebral artery (fPCA) that was out of follow-up for six years. Radiological images revealed midline shifting and mesencephalon compression. We performed endovascular parent artery coil occlusion. The symptoms of the patient improved at the first-month follow-up. Even if there is a mass effect in GSAs, deconstructive EVT is a safe and feasible method for managing these lesions.
Figure
Reference
-
1. Aletich VA, Debrun GM, Monsein LH, Nauta HJ, Spetzler RF. Giant serpentine aneurysms: a review and presentation of five cases. AJNR Am J Neuroradiol. 1995; May. 16(5):1061–72.2. Anson JA, Lawton MT, Spetzler RF. Characteristics and surgical treatment of dolichoectatic and fusiform aneurysms. J Neurosurg. 1996; Feb. 84(2):185–93.
Article3. Benet A, Bang JS, Lawton MT. A3-A3 in situ bypass and distal clip occlusion of giant serpentine anterior communicating artery aneurysm: 3-dimensional operative video. Oper Neurosurg (Hagerstown). 2017; Dec. 13(6):755.
Article4. Christiano LD, Gupta G, Prestigiacomo CJ, Gandhi CD. Giant serpentine aneurysms. Neurosurg Focus. 2009; May. 26(5):E5.
Article5. Coley SC, Hodgson TJ, Jakubowski J. Coil embolization of giant serpentine aneurysms: report of two cases arising from the posterior cerebral artery. Br J Neurosurg. 2002; Feb. 16(1):43–7.
Article6. Dao W, Xiao Z, Kong Z, Jiang J, Lu Z. Clinical characteristics and endovascular treatment in patients with intracranial giant serpentine aneurysms. Quant Imaging Med Surg. 2021; Apr. 11(4):1490–5.
Article7. Deng Q, Feng WF. Giant serpentine aneurysm of the internal cerebral artery and mandibular aneurysm: a case report. Chin Neurosurg J. 2019; Nov. 5:26.
Article8. Gonzalez NR, Duckwiler G, Murayama Y, Viñuela F. Challenges in the endovascular treatment of giant intracranial aneurysms. Neurosurgery. 2008; Jun. 6 Suppl 3:1324–35.
Article9. Kandemirli SG, Cekirge S, Oran I, Saatci I, Kizilkilic O, Cinar C, et al. Intracranial serpentine aneurysms: spontaneous changes of angiographic filling pattern. AJNR Am J Neuroradiol. 2018; Sep. 39(9):1662–8.
Article10. Lan J, Fu ZY, Zhang JJ, Ma C, Cao CJ, Zhao WY, et al. Giant serpentine aneurysm of the middle cerebral artery. World Neurosurg. 2018; Sep. 117:109–14.
Article11. Li M, Ma Y, Jiang P, Wu J, Cao Y, Wang S. Microsurgical outcome of unruptured giant intracranial aneurysms: a single-center experience. Journal of Clinical Neuroscience. 2019; Dec. 70:132–5.
Article12. Mizuno H, Wakabayashi K, Shimizu T, Tomita Y, Koga H, Yoshimoto Y. Deconstructive endovascular treatment of ruptured serpentine basilar artery aneurysm by mid-basilar occlusion. World Neurosurg. 2021; Feb. 146:40–4.
Article13. Mura J, Alvarez VH, Oberman DZ, Cardenas AR, Rabelo NN, Figueiredo EG. Management of giant thrombosed MCA aneurysm: double STA-MCA revascularization. World Neurosurg. 2021; May. 149:1.
Article14. Otsuka G, Miyachi S, Handa T, Negoro M, Okamoto T, Suzuki O, et al. Endovascular trapping of giant serpentine aneurysms by using Guglielmi detachable coils: successful reduction of mass effect. Report of two cases. J Neurosurg. 2001; May. 94(5):836–40.15. Pavesi G, Dimitriadis S, Baroni S, Vallone S, Valzania F, Costella GB, et al. Intraoperative functional and perfusion monitoring during surgery for giant serpentine middle cerebral artery aneurysms. World Neurosurg. 2015; Aug. 84(2):592.
Article16. Segal HD, McLaurin RL. Giant serpentine aneurysm. Report of two cases. J Neurosurg. 1977; Jan. 46(1):115–20.17. Suzuki S, Takahashi T, Ohkuma H, Shimizu T, Fujita S. Management of giant serpentine aneurysms of the middle cerebral artery—review of literature and report of a case successfully treated by STA-MCA anastomosis only. Acta Neurochir (Wien). 1992; 117(1-2):23–9.18. Tao T, Dai W, Li W, Hang CH. Giant serpentine distal anterior cerebral artery aneurysm treated with ın situ side-to-side A3-A3 anastomosis and aneurysm resection. World Neurosurg. 2020; Jan. 133:21–4.19. Yoshimura S, Nishimura Y, Andoh T, Sakai N, Yamada H. Giant serpentine aneurysm followed up for more than 10 years: report of a case and review of the literature. No Shinkei Geka. 1994; Feb. 22(2):179–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Giant Serpentine Aneurysm of the Middle Cerebral Artery
- Giant Serpentine Intracranial Aneurysm Treated with Wrapping under the Extracorporeal Circulation and Hypothermia
- Giant Serpentine Aneurysm of the Middle Cerebral Artery
- Giant Serpentine Intracranial Aneurysm: A Case Report
- Giant Serpentine Aneurysm of the Anterior Communicating Artery: Case Report