Neonatal Med.
2022 Feb;29(1):10-17. 10.5385/nm.2022.29.1.10.
Implementing the Golden Hour Protocol to Improve the Clinical Outcomes in Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Pusan National University Children’s Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2Department of Pediatrics, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- KMID: 2527256
- DOI: http://doi.org/10.5385/nm.2022.29.1.10
Abstract
- Purpose
Since premature infants are sensitive to the changes in blood glucose levels and body temperature, maintaining these parameters is important to avoid the risk of infections. The authors implemented the Golden Hour protocol (GHP) that aims to close the final incubator within one hour of birth by implementing early treatment steps for premature infants after birth, such as maintaining body temperature, securing airway, and rapidly administering glucose fluid and prophylactic antibiotics by securing breathing and rapid blood vessels. This study investigated the effect of GHP application on the short- and long-term clinical outcomes.
Methods
We retrospectively analyzed the medical records between 2017 and 2018 before GHP application and between 2019 and 2020 after GHP application in preterm infants aged 24 weeks or older and those aged less than 33 weeks who were admitted to the neonatal intensive care unit.
Results
Overall, 117 GHP patients and 81 patients without GHP were compared and analyzed. Peripheral vascularization time and prophylactic antibiotic administration time were shortened in the GHP-treated group (P=0.007 and P=0.008). In the short-term results, the GHP-treated group showed reduced hypothermia upon arrival at the neonatal intensive care unit (P=0.002), and the blood glucose level at 1 hour of hospitalization was higher (P=0.012). Furthermore, the incidence of neonatal necrotizing enteritis decreased (P=0.043). As a long-term result, the incidence of BPD was reduced (P=0.004).
Conclusion
We confirmed that applying GHP improved short- and long-term clinical outcomes in premature infants aged <33 weeks age of gestation, and we expect to improve the treatment quality by actively using it for postnatal treatment.
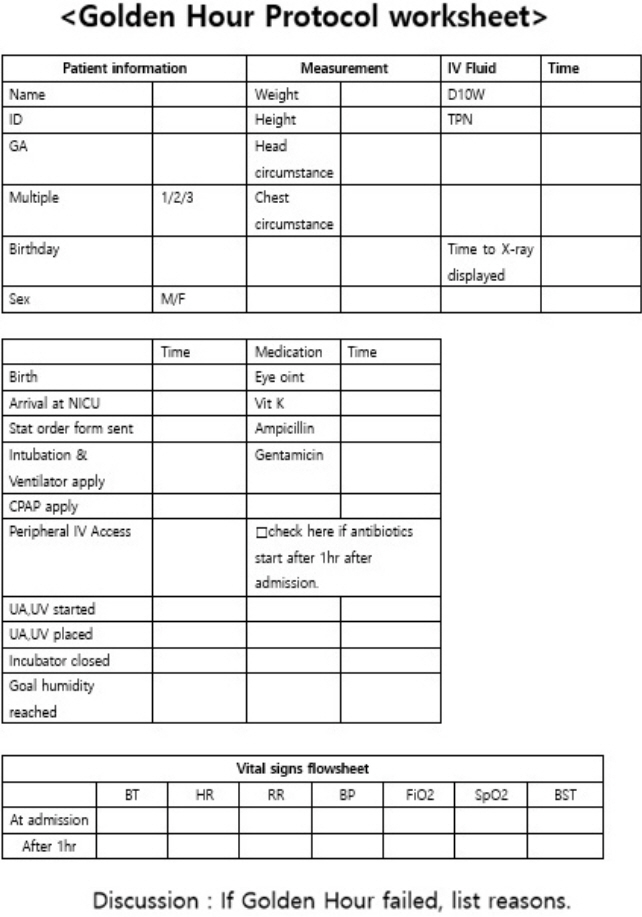
Figure
Reference
-
1. Gleason CA, Juul SE. Avery's diseases of the newborn. 10th ed. Philadelphia: Elsevier Inc.;2018. p. 390–404.2. Itabashi K, Miyazawa T, Kusuda S, Wada K; Japan Pediatric Society Newborn Committee. Changes in mortality rates among extremely preterm infants born before 25 weeks' gestation: comparison between the 2005 and 2010 nationwide surveys in Japan. Early Hum Dev. 2021; 155:105321.3. Zhu Z, Yuan L, Wang J, Li Q, Yang C, Gao X, et al. Mortality and morbidity of infants born extremely preterm at tertiary medical centers in China from 2010 to 2019. JAMA Netw Open. 2021; 4:e219382.4. Cloherty JP, Eichenwald EC, Hansen AR, Stark AR. Manual of neonatal care. 7th ed. Philadelphia: Lippincott Williams & Wilkins;2015. p. 35–9.5. Cowley RA, Hudson F, Scanlan E, Gill W, Lally RJ, Long W, et al. An economical and proved helicopter program for transporting the emergency critically ill and injured patient in Maryland. J Trauma. 1973; 13:1029–38.6. Reynolds RD, Pilcher J, Ring A, Johnson R, McKinley P. The Golden Hour: care of the LBW infant during the first hour of life one unit's experience. Neonatal Netw. 2009; 28:211–9.7. Vento M, Cheung PY, Aguar M. The first golden minutes of the extremely-low-gestational-age neonate: a gentle approach. Neonatology. 