Clin Endosc.
2022 Mar;55(2):297-301. 10.5946/ce.2020.301.
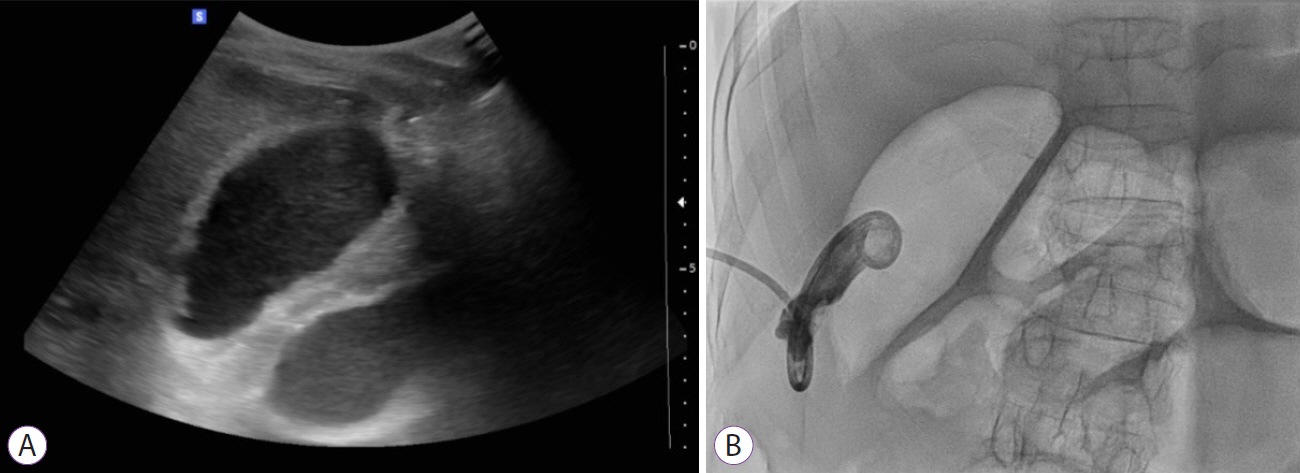
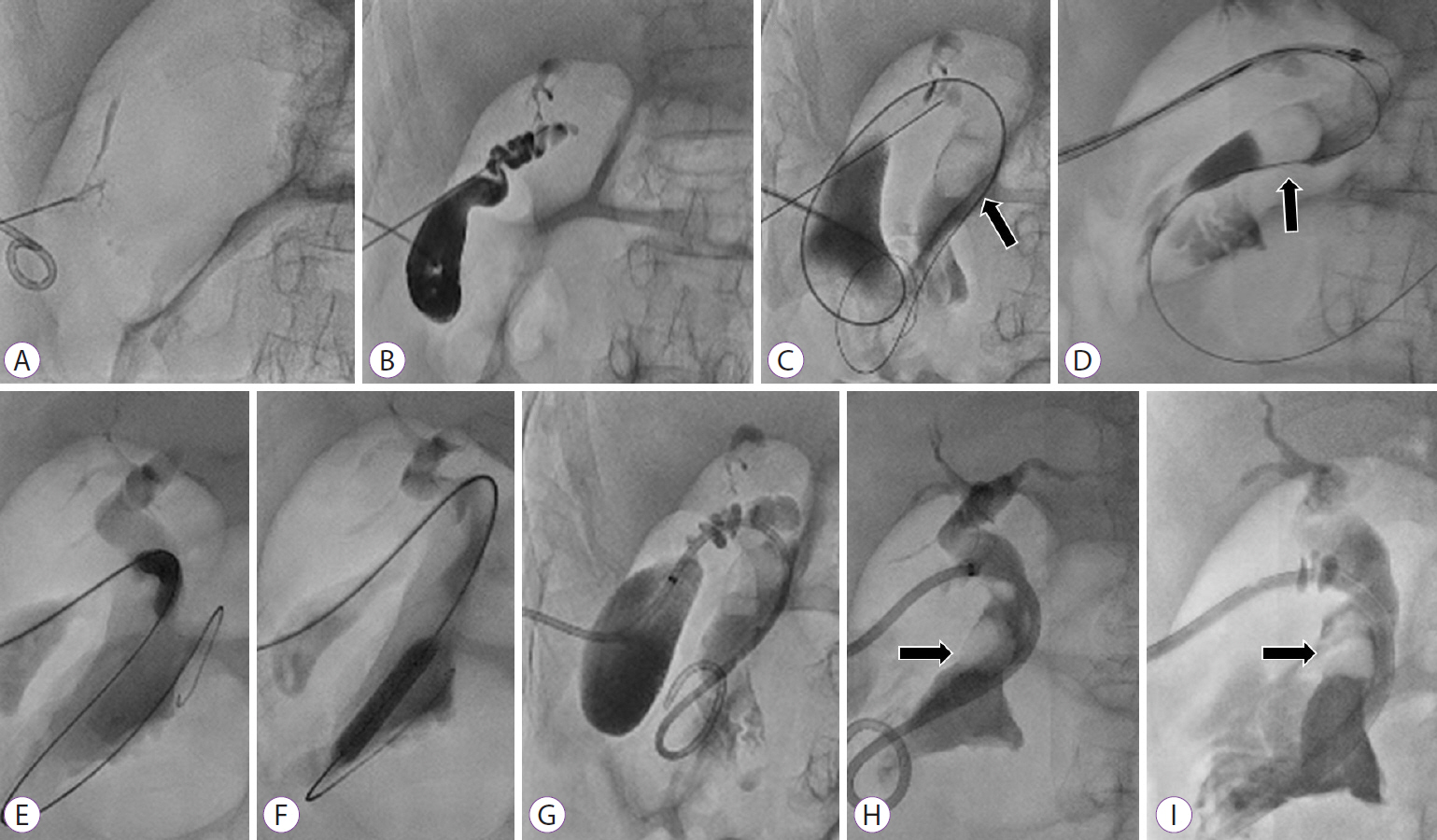
Successful Removal of a Difficult Common Bile Duct Stone by Percutaneous Transcholecystic Cholangioscopy
- Affiliations
-
- 1Department of Internal Medicine, Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2527576
- DOI: http://doi.org/10.5946/ce.2020.301
Abstract
- Common bile duct (CBD) stones are prevalent in 11% to 21% of patients with gallstones and can cause various clinical manifestations, from biliary colic to biliary sepsis. The treatment of choice is endoscopic retrograde cholangiopancreatography, but approximately 5% to 10% of CBD stones are difficult to remove using these conventional endoscopic methods. Although percutaneous transhepatic cholangioscopy and lithotripsy can be used as an alternative, it can be technically demanding and risky if the intrahepatic duct is not dilated. We report a case of a large CBD stone that was successfully removed using percutaneous transcholecystic cholangioscopy.
Keyword
Figure
Reference
-
1. Hermann RE. The spectrum of biliary stone disease. Am J Surg. 1989; 158:171–173.2. Möller M, Gustafsson U, Rasmussen F, Persson G, Thorell A. Natural course vs interventions to clear common bile duct stones: data from the Swedish Registry for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks). JAMA Surg. 2014; 149:1008–1013.3. Williams E, Beckingham I, El Sayed G, et al. