Clin Endosc.
2022 Mar;55(2):167-182. 10.5946/ce.2021.282.
2021 Korean Society of Gastrointestinal Endoscopy Clinical Practice Guidelines for Endoscopic Sedation
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Department of Internal Medicine, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Internal Medicine, Dongguk University Ilsan Hospital, Goyang, Korea
- 4Department of Internal Medicine, Ewha Womans University Seoul Hospital, Seoul, Korea
- 5Department of Internal Medicine, Kangwon National University School of Medicine, Kangwon National University Hospital, Chuncheon, Korea
- 6Department of Internal Medicine, Seoul Medical Center, Seoul, Korea
- 7Department of Internal Medicine, Jeonbuk National University Hospital, Jeonju, Korea
- 8Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea
- 9Department of Pediatrics, Seoul Metropolitan Children’s Hospital, Seoul, Korea
- 10Department of Internal Medicine, Wonkwang University College of Medicine and Hospital, Iksan, Korea
- 11Department of Internal Medicine, Gachon University, Gil Medical Center, Incheon, Korea
- 12Department of Internal Medicine, Uijungbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 13Yonsei Wonju Medical Library, Yonsei University Wonju College of Medicine, Wonju, Korea
- 14Division of Healthcare Technology Assessment Research, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
- 15Department of Urology, Yonsei University Wonju College of Medicine/Center of Evidence Based Medicine Institute of Convergence Science, Wonju, Korea
- 16Division of Gastroenterology, Department of Internal Medicine, Cha University Gangnam Medical Center, Seoul, Korea
- KMID: 2527558
- DOI: http://doi.org/10.5946/ce.2021.282
Abstract
- Sedation can resolve anxiety and fear in patients undergoing endoscopy. The use of sedatives has increased in Korea. Appropriate sedation is a state in which the patient feels subjectively comfortable while maintaining the airway reflex for stable spontaneous breathing. The patient should maintain a state of consciousness to the extent that he or she can cooperate with the needs of the medical staff. Despite its benefits, endoscopic sedation has been associated with cardiopulmonary complications. Cardiopulmonary complications are usually temporary. Most patients recover without sequelae. However, they may progress to serious complications, such as cardiovascular collapse. Therefore, it is essential to screen high-risk patients before sedation and reduce complications by meticulous monitoring. Additionally, physicians should be familiar with the management of emergencies. The first Korean clinical practice guideline for endoscopic sedation was developed based on previous worldwide guidelines for endoscopic sedation using an adaptation process. The guideline consists of nine recommendations based on a critical review of currently available data and expert consensus when the guideline was drafted. These guidelines should provide clinicians, nurses, medical school students, and policy makers with information on how to perform endoscopic sedation with minimal risk.
Figure
Reference
-
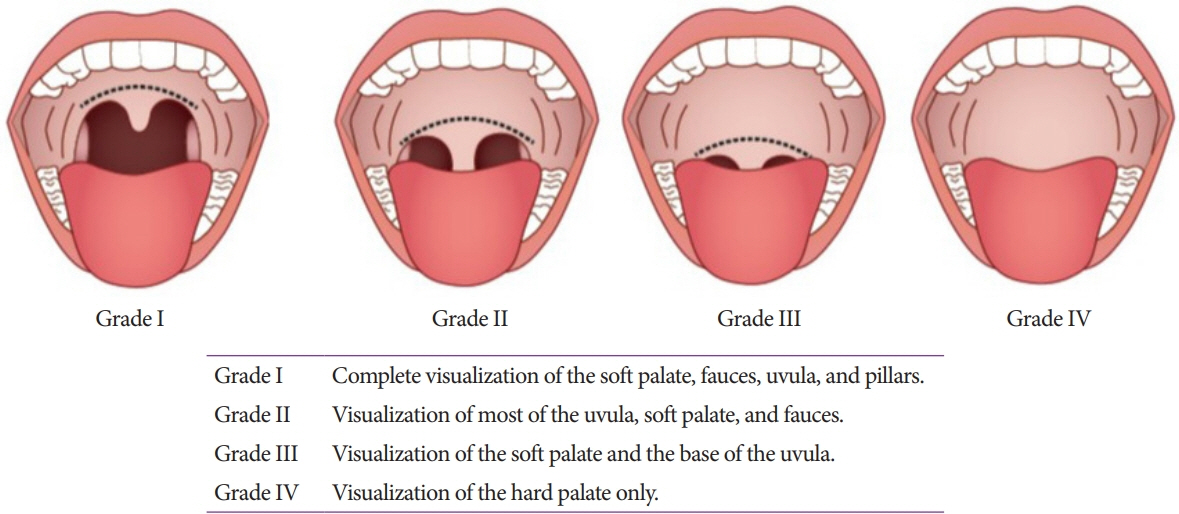
1. Dumonceau JM, Riphaus A, Beilenhoff U, et al. European curriculum for sedation training in gastrointestinal endoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA). Endoscopy. 2013; 45:496–504.2. Gotoda T, Akamatsu T, Abe S, et al. Guidelines for sedation in gastroenterological endoscopy (second edition). Dig Endosc. 2021; 33:21–53.3. American Association for the Study of Liver Diseases; American College of Gastroenterology; American Gastroenterological Association Institute, et al. Multisociety sedation curriculum for gastrointestinal endoscopy. Gastrointest Endosc. 2012; 76:e1–e25.4. Schilling D, Leicht K, Beilenhoff U, et al. Impact of S3 training courses “Sedation and emergency management in endoscopy for endoscopy nurses and assisting personnel” on the process and structure quality in gastroenterological endoscopy in practices and clinics - results of a nationwide survey. Z Gastroenterol. 2013; 51:619–627.5. Berzin TM, Sanaka S, Barnett SR, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011; 73:710–717.6. Qadeer MA, Lopez AR, Dumot JA, Vargo JJ. Hypoxemia during moderate sedation for gastrointestinal endoscopy: causes and associations. Digestion. 2011; 84:37–45.7. Frieling T, Heise J, Kreysel C, Kuhlen R, Schepke M. Sedation-associated complications in endoscopy--prospective multicentre survey of 191142 patients. Z Gastroenterol. 2013; 51:568–572.8. Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011; 74:1238–1247.9. Mador MJ, Nadler J, Mreyoud A, et al. Do patients at risk of sleep apnea have an increased risk of cardio-respiratory complications during endoscopy procedures? Sleep Breath. 2012; 16:609–615.10. Dumonceau JM, Riphaus A, Schreiber F, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates guideline--updated June 2015. Endoscopy. 2015; 47:1175–1189.11. ASGE Standards of Practice Committee, Early DS, Lightdale JR, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018; 87:327–337.12. Friedrich K, Stremmel W, Sieg A. Endoscopist-administered propofol sedation is safe - a prospective evaluation of 10,000 patients in an outpatient practice. J Gastrointestin Liver Dis. 2012; 21:259–263.13. Kim SY, Moon CM, Kim MH, et al. Impacts of age and sedation on cardiocerebrovascular adverse events after diagnostic GI endoscopy: a nationwide population-based study. Gastrointest Endosc. 2020; 92:591–602.e16.14. Mehta PP, Kochhar G, Kalra S, et al. Can a validated sleep apnea scoring system predict cardiopulmonary events using propofol sedation for routine EGD or colonoscopy? A prospective cohort study. Gastrointest Endosc. 2014; 79:436–444.15. Cha JM, Jeun JW, Pack KM, et al. Risk of sedation for diagnostic esophagogastroduodenoscopy in obstructive sleep apnea patients. World J Gastroenterol. 2013; 19:4745–4751.16. Hinkelbein J, Lamperti M, Akeson J, et al. European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur J Anaesthesiol. 2018; 35:6–24.17. Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985; 32:429–434.18. Dietrich CG, Kottmann T, Diedrich A, Drouven FM. Sedation-associated complications in endoscopy are not reduced significantly by implementation of the German S-3-guideline and occur in a severe manner only in patients with ASA class III and higher. Scand J Gastroenterol. 2013; 48:1082–1087.19. Enestvedt BK, Eisen GM, Holub J, Lieberman DA. Is the American Society of Anesthesiologists classification useful in risk stratification for endoscopic procedures? Gastrointest Endosc. 2013; 77:464–471.20. Muravchick S. The elderly outpatient: current anesthetic implications. Curr Opin Anaesthesiol. 2002; 15:621–625.21. Boss GR, Seegmiller JE. Age-related physiological changes and their clinical significance. West J Med. 1981; 135:434–440.22. Shaker R, Ren J, Bardan E, et al. Pharyngoglottal closure reflex: characterization in healthy young, elderly and dysphagic patients with predeglutitive aspiration. Gerontology. 2003; 49:12–20.23. Lukens FJ, Loeb DS, Machicao VI, Achem SR, Picco MF. Colonoscopy in octogenarians: a prospective outpatient study. Am J Gastroenterol. 2002; 97:1722–1725.24. ASGE Standards of Practice Committee, Chandrasekhara V, Early DS, et al. Modifications in endoscopic practice for the elderly. Gastrointest Endosc. 2013; 78:1–7.25. Darling E. Practical considerations in sedating the elderly. Crit Care Nurs Clin North Am. 1997; 9:371–380.26. Peacock JE, Lewis RP, Reilly CS, Nimmo WS. Effect of different rates of infusion of propofol for induction of anaesthesia in elderly patients. Br J Anaesth. 