Blood Res.
2022 Mar;57(1):51-58. 10.5045/br.2021.2021176.
Real-world evidence of levofloxacin prophylaxis in elderly patients with newly diagnosed multiple myeloma who received bortezomib, melphalan, and prednisone regimen
- Affiliations
-
- 1Department of Hematology-Oncology, Chonnam National University Hwasun Hospital and Chonnam National University Medical School, Hwasun, Korea
- 2Department of Internal Medicine, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea
- 3Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- KMID: 2527497
- DOI: http://doi.org/10.5045/br.2021.2021176
Abstract
- Background
Although survival outcomes of multiple myeloma (MM) have improved with the development of new and effective agents, infection remains the major cause of morbidity and mortality. Here, we evaluated the efficacy of levofloxacin prophylaxis (in a real-world setting) during bortezomib, melphalan, and prednisone (VMP) therapy in elderly patients with newly diagnosed MM.
Methods
This study retrospectively analyzed the records of patients with newly diagnosed MM treated with the VMP regimen between February 2011 and September 2020 at three institutes of the Republic of Korea.
Results
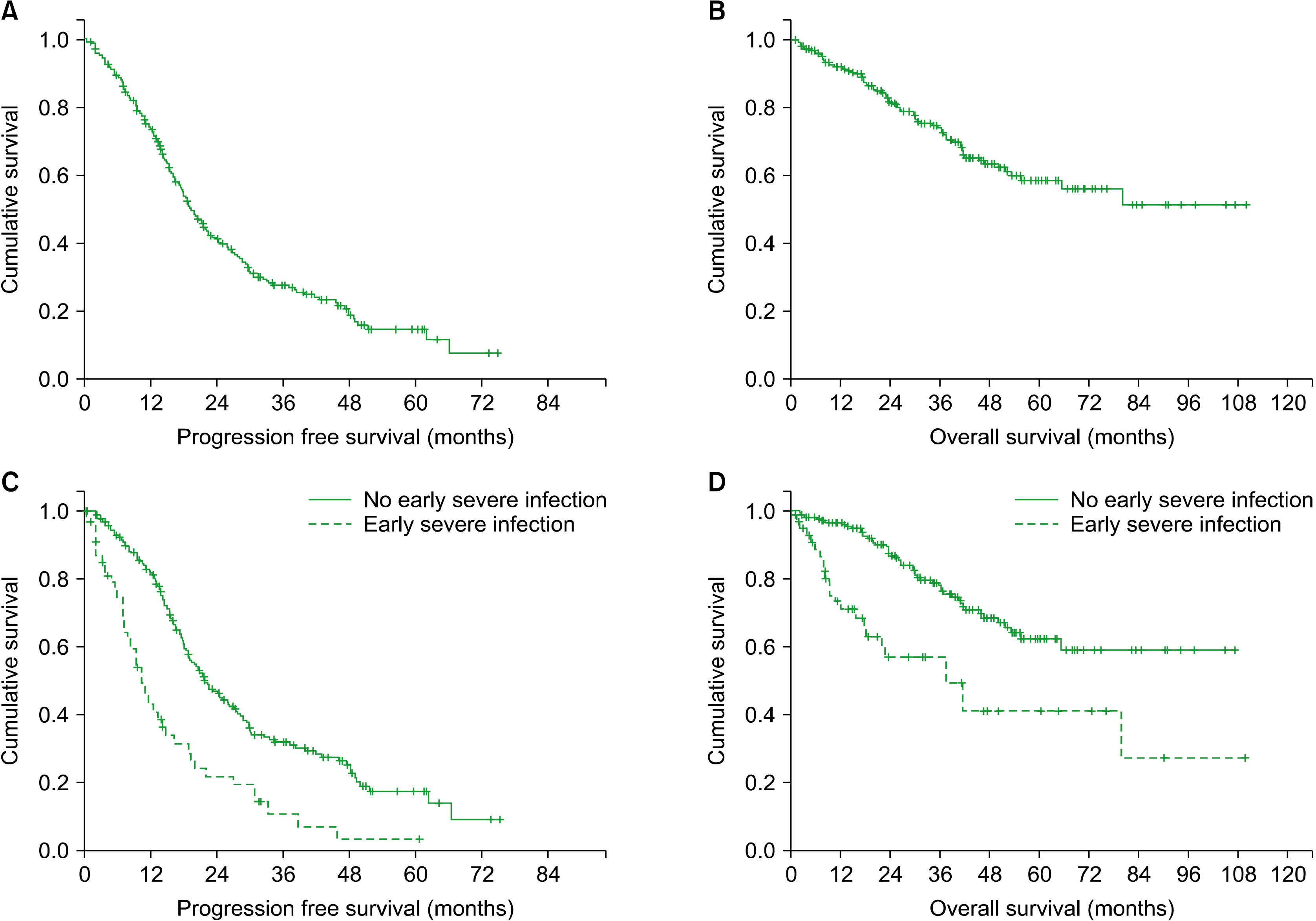
Of a total of 258 patients, 204 (79.1%) received levofloxacin prophylaxis during VMP therapy. The median number of levofloxacin prophylaxis cycles was 4 (range, 1‒9), but 10 patients did not complete the planned prophylaxis because of side effects. Sixty-six patients (25.5%) experienced severe infections during VMP therapy, most of which (74.7%) occurred within the first four cycles of VMP therapy regardless of levofloxacin prophylaxis status. Early severe infection was significantly associated with poor survival. In multivariate analysis, levofloxacin prophylaxis was significantly associated with a lower risk in early severe infection.
