J Korean Foot Ankle Soc.
2022 Mar;26(1):22-29. 10.14193/jkfas.2022.26.1.22.
Current Trends in the Treatment of Ankle Ligament Injuries: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungbuk National University Hospital, Cheongju, Korea
- 2Department of Orthopedic Surgery, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea
- 3Department of Orthopedic Surgery, College of Medicine, Dong-A University, Busan, Korea
- 4Department of Orthopedic Surgery, Chosun University Hospital, Gwangju, Korea
- 5Department of Orthopedic Surgery, Inje University Sanggye Paik Hospital, Seoul, Korea
- KMID: 2527008
- DOI: http://doi.org/10.14193/jkfas.2022.26.1.22
Abstract
- Purpose
Despite continuous updates of standard treatment guidelines for acute ankle sprain and chronic ankle instability (CAI), in practice preferred treatment protocols vary widely. Based on a Korean Foot and Ankle Society (KFAS) member survey, this study reports current trends in the management of ankle ligament injuries.
Materials and Methods
A web-based questionnaire containing 34 questions was sent to all KFAS members in September 2021. Questions mainly addressed clinical experience and preferences for the diagnosis and treatment of ankle ligament injuries. Answers with a prevalence of ≥50% among respondents were considered to reflect tendencies.
Results
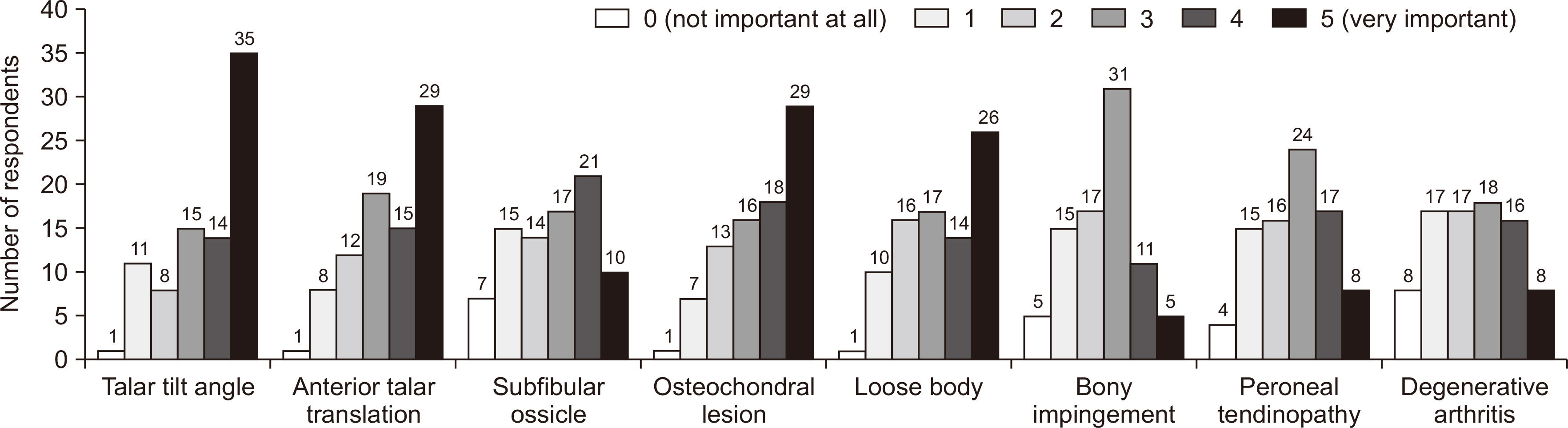
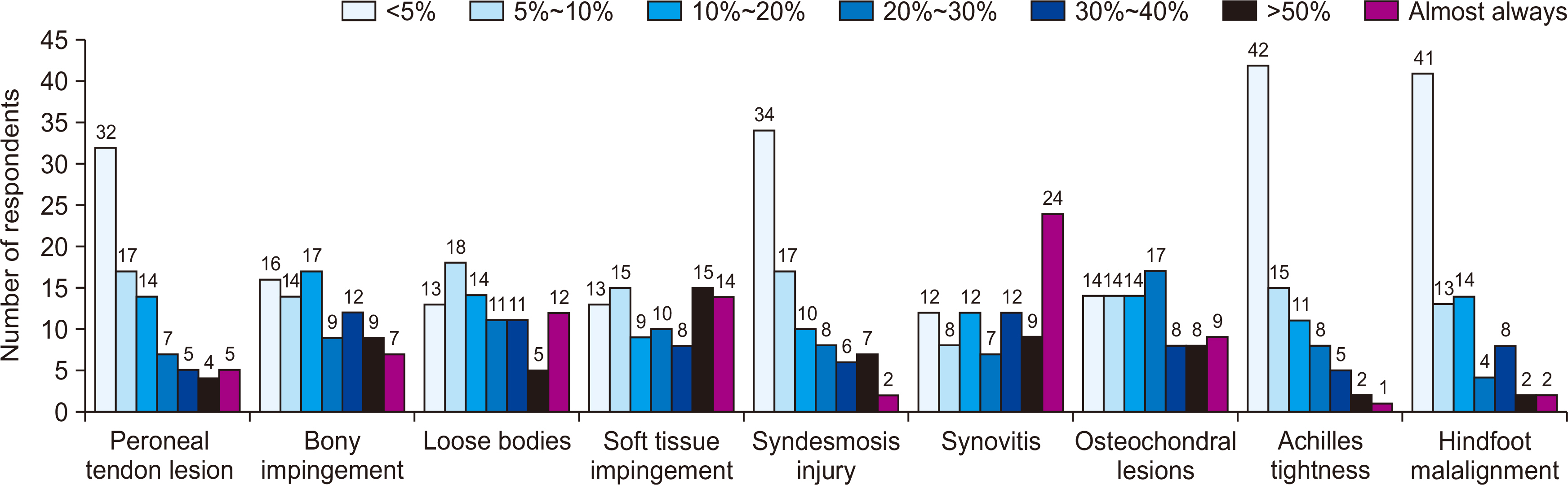
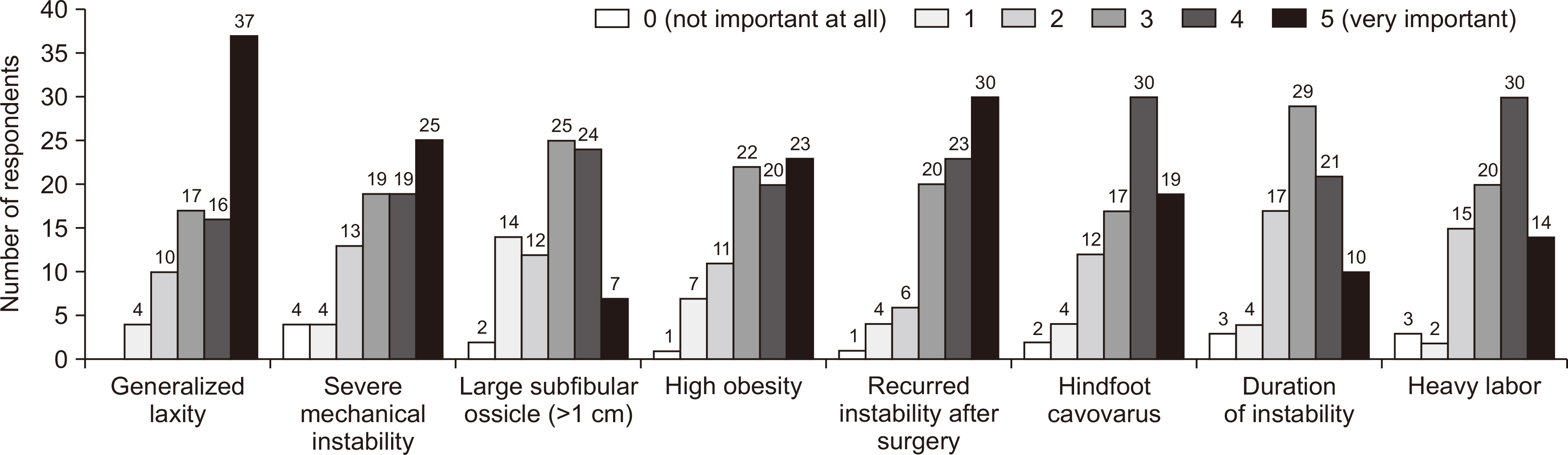
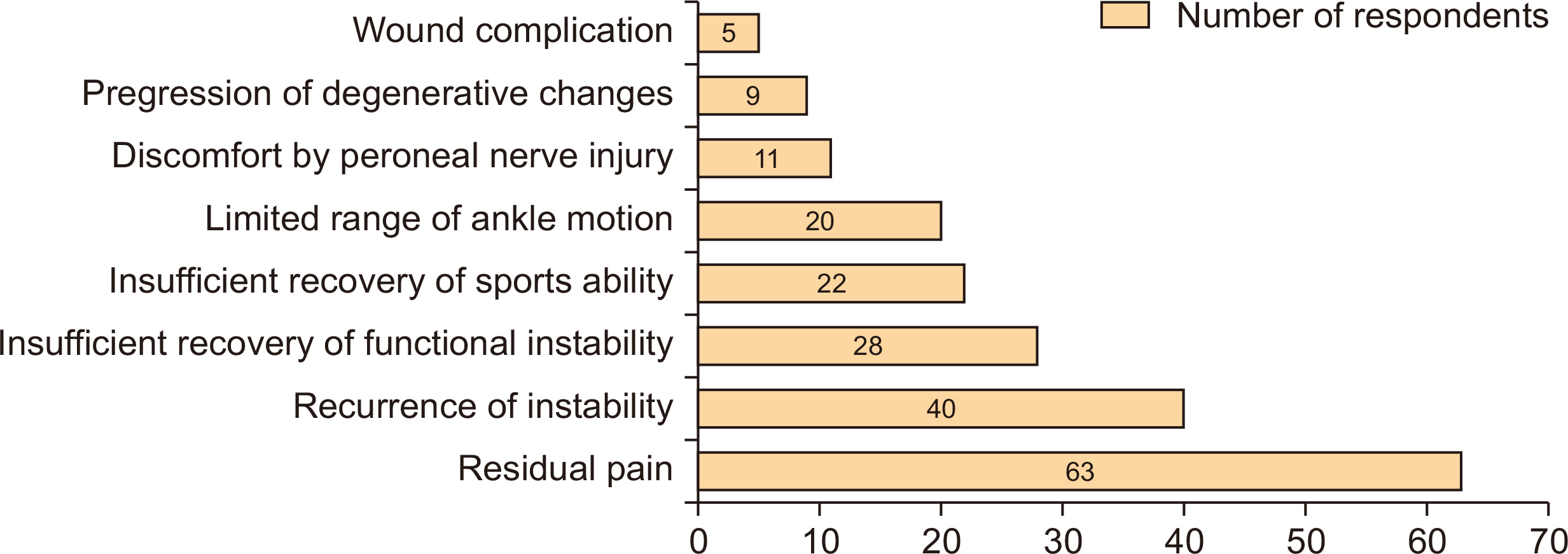
Eighty-four of the 550 members (15.3%) responded. Answers that showed a tendency were as follows: commonest additional image study (ultrasound), conservative treatment modality (immobilization, oral medication), frequency of surgical treatment (<5 cases per annum), most important factor when deciding on surgical treatment (activity level, e.g., occupation or sport), and commonest surgical procedure (open ligament repair). Answers that showed a tendency for CAI were as follows: most important symptom (repeated sprain, giving way), radiological factors (talar tilt, osteochondral lesion, anterior talar translation), and patient factors (occupation, sports activities, recurrent instability after surgery, etc.). For decision making regarding surgical treatment and method, the most preferred surgical procedure was the modified Broström procedure, and the most common repair technique was suture anchor technique. The following were considered poor prognostic factors; generalized laxity, failed previous surgery, cavovarus, severe mechanical instability, heavy work, obesity, and dissatisfaction after surgery because of residual pain.
Conclusion
This study updates information regarding current trends in the management of ankle ligament injuries in Korea, and reveals consensus opinions and variations in approaches to patients with an acute or chronic injury. The divergence of approaches identified indicates the need for further studies to determine standard guidelines and long-term results.
Figure
Reference
-
1. van den Bekerom MP, Kerkhoffs GM, McCollum GA, Calder JD, van Dijk CN. 2013; Management of acute lateral ankle ligament injury in the athlete. Knee Surg Sports Traumatol Arthrosc. 21:1390–5. doi: 10.1007/s00167-012-2252-7. DOI: 10.1007/s00167-012-2252-7. PMID: 23108678.
Article2. DiGiovanni CW, Brodsky A. 2006; Current concepts: lateral ankle instability. Foot Ankle Int. 27:854–66. doi: 10.1177/107110070602701019. DOI: 10.1177/107110070602701019. PMID: 17054892.
Article3. Hubbard TJ. 2008; Ligament laxity following inversion injury with and without chronic ankle instability. Foot Ankle Int. 29:305–11. doi: 10.3113/FAI.2008.0305. DOI: 10.3113/FAI.2008.0305. PMID: 18348827.