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017; 66:765–782.4. Lee JH, Kim HW, Kang DH, et al. Usefulness of percutaneous transhepatic cholangioscopic lithotomy for removal of difficult common bile duct stones. Clin Endosc. 2013; 46:65–70.5. Jung GS, Kim YJ, Yun JH, et al. Percutaneous transcholecystic removal of common bile duct stones: case series in 114 patients. Radiology. 2019; 290:238–243.6. Ahmed S, Schlachter TR, Hong K. Percutaneous transhepatic cholangioscopy. Tech Vasc Interv Radiol. 2015; 18:201–209.7. Molvar C, Glaenzer B. Choledocholithiasis: evaluation, treatment, and outcomes. Semin Intervent Radiol. 2016; 33:268–276.8. Turner MA, Fulcher AS. The cystic duct: normal anatomy and disease processes. Radiographics. 2001; 21:3–22. questionnaire 288-294.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous transhepatic removal of common bile duct stone: a case report
- Two Cases of Percutaneous Transhepatic Choledochoscopy Treatment of Intrahepatic Duct Stones that Occurred after Living Donor Liver Transplantation
- Successful Endoscopic Treatment of Difficult Common Bile Duct Stones Using Various Interventional Techniques: A Case Report
- Usefulness of Percutaneous Transhepatic Cholangioscopy for Treatment of Intrahepatic Duct and Common Bile Stones and Diagnosis of Intrahepatic Duct Lesions with Biopsy
- Removal of a Large, Intractable Common Bile Duct Stone by Direct Peroral Cholangioscopy Using Upper Gastrointestinal Endoscopy and Polypectomy Snare