2009; 95:286–98.8. Annibale DJ, Bissinger RL. The golden hour. Adv Neonatal Care. 2010; 10:221–3.9. Castrodale V, Rinehart S. The golden hour: improving the stabilization of the very low birth-weight infant. Adv Neonatal Care. 2014; 14:9–14.10. Reuter S, Messier S, Steven D. The neonatal Golden Hour: intervention to improve quality of care of the extremely low birth weight infant. S D Med. 2014; 67:397–405.11. Lambeth TM, Rojas MA, Holmes AP, Dail RB. First Golden Hour of life: a quality improvement initiative. Adv Neonatal Care. 2016; 16:264–72.12. Sharma D. Golden hour of neonatal life: need of the hour. Matern Health Neonatol Perinatol. 2017; 3:16.13. Sharma D. Golden 60minutes of newborn's life: part 1. Preterm neonate. J Matern Fetal Neonatal Med. 2017; 30:2716–27.14. Sharma D, Sharma P, Shastri S. Golden 60minutes of newborn's life: part 2. Term neonate. J Matern Fetal Neonatal Med. 2017; 30:2728–33.15. Harriman TL, Carter B, Dail RB, Stowell KE, Zukowsky K. Golden hour protocol for preterm infants: a quality improvement project. Adv Neonatal Care. 2018; 18:462–70.16. Peleg B, Globus O, Granot M, Leibovitch L, Mazkereth R, Eisen I, et al. "Golden Hour" quality improvement intervention and short-term outcome among preterm infants. J Perinatol. 2019; 39:387–92.17. Bhatt DR, White R, Martin G, Van Marter LJ, Finer N, Goldsmith JP, et al. Transitional hypothermia in preterm newborns. J Perinatol. 2007; 27 Suppl 2:S45–7.18. Boo NY, Guat-Sim Cheah I; Malaysian National Neonatal Registry. Admission hypothermia among VLBW infants in Malaysian NICUs. J Trop Pediatr. 2013; 59:447–52.19. Hazan J, Maag U, Chessex P. Association between hypothermia and mortality rate of premature infants: revisited. Am J Obstet Gynecol. 1991; 164(1 Pt 1):111–2.20. Wang H, Liddell CA, Coates MM, Mooney MD, Levitz CE, Schumacher AE, et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384:957–79.21. Polin RA; Committee on Fetus and Newborn. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics. 2012; 129:1006–15.22. Shane AL, Sanchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017; 390:1770–80.23. Ford H, Watkins S, Reblock K, Rowe M. The role of inflammatory cytokines and nitric oxide in the pathogenesis of necrotizing enterocolitis. J Pediatr Surg. 1997; 32:275–82.24. Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005; 115:696–703.25. Prado C, Michels M, Avila P, Burger H, Milioli M, Dal-Pizzol F. The protective effects of fecal microbiota transplantation in an experimental model of necrotizing enterocolitis. J Pediatr Surg. 2019; 54:1578–83.26. Tudehope DI. The epidemiology and pathogenesis of neonatal necrotizing enterocolitis. J Paediatr Child Health. 2005; 41:167–8.27. Berger TM, Bachmann II, Adams M, Schubiger G. Impact of improved survival of very low-birth-weight infants on incidence and severity of bronchopulmonary dysplasia. Biol Neonate. 2004; 86:124–30.28. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–9.29. Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics. 2000; 105:1194–201.30. McGrath JM. Is evidence-based practice routine in the golden hour? J Perinat Neonatal Nurs. 2012; 26:109–11.31. Wallingford B, Rubarth L, Abbott A, Miers LJ. Implementation and evaluation of “golden hour” practices in infants younger than 33 weeks' gestation. Newborn Infant Nurs Rev. 2012; 12:86–96.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurodevelopmental outcomes of preterm infants
- Evaluation and Management of Main Bacterial Infections in Premature Infants
- Neonatal outcomes of very low birthweight infants from spontaneous and indicated preterm delivery
- Growth patterns of preterm infants in Korea
- Clinical Trials for Preterm Infants' Neurodevelopment to the Norm: Erythropoietin and Nutritional Interventions