1990; 65:346–352.27. Horiuchi A, Nakayama Y, Tanaka N, Ichise Y, Katsuyama Y, Ohmori S. Propofol sedation for endoscopic procedures in patients 90 years of age and older. Digestion. 2008; 78:20–23.28. Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C. Conscious sedation with propofol in elderly patients: a prospective evaluation. Aliment Pharmacol Ther. 2003; 17:1493–1501.29. Bell GD, Spickett GP, Reeve PA, Morden A, Logan RF. Intravenous midazolam for upper gastrointestinal endoscopy: a study of 800 consecutive cases relating dose to age and sex of patient. Br J Clin Pharmacol. 1987; 23:241–243.30. Cha JM, Kozarek RA, La Selva D, et al. Risks and benefits of colonoscopy in patients 90 years or older, compared with younger patients. Clin Gastroenterol Hepatol. 2016; 14:80–86.e1.31. Kazama T, Takeuchi K, Ikeda K, et al. Optimal propofol plasma concentration during upper gastrointestinal endoscopy in young, middle-aged, and elderly patients. Anesthesiology. 2000; 93:662–669.32. Martínez JF, Aparicio JR, Compañy L, et al. Safety of continuous propofol sedation for endoscopic procedures in elderly patients. Rev Esp Enferm Dig. 2011; 103:76–82.33. Hayee B, Dunn J, Loganayagam A, et al. Midazolam with meperidine or fentanyl for colonoscopy: results of a randomized trial. Gastrointest Endosc. 2009; 69:681–687.34. Cohen LB, Hightower CD, Wood DA, Miller KM, Aisenberg J. Moderate level sedation during endoscopy: a prospective study using low-dose propofol, meperidine/fentanyl, and midazolam. Gastrointest Endosc. 2004; 59:795–803.35. Korean Medical Association. 2016 clinical recommendations for propofol-based sedation for physicians in Korean healthcare clinics and hospitals (in Korean). 2016 [Internet]. Seoul: KMA;c2016 [cited 2022 Jan 24]. Available from: https://www.nsdoctor.co.kr/file_download.php?idx=2384.36. Cohen LB, Dubovsky AN, Aisenberg J, Miller KM. Propofol for endoscopic sedation: a protocol for safe and effective administration by the gastroenterologist. Gastrointest Endosc. 2003; 58:725–732.37. Fatima H, DeWitt J, LeBlanc J, Sherman S, McGreevy K, Imperiale TF. Nurse-administered propofol sedation for upper endoscopic ultrasonography. Am J Gastroenterol. 2008; 103:1649–1656.38. Heuss LT, Froehlich F, Beglinger C. Nonanesthesiologist-administered propofol sedation: from the exception to standard practice. Sedation and monitoring trends over 20 years. Endoscopy. 2012; 44:504–511.39. Jensen JT, Vilmann P, Horsted T, et al. Nurse-administered propofol sedation for endoscopy: a risk analysis during an implementation phase. Endoscopy. 2011; 43:716–722.40. Daza JF, Tan CM, Fielding RJ, Brown A, Farrokhyar F, Yang I. Propofol administration by endoscopists versus anesthesiologists in gastrointestinal endoscopy: a systematic review and meta-analysis of patient safety outcomes. Can J Surg. 2018; 61:226–236.41. Külling D, Orlandi M, Inauen W. Propofol sedation during endoscopic procedures: how much staff and monitoring are necessary? Gastrointest Endosc. 2007; 66:443–449.42. Vargo JJ, Niklewski PJ, Williams JL, Martin JF, Faigel DO. Patient safety during sedation by anesthesia professionals during routine upper endoscopy and colonoscopy: an analysis of 1.38 million procedures. Gastrointest Endosc. 2017; 85:101–108.43. Khiani VS, Soulos P, Gancayco J, Gross CP. Anesthesiologist involvement in screening colonoscopy: temporal trends and cost implications in the medicare population. Clin Gastroenterol Hepatol. 2012; 10:58–64.e1.44. Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med. 2013; 173:551–556.45. Wernli KJ, Brenner AT, Rutter CM, Inadomi JM. Risks associated with anesthesia services during colonoscopy. Gastroenterology. 2016; 150:888–894. quiz e18.46. Practice guidelines for moderate procedural sedation and analgesia 2018: a report by the American Society of Anesthesiologists Task Force on moderate procedural sedation and analgesia, the American Association of Oral and Maxillofacial surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology. 