Conclusion
Our findings suggest that levofloxacin prophylaxis should be considered at least during the first four cycles of VMP therapy in elderly patients with newly diagnosed MM.
Keyword
Figure
Reference
-
1. Kyle RA, Rajkumar SV. 2008; Multiple myeloma. Blood. 111:2962–72. DOI: 10.1182/blood-2007-10-078022. PMID: 18332230. PMCID: PMC2265446.
Article2. Siegel RL, Miller KD, Fuchs HE, Jemal A. 2021; Cancer statistics, 2021. CA Cancer J Clin. 71:7–33. DOI: 10.3322/caac.21654. PMID: 33433946.
Article3. Kristinsson SY, Landgren O, Dickman PW, Derolf AR, Björkholm M. 2007; Patterns of survival in multiple myeloma: a population-based study of patients diagnosed in Sweden from 1973 to 2003. J Clin Oncol. 25:1993–9. DOI: 10.1200/JCO.2006.09.0100. PMID: 17420512.
Article4. Kumar SK, Rajkumar SV, Dispenzieri A, et al. 2008; Improved survival in multiple myeloma and the impact of novel therapies. Blood. 111:2516–20. DOI: 10.1182/blood-2007-10-116129. PMID: 17975015. PMCID: PMC2254544.
Article5. Kumar SK, Dispenzieri A, Lacy MQ, et al. 2014; Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia. 28:1122–8. DOI: 10.1038/leu.2013.313. PMID: 24157580. PMCID: PMC4000285.
Article6. Backhaus E, Berg S, Andersson R, et al. 2016; Epidemiology of invasive pneumococcal infections: manifestations, incidence and case fatality rate correlated to age, gender and risk factors. BMC Infect Dis. 16:367. DOI: 10.1186/s12879-016-1648-2. PMID: 27487784. PMCID: PMC4972955.
Article7. Mills KH, Cawley JC. 1983; Abnormal monoclonal antibody-defined helper/suppressor T-cell subpopulations in multiple myeloma: relationship to treatment and clinical stage. Br J Haematol. 53:271–5. DOI: 10.1111/j.1365-2141.1983.tb02021.x. PMID: 6217831.
Article8. Schütt P, Brandhorst D, Stellberg W, et al. 2006; Immune parameters in multiple myeloma patients: influence of treatment and correlation with opportunistic infections. Leuk Lymphoma. 47:1570–82. DOI: 10.1080/10428190500472503. PMID: 16966269.
Article9. Frassanito MA, Cusmai A, Dammacco F. 2001; Deregulated cytokine network and defective Th1 immune response in multiple myeloma. Clin Exp Immunol. 125:190–7. DOI: 10.1046/j.1365-2249.2001.01582.x. PMID: 11529908. PMCID: PMC1906126.
Article10. Gavazzi G, Krause KH. 2002; Ageing and infection. Lancet Infect Dis. 2:659–66. DOI: 10.1016/S1473-3099(02)00437-1. PMID: 12409046.
Article11. Nucci M, Anaissie E. 2009; Infections in patients with multiple myeloma in the era of high-dose therapy and novel agents. Clin Infect Dis. 49:1211–25. DOI: 10.1086/605664. PMID: 19769539.