Article4. Baumhauer JF, O'Brien T. 2002; Surgical considerations in the treatment of ankle instability. J Athl Train. 37:458–62. PMID: 12937567. PMCID: PMC164377.5. Cho BK, Kim YM, Choi SM, Park HW, SooHoo NF. Revision anatomical reconstruction of the lateral ligaments of the ankle augmented with suture tape for patients with a failed Broström procedure. Bone Joint J. 2017; 99-B:1183–9. doi: 10.1302/0301-620X.99B9.BJJ-2017-0144.R1. DOI: 10.1302/0301-620X.99B9.BJJ-2017-0144.R1. PMID: 28860398.
Article6. Coetzee JC, Ellington JK, Ronan JA, Stone RM. 2018; Functional results of open Broström ankle ligament repair augmented with a suture tape. Foot Ankle Int. 39:304–10. doi: 10.1177/1071100717742363. DOI: 10.1177/1071100717742363. PMID: 29420055.
Article7. Kang HJ, Jung HG. 2018; Indications of lateral ankle ligament reconstruction with a free tendon and associated evidence. J Korean Foot Ankle Soc. 22:91–4. doi: 10.14193/jkfas.2018.22.3.91. DOI: 10.14193/jkfas.2018.22.3.91.
Article8. Guelfi M, Zamperetti M, Pantalone A, Usuelli FG, Salini V, Oliva XM. 2018; Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: a systematic review. Foot Ankle Surg. 24:11–8. doi: 10.1016/j.fas.2016.05.315. DOI: 10.1016/j.fas.2016.05.315. PMID: 29413768.
Article9. Pihlajamäki H, Hietaniemi K, Paavola M, Visuri T, Mattila VM. 2010; Surgical versus functional treatment for acute ruptures of the lateral ligament complex of the ankle in young men: a randomized controlled trial. J Bone Joint Surg Am. 92:2367–74. doi: 10.2106/JBJS.I.01176. DOI: 10.2106/JBJS.I.01176. PMID: 20833874.10. Pijnenburg AC, Bogaard K, Krips R, Marti RK, Bossuyt PM, van Dijk CN. 2003; Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomised, prospective trial. J Bone Joint Surg Br. 85:525–30. doi: 10.1302/0301-620X.85B4.13928. DOI: 10.1302/0301-620X.85B4.13928. PMID: 12793557.11. Pijnenburg AC, van Dijk CN, Bossuyt PM, Marti RK. 2000; Treatment of ruptures of the lateral ankle ligaments: a meta-analysis. J Bone Joint Surg Am. 82:761–73. doi: 10.2106/00004623-200006000-00002. DOI: 10.2106/00004623-200006000-00002. PMID: 10859095.
Article12. Povacz P, Unger SF, Miller WK, Tockner R, Resch H. 1998; A randomized, prospective study of operative and non-operative treatment of injuries of the fibular collateral ligaments of the ankle. J Bone Joint Surg Am. 80:345–51. doi: 10.2106/00004623-199803000-00006. DOI: 10.2106/00004623-199803000-00006. PMID: 9531201.
Article13. Cho BK. 2018; Evidence-based treatment of acute lateral ankle sprain. J Korean Foot Ankle Soc. 22:135–44. doi: 10.14193/jkfas.2018.22.4.135. DOI: 10.14193/jkfas.2018.22.4.135.
Article14. Feger MA, Glaviano NR, Donovan L, Hart JM, Saliba SA, Park JS, et al. 2017; Current trends in the management of lateral ankle sprain in the United States. Clin J Sport Med. 27:145–52. doi: 10.1097/JSM.0000000000000321. DOI: 10.1097/JSM.0000000000000321. PMID: 27347860.
Article15. Al-Mohrej OA, Al-Kenani NS. 2016; Acute ankle sprain: conservative or surgical approach? EFORT Open Rev. 1:34–44. doi: 10.1302/2058-5241.1.000010. DOI: 10.1302/2058-5241.1.000010. PMID: 28461926. PMCID: PMC5367574.
Article16. Michels F, Pereira H, Calder J, Matricali G, Glazebrook M, Guillo S, et al. 2018; Searching for consensus in the approach to patients with chronic lateral ankle instability: ask the expert. Knee Surg Sports Traumatol Arthrosc. 26:2095–102. doi: 10.1007/s00167-017-4556-0. DOI: 10.1007/s00167-017-4556-0. PMID: 28439639.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Syndesmotic Injury: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Ankle Arthritis: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Acute Achilles Tendon Rupture: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey