J Cerebrovasc Endovasc Neurosurg.
2022 Mar;24(1):10-15. 10.7461/jcen.2021.E2021.06.012.
Angiographic characteristics of ruptured versus unruptured vertebral artery dissecting aneurysm
- Affiliations
-
- 1Department of Neurosurgery, Daegu Catholic University Hospital, Daegu, Korea
- KMID: 2527590
- DOI: http://doi.org/10.7461/jcen.2021.E2021.06.012
Abstract
Objective
Vertebral artery dissecting aneurysm (VADA) is a rare and critical disease. VADA rupture can cause subarachnoid hemorrhage which is a major complication of VADA due to their high rebleeding rate and poor outcome. In the present study, ruptured and unruptured VADAs were compared by analyzing angiographic findings to determine useful predisposing factors for VADA rupture for appropriate treatment selection.
Methods
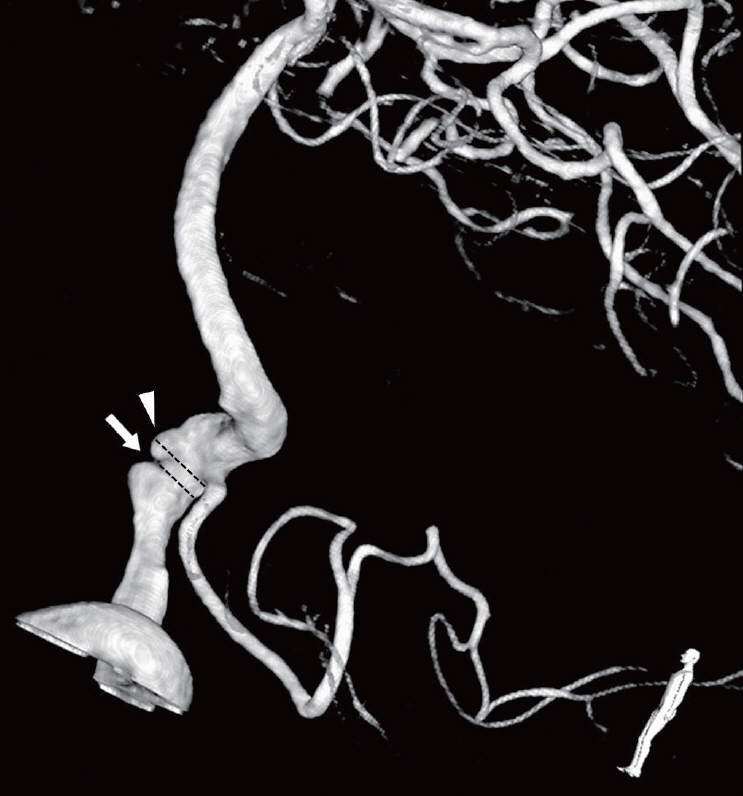
Subjects with VADA treated during a 10-year period were retrospectively identified. The 57 cases diagnosed with VADA were divided into ruptured (n=15) and unruptured (n=42) groups. In addition, each case was analyzed using angiographic 3-dimensional (3-D) reconstructed images. Factors such as length, dilated and stenotic diameter, shape, and vessel around the vertebral artery (VA) were measured and statistically compared.
Results
In the ruptured group, stenotic findings of the affected lesion were more common and severe than in the unruptured group. The average stenotic diameter was 2.27 mm (vs. 2.84 mm). And stenotic degree was 62% and 53% in the ruptured and unruptured groups, respectively. Posterior communicating artery (PcomA) flow was more common in the ruptured group (87% vs. 55%, p=0.028).
Conclusions
Based on angiographic findings, stenotic lesions, which may be influenced by PcomA flow, are more common in ruptured VADAs.
Figure
Reference
-
1. Beck J, Rohde S, el Beltagy M, Zimmermann M, Berkefeld J, Seifert V, et al. Difference in configuration of ruptured and unruptured intracranial aneurysms determined by biplanar digital subtraction angiography. Acta Neurochir (Wien). 2003; Oct. 145(10):861–5. discussion 865.
Article2. Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015; Jun. 14(6):640–54.
Article3. Gottesman RF, Sharma P, Robinson KA, Arnan M, Tsui M, Saber-Tehrani A, et al. Imaging characteristics of symptomatic vertebral artery dissection: a systematic review. Neurologist. 2012; Sep. 18(5):255–60.4. Guan J, Li G, Kong X, He C, Long J, Qin H, et al. Endovascular treatment for ruptured and unruptured vertebral artery dissecting aneurysms: a meta-analysis. J Neurointerv Surg. 2017; Jun. 9(6):558–63.
Article5. Iida H, Naito T, Hondo H, Demachi H, Aoki S. Intracranial aneurysms in autosomal dominant polycystic kidney disease detected by MR angiography: screening and treatment. Nihon Jinzo Gakkai Shi. 1998; Feb. 40(2):42–7.6. Ishibashi T, Murayama Y, Urashima M, Saguchi T, Ebara M, Arakawa H, et al. Unruptured intracranial aneurysms: incidence of rupture and risk factors. Stroke. 2009; Jan. 40(1):313–6.7. Jin SC, Kwon DH, Choi CG, Ahn JS, Kwun BD. Endovascular strategies for vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2009; Sep. 30(8):1518–23.
Article8. Kashiwazaki D, Ushikoshi S, Asano T, Kuroda S, Houkin K. Long-term clinical and radiological results of endovascular internal trapping in vertebral artery dissection. Neuroradiology. 2013; Feb. 55(2):201–6.
Article9. Kim BM, Shin YS, Kim SH, Suh SH, Ihn YK, Kim DI, et al. Incidence and risk factors of recurrence after endovascular treatment of intracranial vertebrobasilar dissecting aneurysms. Stroke. 2011; Sep. 42(9):2425–30.
Article10. Kim CH, Son YJ, Paek SH, Han MH, Kim JE, Chung YS, et al. Clinical analysis of vertebrobasilar dissection. Acta Neurochir (Wien). 2006; Apr. 148(4):395–404.
Article11. Kitanaka C, Tanaka J, Kuwahara M, Teraoka A, Sasaki T, Takakura K, et al. Nonsurgical treatment of unruptured intracranial vertebral artery dissection with serial follow-up angiography. J Neurosurg. 1994; Apr. 80(4):667–74.
Article12. Lv X, Jiang C, Li Y, Wu Z. Clinical outcomes of ruptured and unruptured vertebral artery-posterior inferior cerebellar artery complex dissecting aneurysms after endovascular embolization. AJNR Am J Neuroradiol. 2010; Aug. 31(7):1232–5.
Article13. Mazur MD, Kilburg C, Wang V, Taussky P. Pipeline embolization device for the treatment of vertebral artery aneurysms: the fate of covered branch vessels. J Neurointerv Surg. 2016; Oct. 8(10):1041–7.
Article14. Nam KH, Ko JK, Cha SH, Choi CH, Lee TH, Lee JI. Endovascular treatment of acute intracranial vertebral artery dissection: long-term follow-up results of internal trapping and reconstructive treatment using coils and stents. J Neurointerv Surg. 2015; Nov. 7(11):829–34.
Article15. Nam SW, Choi S, Cheong Y, Kim YH, Park HK. Evaluation of aneurysm-associated wall shear stress related to morphological variations of circle of Willis using a microfluidic device. J Biomech. 2015; Jan. 48(2):348–53.
Article16. Park KW, Park JS, Hwang SC, Im SB, Shin WH, Kim BT. Vertebral artery dissection: natural history, clinical features and therapeutic considerations. J Korean Neurosurg Soc. 2008; Sep. 44(3):109–15.
Article17. Ro A, Kageyama N. Pathomorphometry of ruptured intracranial vertebral arterial dissection: adventitial rupture, dilated lesion, intimal tear, and medial defect. J Neurosurg. 2013; Jul. 119(1):221–7.
Article18. Saatci I, Yavuz K, Ozer C, Geyik S, Cekirge HS. Treatment of intracranial aneurysms using the pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol. 2012; Sep. 33(8):1436–46.
Article19. Shimoji T, Bando K, Nakajima K, Ito K. Dissecting aneurysm of the vertebral artery. Report of seven cases and angiographic findings. J Neurosurg. 1984; Dec. 61(6):1038–46.20. Shin JH, Suh DC, Choi CG, Leei HK. Vertebral artery dissection: spectrum of imaging findings with emphasis on angiography and correlation with clinical presentation. Radiographics. 2000; Nov-Dec. 20(6):1687–96.
Article21. Takagi T, Takayasu M, Suzuki Y, Yoshida J. Prediction of rebleeding from angiographic features in vertebral artery dissecting aneurysms. Neurosurg Rev. 2007; Jan. 30(1):32–8. discussion 38.
Article22. Yamaura A, Watanabe Y, Saeki N. Dissecting aneurysms of the intracranial vertebral artery. J Neurosurg. 1990; Feb. 72(2):183–8.
Article23. Zhou W, Lu M, Li J, Chen F, Hu Q, Yang S. Functional posterior communicating artery of patients with posterior circulation ischemia using phase contrast magnetic resonance angiography. Exp Ther Med. 2019; Jan. 17(1):337–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antegrade Recanalization of Parent Artery after Internal Trapping of Ruptured Vertebral Artery Dissecting Aneurysm
- Endovascular Coil Trapping of a Ruptured Dissecting Aneurysm of the Vertebral Artery Using Detachable Coils and Micro-Tornado(R) Coils
- Dissecting Aneurysm of the Intracranial Vertbral Artery: Case Report
- Treatment of Ruptured Dissecting Aneurysm Associated with Fenestration of Vertebral Artery: A Case Report
- Angiographic Characteristics of the Intracranial Saccular Aneurysms to Predict the Rupture