Article12. Blimark C, Holmberg E, Mellqvist UH, et al. 2015; Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 100:107–13. DOI: 10.3324/haematol.2014.107714. PMID: 25344526. PMCID: PMC4281323.
Article13. Jung SH, Cho MS, Kim HK, et al. 2016; Risk factors associated with early mortality in patients with multiple myeloma who were treated upfront with a novel agents containing regimen. BMC Cancer. 16:613. DOI: 10.1186/s12885-016-2645-y. PMID: 27501959. PMCID: PMC4977683.
Article14. Charlson M, Szatrowski TP, Peterson J, Gold J. 1994; Validation of a combined comorbidity index. J Clin Epidemiol. 47:1245–51. DOI: 10.1016/0895-4356(94)90129-5. PMID: 7722560.
Article15. Kumar S, Paiva B, Anderson KC, et al. 2016; International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 7:e328–46. DOI: 10.1016/S1470-2045(16)30206-6. PMID: 27511158.16. Dumontet C, Hulin C, Dimopoulos MA, et al. 2018; A predictive model for risk of early grade ≥ 3 infection in patients with multiple myeloma not eligible for transplant: analysis of the FIRST trial. Leukemia. 32:1404–13. DOI: 10.1038/s41375-018-0133-x. PMID: 29784907. PMCID: PMC5990520.
Article17. Vesole DH, Oken MM, Heckler C, et al. 2012; Oral antibiotic prophylaxis of early infection in multiple myeloma: a URCC/ECOG randomized phase III study. Leukemia. 26:2517–20. DOI: 10.1038/leu.2012.124. PMID: 22678167. PMCID: PMC4734137.
Article18. Smilack JD. 1999; Trimethoprim-sulfamethoxazole. Mayo Clin Proc. 74:730–4. DOI: 10.4065/74.7.730. PMID: 10405706.
Article19. Zhanel GG, Karlowsky JA, Harding GK, et al. 2000; A Canadian national surveillance study of urinary tract isolates from outpatients: comparison of the activities of trimethoprim-sulfamethoxazole, ampicillin, mecillinam, nitrofurantoin, and ciprofloxacin. The Canadian Urinary Isolate Study Group. Antimicrob Agents Chemother. 44:1089–92. DOI: 10.1128/AAC.44.4.1089-1092.2000. PMID: 10722520. PMCID: PMC89821.
Article20. Drayson MT, Bowcock S, Planche T, et al. 2019; Levofloxacin prophylaxis in patients with newly diagnosed myeloma (TEAMM): a multicentre, double-blind, placebo-controlled, randomised, phase 3 trial. Lancet Oncol. 20:1760–72. DOI: 10.1016/S1470-2045(19)30506-6. PMID: 31668592. PMCID: PMC6891230.
Article21. Iuliano AD, Roguski KM, Chang HH, et al. 2018; Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 391:1285–300. DOI: 10.1016/S0140-6736(17)33293-2. PMID: 29248255. PMCID: PMC5935243.22. Jung SH, Bae SY, Ahn JS, et al. 2013; Lymphocytopenia is associated with an increased risk of severe infections in patients with multiple myeloma treated with bortezomib-based regimens. Int J Hematol. 97:382–7. DOI: 10.1007/s12185-013-1270-7. PMID: 23355264.
Article23. Soekojo CY, Low JZ, Oh J, Ooi M, De Mel S, Chng WJ. 2020; Bacterial infection among patients with multiple myeloma treated with bortezomib-based induction therapy: real-world experience in an Asian Cancer Center. Clin Lymphoma Myeloma Leuk. 20:e165–70. DOI: 10.1016/j.clml.2019.12.024. PMID: 32019731.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bortezomib and melphalan as a conditioning regimen for autologous stem cell transplantation in multiple myeloma
- Modified dose of melphalan-prednisone in multiple myeloma patients receiving bortezomib plus melphalan-prednisone treatment
- Chemotherapy adherence is a favorable prognostic factor for elderly patients with multiple myeloma who are treated with a frontline bortezomib-containing regimen
- Combination chemotherapy with vincristine, melphalan and prednisone for multiple myeloma
- Effect of Cyclophosphamide and Prednisone as a First-line Treatment for Non-transplant Candidates with Multiple Myeloma