2018; 128:437–479.47. Dumonceau JM, Riphaus A, Aparicio JR, et al. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology guideline: non-anesthesiologist administration of propofol for gi endoscopy. Endoscopy. 2010; 42:960–974.48. Riphaus A, Macias-Gomez C, Devière J, Dumonceau JM. Propofol, the preferred sedation for screening colonoscopy, is underused. Results of an international survey. Dig Liver Dis. 2012; 44:389–392.49. Lee CK, Dong SH, Kim ES, et al. Room for quality improvement in endoscopist-directed sedation: results from the first nationwide survey in Korea. Gut Liver. 2016; 10:83–94.50. Bell GD, Bown S, Morden A, Coady T, Logan RF. Prevention of hypoxaemia during upper-gastrointestinal endoscopy by means of oxygen via nasal cannulae. Lancet. 1987; 1:1022–1024.51. Bell GD, Quine A, Antrobus JH, et al. Upper gastrointestinal endoscopy: a prospective randomized study comparing continuous supplemental oxygen via the nasal or oral route. Gastrointest Endosc. 1992; 38:319–325.52. Bowling TE, Hadjiminas CL, Polson RJ, Baron JH, Foale RA. Effects of supplemental oxygen on cardiac rhythm during upper gastrointestinal endoscopy: a randomised controlled double blind trial. Gut. 1993; 34:1492–1497.53. Crantock L, Cowen AE, Ward M, Roberts RK. Supplemental low flow oxygen prevents hypoxia during endoscopic cholangiopancreatography. Gastrointest Endosc. 1992; 38:418–420.54. Zuccaro G, Radaelli F, Vargo J, et al. Routine use of supplemental oxygen prevents recognition of prolonged apnea during endoscopy. Gastrointest Endosc. 2000; 51:AB141.55. Griffin SM, Chung SC, Leung JW, Li AK. Effect of intranasal oxygen on hypoxia and tachycardia during endoscopic cholangiopancreatography. BMJ. 1990; 300:83–84.56. Gross JB, Long WB. Nasal oxygen alleviates hypoxemia in colonoscopy patients sedated with midazolam and meperidine. Gastrointest Endosc. 1990; 36:26–29.57. Haines DJ, Bibbey D, Green JR. Does nasal oxygen reduce the cardiorespiratory problems experienced by elderly patients undergoing endoscopic retrograde cholangiopancreatography? Gut. 1992; 33:973–975.58. Iwao T, Toyonaga A, Shigemori H, Sumino M, Oho K, Tanikawa K. Supplemental oxygen during endoscopic variceal ligation: effects on arterial oxygenation and cardiac arrhythmia. Am J Gastroenterol. 1995; 90:2186–2190.59. Jurell KR, O’Connor KW, Slack J, et al. Effect of supplemental oxygen on cardiopulmonary changes during gastrointestinal endoscopy. Gastrointest Endosc. 1994; 40:665–670.60. Kim H, Hyun JN, Lee KJ, Kim HS, Park HJ. Oxygenation before endoscopic sedation reduces the hypoxic event during endoscopy in elderly patients: a randomized controlled trial. J Clin Med. 2020; 9:3282.61. Patterson KW, Noonan N, Keeling NW, Kirkham R, Hogan DF. Hypoxemia during outpatient gastrointestinal endoscopy: the effects of sedation and supplemental oxygen. J Clin Anesth. 1995; 7:136–140.62. Rozario L, Sloper D, Sheridan MJ. Supplemental oxygen during moderate sedation and the occurrence of clinically significant desaturation during endoscopic procedures. Gastroenterol Nurs. 2008; 31:281–285.63. Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy, Lichtenstein DR, Jagannath S, et al. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008; 68:815–826.64. American Society of Anesthesiologists Task Force on sedation and analgesia by non-anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002; 96:1004–1017.65. ASGE Ensuring Safety in the Gastrointestinal Endoscopy Unit Task Force, Calderwood AH, Chapman FJ, et al. Guidelines for safety in the gastrointestinal endoscopy unit. Gastrointest Endosc. 2014; 79:363–372.66. Cohen LB, Delegge MH, Aisenberg J, et al. AGA Institute review of endoscopic sedation. Gastroenterology. 2007; 133:675–701.67. Waring JP, Baron TH, Hirota WK, et al. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. Gastrointest Endosc. 2003; 58:317–322.68. Maurer WG, Walsh M, Viazis N. Basic requirements for monitoring sedated patients: blood pressure, pulse oximetry, and EKG. Digestion. 2010; 82:87–89.69. Lucendo AJ, González-Huix F, Tenias JM, et al. Gastrointestinal endoscopy sedation and monitoring practices in Spain: a nationwide survey in the year 2014. Endoscopy. 2015; 47:383–390.70. Riphaus A, Rabofski M, Wehrmann T. Endoscopic sedation and monitoring practice in Germany: results from the first nationwide survey. Z Gastroenterol. 2010; 48:392–397.71. Willey J, Vargo JJ, Connor JT, Dumot JA, Conwell DL, Zuccaro G. Quantitative assessment of psychomotor recovery after sedation and analgesia for outpatient EGD. Gastrointest Endosc. 2002; 56:810–816.72. Aldrete JA. Modifications to the postanesthesia score for use in ambulatory surgery. J Perianesth Nurs. 1998; 13:148–155.73. Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970; 49:924–934.74. Chung F. Are discharge criteria changing? J Clin Anesth. 1993; 5(Suppl 1):64S–68S.75. Chung F, Chan VW, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth. 1995; 7:500–506.76. Amornyotin S, Chalayonnavin W, Kongphlay S. Recovery pattern and home-readiness after ambulatory gastrointestinal endoscopy. J Med Assoc Thai. 2007; 90:2352–2358.77. Trevisani L, Cifalà V, Gilli G, Matarese V, Zelante A, Sartori S. Post-anaesthetic discharge scoring system to assess patient recovery and discharge after colonoscopy. World J Gastrointest Endosc. 2013; 5:502–507.78. Gurunathan U, Rahman T, Williams Z, et al. Effect of midazolam in addition to propofol and opiate sedation on the quality of recovery after colonoscopy: a randomized clinical trial. Anesth Analg. 2020; 131:741–750.79. Thompson R, Seck V, Riordan S, Wong S. Comparison of the effects of midazolam/fentanyl, midazolam/propofol, and midazolam/fentanyl/ propofol on cognitive function after gastrointestinal endoscopy. Surg Laparosc Endosc Percutan Tech. 2019; 29:441–446.80. Zhang K, Xu H, Li HT. Safety and efficacy of propofol alone or in combination with other agents for sedation of patients undergoing colonoscopy: an updated meta-analysis. Eur Rev Med Pharmacol Sci. 2020; 24:4506–4518.81. Hsu YH, Lin FS, Yang CC, Lin CP, Hua MS, Sun WZ. Evident cognitive impairments in seemingly recovered patients after midazolam-based light sedation during diagnostic endoscopy. J Formos Med Assoc. 2015; 114:489–497.82. Horiuchi A, Nakayama Y, Hidaka N, Ichise Y, Kajiyama M, Tanaka N. Low-dose propofol sedation for diagnostic esophagogastroduodenoscopy: results in 10,662 adults. Am J Gastroenterol. 2009; 104:1650–1655.83. Horiuchi A, Nakayama Y, Fujii H, Katsuyama Y, Ohmori S, Tanaka N. Psychomotor recovery and blood propofol level in colonoscopy when using propofol sedation. Gastrointest Endosc. 2012; 75:506–512.84. Horiuchi A, Nakayama Y, Kajiyama M, et al. Safety and effectiveness of propofol sedation during and after outpatient colonoscopy. World J Gastroenterol. 2012; 18:3420–3425.85. Watkins TJ, Bonds RL, Hodges K, Goettle BB, Dobson DAM, Maye JP. Evaluation of postprocedure cognitive function using 3 distinct standard sedation regimens for endoscopic procedures. AANA J. 2014; 82:133–139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sedation Regimens for Gastrointestinal Endoscopy
- Considerable Variability of Procedural Sedation and Analgesia Practices for Gastrointestinal Endoscopic Procedures in Europe
- Endoscopic Sedation: From Training to Performance
- Management of antithrombotic agents for gastrointestinal endoscopy
- A Nationwide Survey on the Facilities and Personnel for Endoscopic Sedation: Results from 50 Qualified Endoscopy Units of Teaching Hospitals Accredited by the Korean Society of Gastrointestinal Endoscopy (KSGE)